The preoperative visit is often the time to establish the anesthesiologist–patient relationship (APR). Frequently patients remember their surgeon but fail to remember who their anesthesiologist was and his/her key role in perioperative care. Using an opinion survey, the aim of this study was to analyze the current perception of outpatients (ASA I and II) about the APR during the immediate postoperative period.
DesignDescriptive cross-sectional multicenter trial including four healthcare institutions between August 2011 and May 2012.
Methods340 surveys were administered to ASA I and II adult subjects scheduled for outpatient surgery, with Aldrette recovery score of 10 prior to discharge.
ResultsOnly 74.1% of the people acknowledged their anesthesiologist as a specialized physician. 21.2% were unaware of the professional training required to become an anesthesiologist and 99% of the patients said that it was gratifying to have the doctor who did the preoperative evaluation in the OR; however this only occurred in 35% of the cases.
ConclusionsNotwithstanding the high level of outpatient satisfaction with their anesthetic care, some strategies are required to strengthen their perception about the specialty. The APR should not be limited to a preoperative evaluation for the surgical procedure, but should be more comprehensive. There is a need to establish closer links with the community to create awareness about the role of the anesthesiologist and his/her outstanding contribution to the patient's care and safety.
La consulta preanestésica es frecuentemente el momento para establecer la relación anestesiólogo-paciente. Es usual que los pacientes recuerden a su cirujano, pero no a su anestesiólogo, o la importancia que este tiene en su cuidado perioperatorio. El objetivo de este trabajo fue analizar la percepción actual de los pacientes ambulatorios (ASA I y II) en el posoperatorio inmediato sobre la relación anestesiólogo-paciente mediante una encuesta de opinión.
DiseñoEstudio descriptivo multicéntrico de corte transversal realizado en 4 instituciones de salud entre agosto de 2011 y mayo de 2012.Métodos: Se aplicaron 340 encuestas a sujetos adultos programados para cirugía ambulatoria, ASA I y II con Aldrette de 10 en recuperación, antes del alta.
ResultadosSolo un 74,1% de las personas reconocía a su anestesiólogo como un médico especialista. El 21,2% desconocía la formación profesional real de este. El 99% de los pacientes refirió como agradable que quien realizó su valoración preoperatoria fuera el mismo que estuviera en su cirugía, pero esta situación se dio solamente en un 35% de los casos.
ConclusionesA pesar de la alta satisfacción de los pacientes ambulatorios sobre su cuidado anestésico, se requieren estrategias para fortalecer la percepción que tienen sobre nuestra especialidad. La relación anestesiólogo-paciente no debería limitarse solamente a la ejecución de la valoración preoperatoria y del procedimiento quirúrgico; adicionalmente deberían incluir espacios que poco se abordan. Es indispensable un mayor acercamiento a la comunidad para dar a conocer el papel del anestesiólogo y su contribución preponderante al cuidado y la seguridad del paciente.
Modern anesthesia requires the anesthesiologist to have a profound medical knowledge to make decisions that are vital in the short term. However, patients know very little about anesthesiologists and there is often a misconception about the specialty, ignoring the anesthetist role and responsibility during surgery. These facts interfere with the APR and hinder the understanding about the expectations and outcomes of the procedure.1–3
The pre-anesthesia visit is an opportunity to establish a positive APR and to clear any doubts about the anesthetic procedure.4 Very often, the doctor who makes the preoperative evaluation is not the same specialist who provides intraoperative anesthesia care or who makes the follow-up after surgery. These situations often result in the patient's failure to identify the name of the anesthesiologist or acknowledging the importance of the anesthesiologist during perioperative care, thinking that the surgeon is the sole care provider and even ignoring anesthesiology as a medical specialty.1,2,4,5
Prior studies in Latin America have shown that about one third of the patients did not know who their anesthesiologist was and only 58–60% acknowledged him/her as a physician. Up to 20% of the patients were unaware of the role or attributions of the anesthetist.4,6 In 1991, a study carried out in Cali, Colombia showed that only 74% of the patients knew who had administered the anesthesia and just 68% acknowledge the anesthesiologist as a medical doctor. 68.5% of the patients were able to identify their surgeon, while only 21% identified their anesthesiologist.7
The purpose of this paper was to establish the current perception of (ASA I and II) outpatients following surgery, with regards to the academic training of their anesthesiologist, his/her role and some aspects of the anesthesiologist–patient relationship.
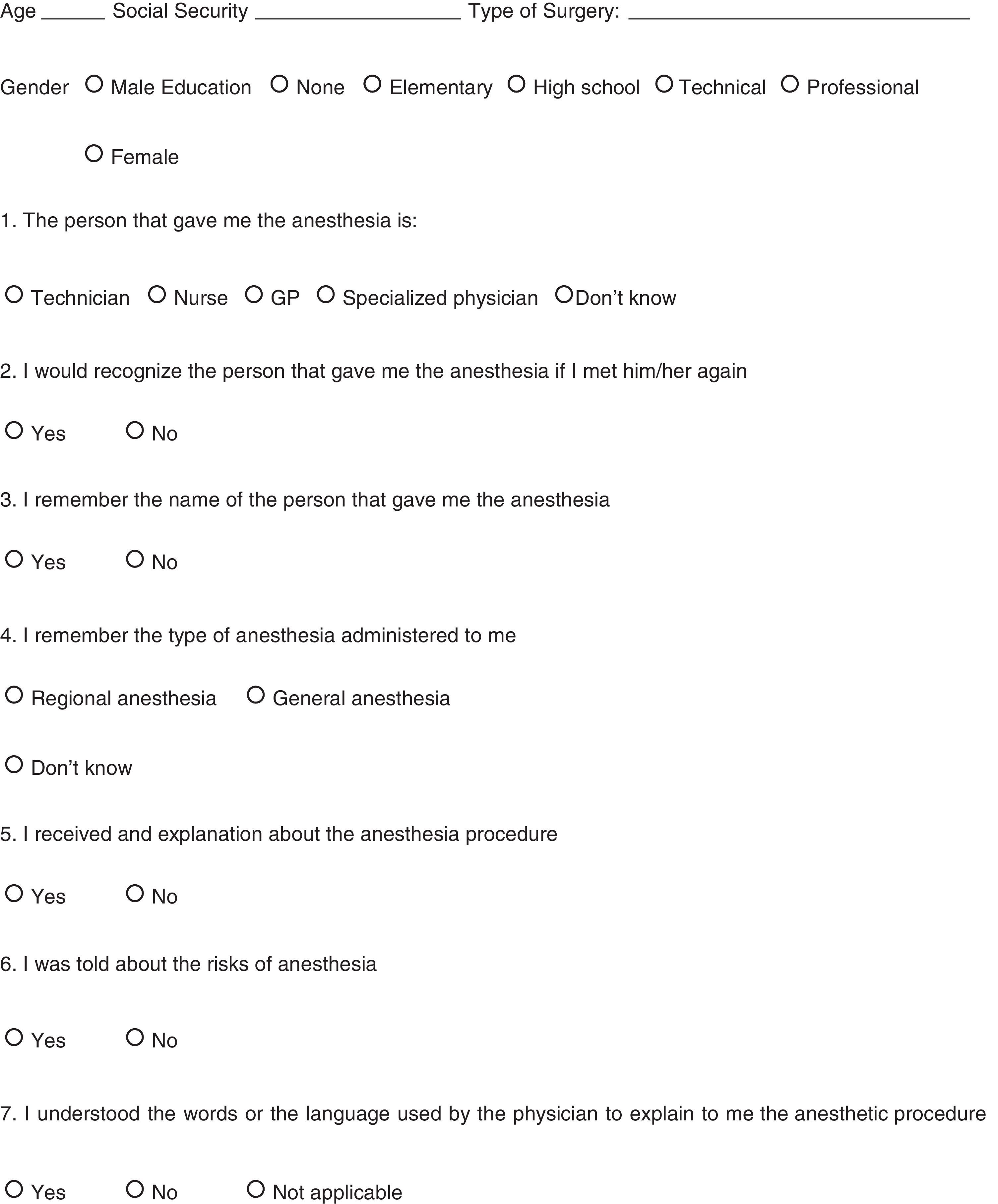
Materials and methodsType of trialThe trial design was descriptive, multicentric, cross-sectional, including four healthcare institutions in the city, from August 2011 to May 2012. A measurement tool was developed to identify the key factors in the APR, according to the patient's perception in the immediate postoperative period.
ScopeFour level III and IV private, semi-private and public healthcare institutions were included: Centro Médico Imbanaco (CMI), Hospital Universitario del Valle (HUV), Fundación Clínica Valle del Lili (FVL) and Sebastián de Belalcázar Clinic that provided care to patients under the various health care modalities.
Trial populationPatients of all races and socio-economic levels who came for ambulatory surgery at the institutions participating in the trial.
Inclusion criteriaAdults ≥18 years of age undergoing ambulatory surgery and classified as ASA I and II with Aldrete recovery score of 10 prior to discharge and who had signed their informed consent to participate the trial.
Exclusion criteriaPatients with a history of psychiatric or psychological conditions; patients who required hospitalization following surgery.
Sample sizeTo calculate the number of patients to be surveyed, a formula for descriptive trials with 95% significance was used. Patient satisfaction was the key outcome variable, using as a reference a previous trial that reported a prevalence of satisfaction of 80%8; the average number of surgical procedures done per month at the participating institutions was considered (CMI: 1000 FVL: 1000 HUV: 1100 Sebastián de Belalcázar: 450). Taking these factors into account, the estimated sample size for the trial was 245 patients. To compensate for any potential losses, the final sample size grew to 340 patients. Subsequently, a sample distribution was made proportional to the number of patients served at each institution.
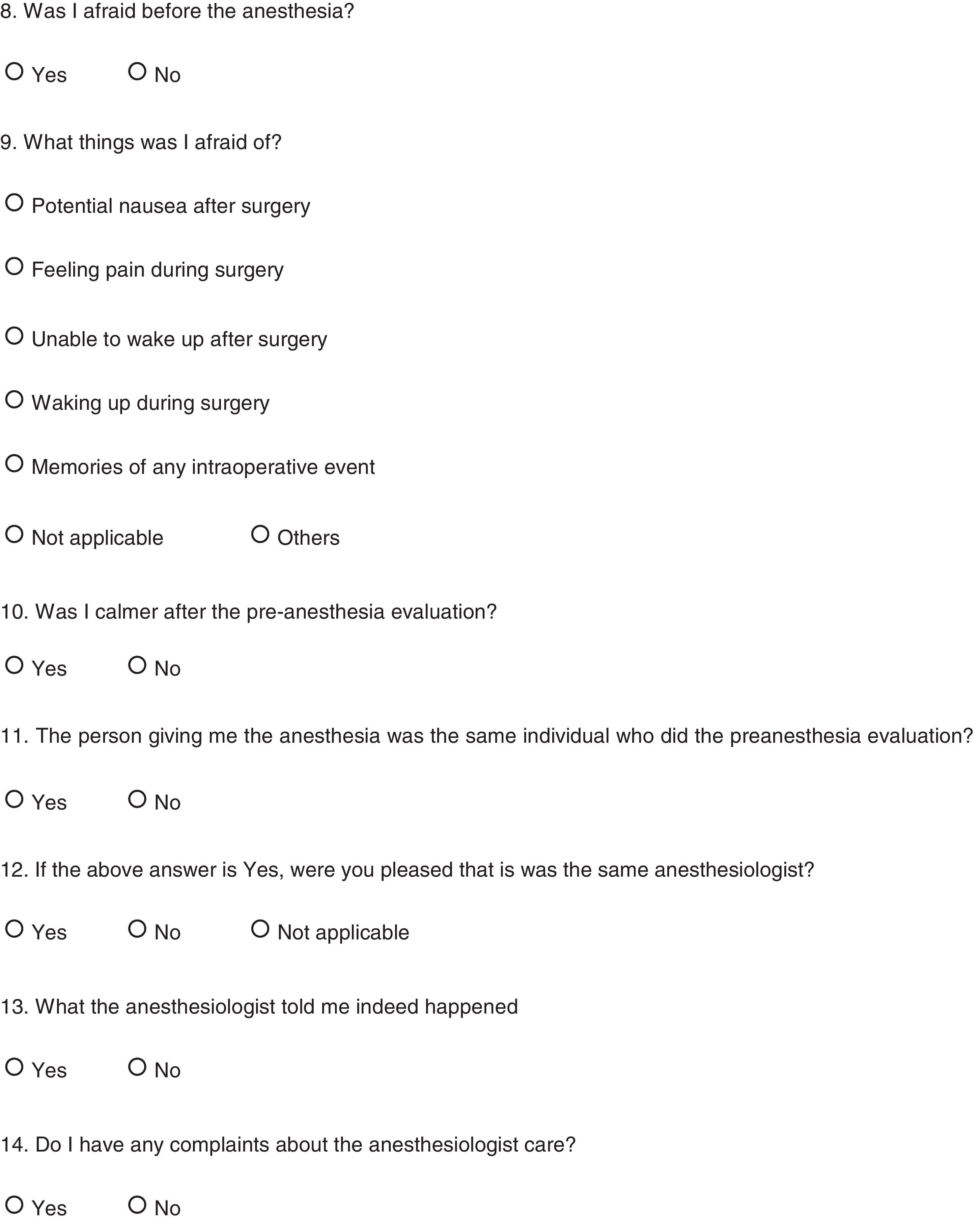
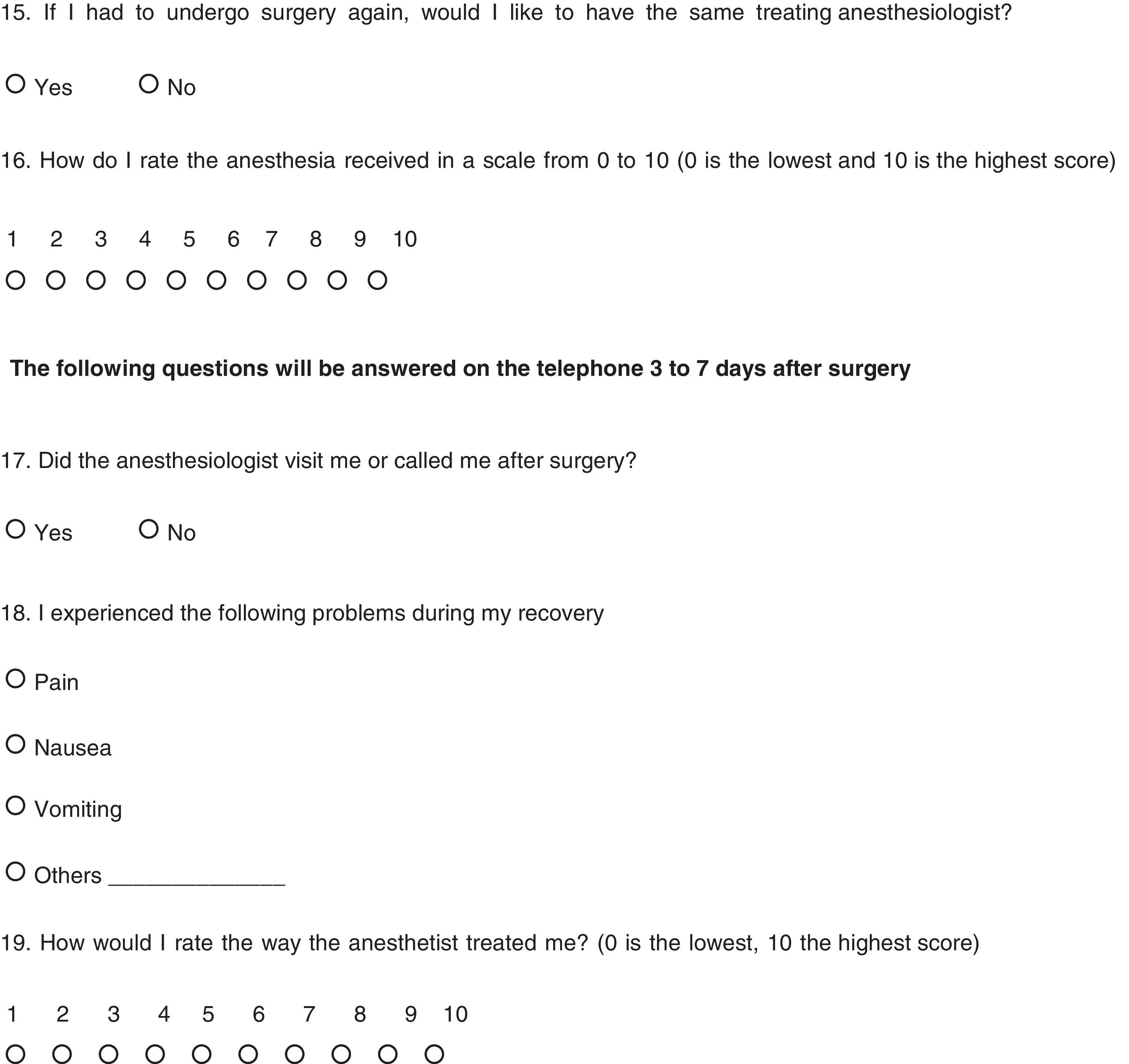
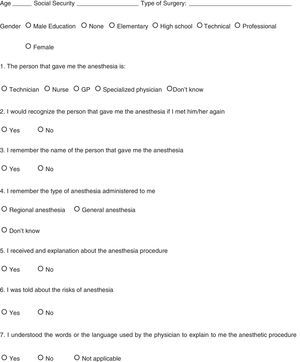
Data collectionAn opinion survey (Annex 1) during the immediate postoperative period and a telephone call three days later were used to collect the data. The patients responded to the surveys themselves but two trained assistant nurses were available to help patients who experienced difficulties in responding to the survey without influencing their answers.
The questionnaires were drafted according to the state-of-the-art variables and co-variables.9–11 A pilot test was given initially to 40 patients to test the data collection instrument in terms of extent of the information, method of application and comprehension; changes were made on the basis of the pilot test findings, but these results were not considered in the final analysis.
Data base management and designThe information collected was uploaded to an EXCEL database (Microsoft Office® 2010) and exported to the statistical package IBM® SPSS Statistics version 19.0 for processing and analysis.
Analysis planThe population was classified in terms of age distribution and gender. Proportion measures were used for all the qualitative variables.
Ethical considerationsThis trial was approved by the Ethics Committees for Research of the Universidad del Valle and of each of the participating institutions.
ResultsThe distribution of measurements by institution in the four participating centers, for a total of 340 surveys (version 1.1) completed in the course of nine months by patients in their 20s to 70s is shown in Table 1. 42% of the total population were males.
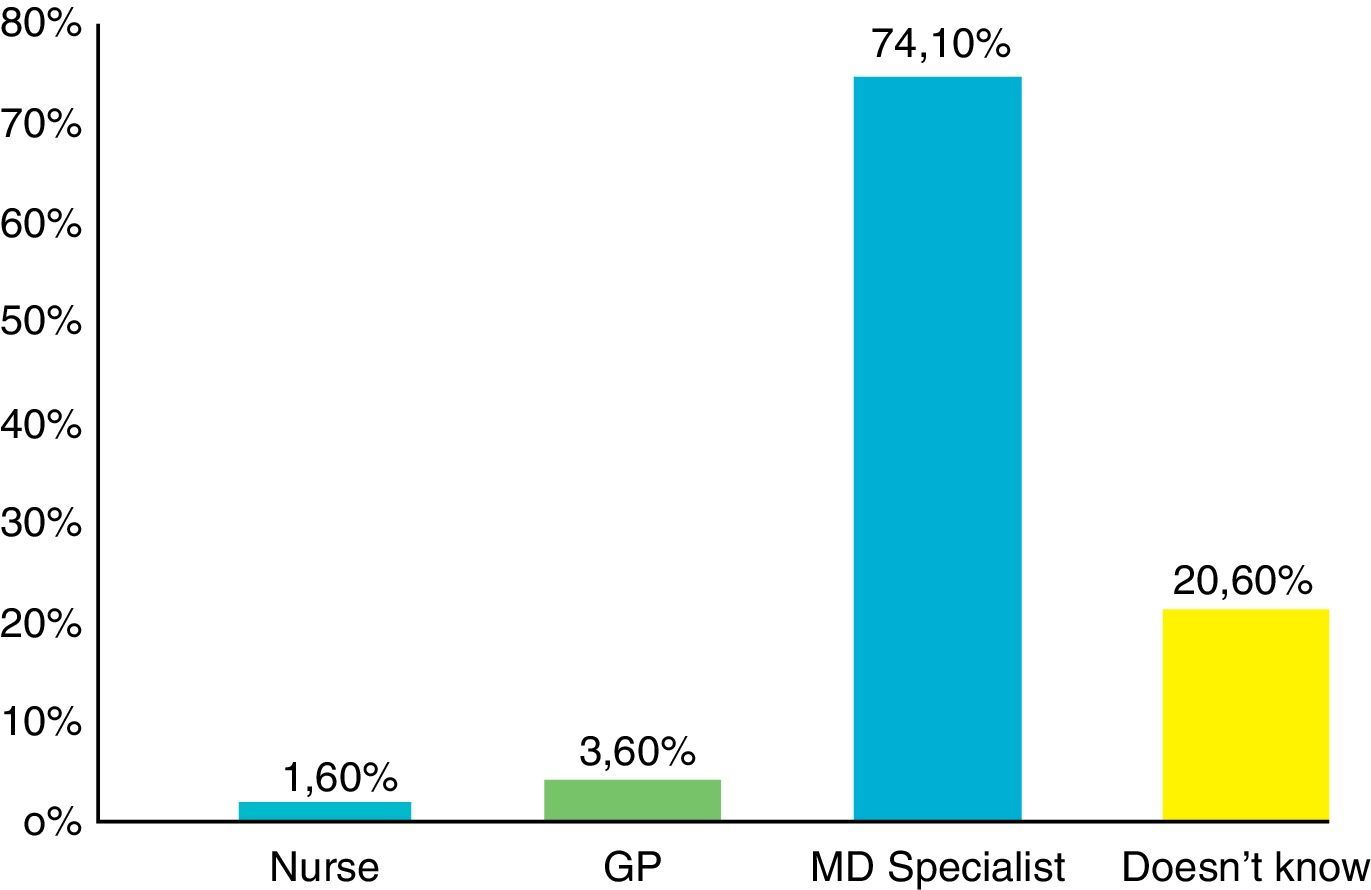
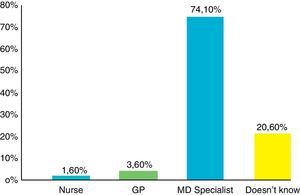
When asking the patients about their knowledge of the anesthesiologist's academic training, 74.1% of them acknowledged the anesthesiologist as a specialized physician and 21.2% were not aware of such professional training (Fig. 1).
When asked whether they would recognize the individual that administered their anesthesia, 86.5% said yes and 45% remembered their name. With regards to the anesthetic technique 23.2% of the patients surveyed did not know what type of anesthesia they were administered, 9.1% claimed that they were not given any explanation about the anesthetic procedure and 22.7% said that they were not briefed about the anesthesia-related risks. When evaluating the communication, 88.8% admitted that they understood the language used by the doctor and in 98.5% of the cases surveyed what the anesthesiologist explained to the patients before the procedure indeed happened.
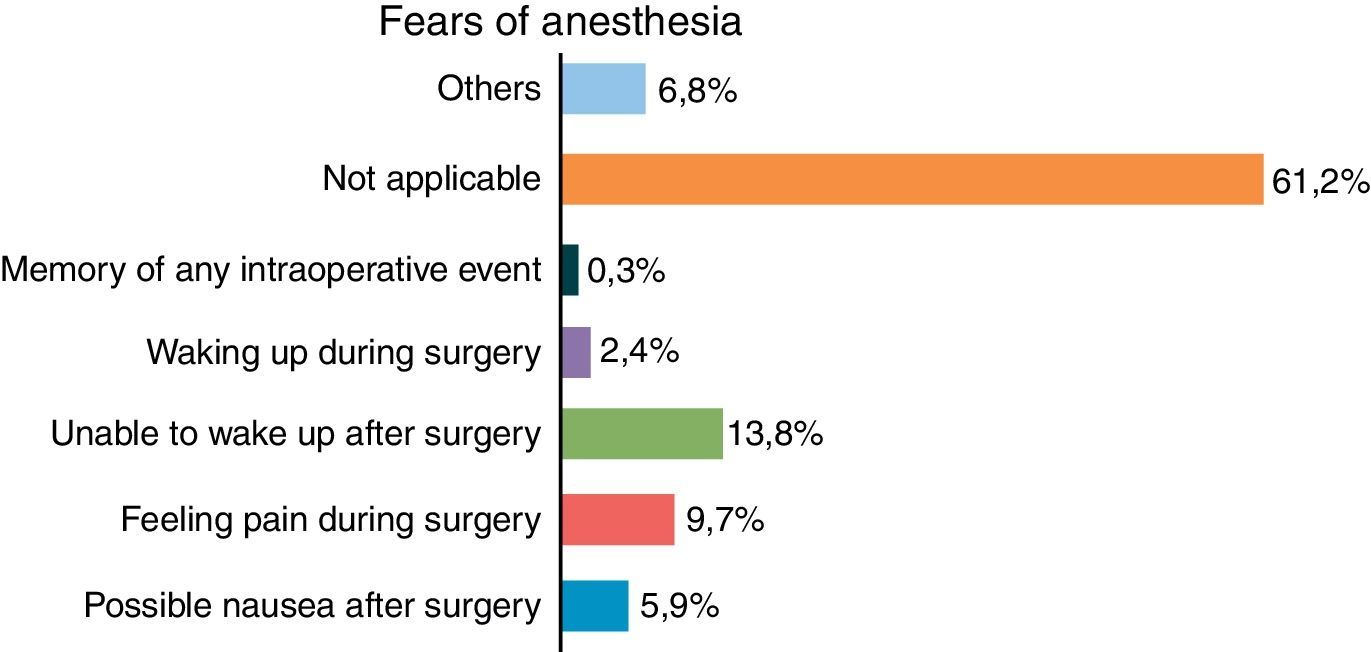
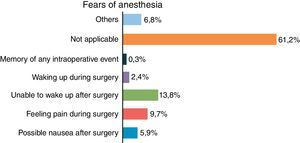
32.1% of the patients said they experienced some fear before the anesthesia. The main fears experienced were not being able to wake up after surgery (13.8%), feeling pain (9.7%) and experiencing nausea and/or vomiting (5.9%) (Fig. 2).
93.8% of the patients acknowledge feeling calmer after the pre-anesthesia evaluation. In 35.1% of the cases, the anesthetist who administered the anesthesia was the same persona that did the pre-surgical evaluation, and this pleased 99% of the patients.
When assessing the level of satisfaction, 98.2% of the population surveyed felt pleased with the anesthetic care, while 98.5% expressed that they would have liked that the anesthesiologist had been the same person who did the pre-surgical evaluation. The ratings given to anesthesia care were 10 in 82.1% of the sample, 9 in 11.2% and 8 in 4.1%. In terms of the telephone call three days after surgery, the survey showed that 66.5% of the patients did not receive a call or a visit from the anesthesiologist.
DiscussionThe initial APR reports were by Drs. Sheffer and Grefenstein in 1960. They concluded that the feeling of anxiety about anesthesia was mainly due to a poor relationship established by the anesthesiologist with the patient. They argued that anesthesiologists were perceived as impersonal and distant people who had skills and were efficient, but were not as real as other doctors. This could partially be explained because of the fleeting doctor–patient relationship and because of the effect of the pre and post-operative medication.2,12
When comparing our results against other previous trials, the findings indicate that the current perception of patients about the anesthesiologist has improved considerably.4 However, notably almost one fourth of patients are unaware of the type of academic training of the anesthesiologist. Although a considerable number of patients would recognize their anesthetist if they met him/her, only half of them would remember the name. It is our belief that the anxiolytic medication used perioperatively, may have an impact on these memories and on other details of the OR experience.2
Our work also yields interesting results about the perception of risk and the expectations around perioperative anesthesia care. Although currently in this day and age the patient has a fundamental right to receive clear and comprehensive information about the procedures he/she is about to undergo, including any risks, it is quite concerning that almost 10% of the patients claimed that they received no explanation about the anesthesia procedure and a higher number (23%) were not informed about the risks of anesthesia. This means that this so fundamental information is not given rigorously in the course of the pre-operative evaluation.
Notwithstanding the fact that the visit of the anesthetist to his/her patients is considered to be a legal and moral duty to make sure that the patient is fully recovered from the drugs used and to identify and treat any potential complication thereof,13 this visit was only reported in 33% of the cases. Hence, the Departments of Anesthesia and Perioperative Medicine should aim their efforts at retrieving the value of the post-anesthesia visit or at least the telephone follow-up. This simple though valuable action would result in improved empathy and acceptance among the community and could further strengthen the APR, acknowledging the constant devotion to safety of the anesthesiologist in the OR.4,5,14,15
We acknowledge some deficiencies in this paper we would like to mention. First of all, though a validated satisfaction scale was not used, the question asked in the survey was carefully studied so it was clearly understood and answered by the patient. In this case, all the questions were prepared and analyzed at successive meetings until a survey format was completed and agreed by the authors. The ethics committees of the participating institutions, making sure that the assisting staff did not influence the patients in their answers, closely followed this effort. The trial showed however that most patients expressed high satisfaction with anesthesia care.
To conclude we may say that despite the high level of outpatient satisfaction with anesthesia care, there is a need to strengthen the perception of patients about their relationship with the anesthesiologist, beyond the pre-anesthesia evaluation and the surgical procedure, including other perioperative considerations seldom discussed. Anesthesia specialists and anesthesiology organizations shall promote a closer relationship with the communities to educate them on the key role they play, contributing to the patient's care and safety.
FundingNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Giraldo Tascón VL, Castillo G, Quintero Saker U, Palacio L, Díaz Ante Y, Palacio Arboleda M, et al. Percepción de la relación anestesiólogo-paciente valorada en el posoperatorio de pacientes ASA I y II en instituciones de nivel III y IV (estudio RAP-2) en Santiago de Cali. Rev Colomb Anestesiol. 2014;42:20–27.