The pharynx is a musculomembranous tube common to the upper respiratory tract and the initial segment of the GI tract. Any endoscopic therapeutic procedure requires the participation of a competent anesthetist to secure the patency and control of the airway, upon the induction of general anesthesia that blocks the protective reflexes and hence prevents the passage of the GI contents into the lower respiratory tract. The endoscopist is required to be cautious in the use of the technique to accomplish the objective.
A clinical case of a failed endoscopic therapeutic procedure presenting subcutaneous emphysema, suggestive of a perforation is discussed. In order to define the topography and to make a differential diagnosis of the lesion, a clinical signs sequence is conducted that revealed a perforation of the posterior pharynx, then confirmed using endoscopic imaging. An algorithm is suggested to make the differential diagnosis between an intra and an extra-glottic perforation.
La faringe es un conducto músculo membranoso que es común a las vías respiratorias superiores y a la parte inicial del aparato digestivo, por lo que los procedimientos endoscópicos-terapéuticos requieren de la competencia del anestesiólogo, para la permeabilización y control de la vía respiratoria una vez que los reflejos protectores queden ausentes al inducirse la anestesia general, y de esta manera evitar el paso del contenido digestivo a la vía respiratoria inferior. Al mismo tiempo el endoscopista debe emplear una técnica cuidadosa que permita lograr el objetivo propuesto. Se expone un caso clínico que posterior a procedimiento endoscópico-terapéutico fallido presenta enfisema subcutáneo; que sugiere una perforación. Para determinar latopografía y diagnostico diferencial de la lesión se conduce a un análisis mediante la secuencia de signos clínico; los cuales ponen de manifiesto una perforación de la faringe posterior, que es confirmada mediante métodos imagenológicos y endoscópicos. Se propone un algoritmo para el diagnóstico diferencial entre una perforación intraglótica y extraglótica.
The pharynx is a musculomembranous tubular structure vertically positioned from the base of the skull down to the sixth cervical vertebra. This organ is shared by the upper respiratory tract and the initial segment of the GI tract and comprises three segments or levels: the rhinopharynx (upper segment), the oropharynx (middle segment), and the hypopharynx or laryngopharynx (lower segment).1,2 The pharynx participates in the respiratory function, deglutition, phonation and immunology. The pharynx allows for the passage of air from the nostrils and the mouth to the larynx and serves as a duct for transporting food from the oropharynx to the esophagus. The muscular structure of the pharynx plays a key role in deglutition to propel the alimentary bolus and protect the nasal and laryngeal airway.1–3 Orotracheal intubation is a means to isolate the airway from the GI tract and prevent the passage of the GI contents into the lower airway, particularly under special circumstances such as “full stomach” emergencies and general anesthesia with loss of the protective reflexes in patients undergoing GI tract surgery.4
The case of a patient under general balanced anesthesia with orotracheal intubation for endoscopic retrograde cholecystopancreatography (ERCP) is discussed. A traumatic lesion developed during the diagnostic-therapeutic procedure on the posterior wall of the pharynx, which resulted in subcutaneous emphysema. A clinical analysis of the sequence of events was performed to establish the etiologic, topographic and differential diagnosis of the complication.
Case reportThis is a female, 84-year old patient diagnosed with hepatitis and obstructive jaundice. The patient was evaluated by general surgery and internal medicine, and the gastroenterology service was asked to do an ERCP to determine the presence of extrahepatic biliary tract obstruction. The patient was initially assessed by the anesthesiology service to establish the perioperative approach. Several comorbidities were identified and the patient was classified as ASA-3. The preoperative examination indicated the following findings:
Mucus membranes with jaundiceDecompensated high blood pressure – the patient was evaluated by internal medicine and preoperative antihypertensive treatment was prescribed with captopril 25mg every 12h and oral hydrochlorothiazide 25mg per day until the BP was normalized.
- •
Mucus membranes with jaundice.
- •
Decompensated high blood pressure: the patient was evaluated by internal medicine and preoperative antihypertensive treatment was prescribed with captopril 25mg every 12 hours and oral hydrochlorothiazide 25mg per day until the BP was normalized.
- •
Additional medication: oral cholestyramine 4g/day, IV ranitidine 50mg every 12h.
- •
Physical–neurological examination: aware, able to follow verbal orders, no sensitive or motor disorders.
- •
Altered hepatic enzymes: alanine aminotransferase – Glutamic-Pyruvic Transaminase GPT, aspartate aminotransferase – glutamic oxaloacetic transaminase GOT, alkaline phosphatase, total and direct bilirubin.
- •
Alkaline phosphatase: 990 (39–117U/l), ALT-GPT: 89U/l (0–41U/l), ASAT-GOT: 72U/l (0–38U/l), Total bilirubin: 8mg/dl (0–1mg/dl), Direct bilirubin: 7.1mg/dl (0–0.3mg/dl).
- •
Altered renal function tests: elevated Creatinine that then dropped and normal blood urea nitrogen (BUN).
- •
Initial serum Creatinine: 2.2mg/dl (0.7–1.2mg/dl).
- •
Change in Creatinine 2nd day: 1.5mg/dl.
- •
Complete blood count (CBC): mild anemia, normal leukocyte and platelet count.
- •
Hemoglobin: 9.8g/dl (12.5–18g/dl).
- •
Hematocrit: 29% (36–54%).
- •
C-reactive protein: 96mg/l (<1mg/l) increased.
Other tests performed were normal: rest ECG, chest X-ray, thrombin and thromboplastin times, arterial gases, electrolytes, blood glucose and troponins. The predictors evaluated showed no airway difficulties.
Due to the increased risk of perioperative morbidity and mortality, the family is educated on the possibility administering conservative treatment to the patient rather than doing an invasive procedure. However, the family insists on doing the procedure despite the risks and signed the informed consent.
The patient is placed in supine decubitus for monitoring in the OR. The electrodes are placed for leads DII electrocardiography, partial oxygen saturation pSO2, non-invasive blood pressure (NIBP), capnometry and capnography; peripheral vein crystalloid fluids perfusion is initiated based on basal needs, concurrent losses and fasting. The vital signs prior to the induction of anesthesia were normal. Facemask pre-oxygenation is administered to 100% pSO2. Rapid sequence induction with IV Propofol 100mg and Rocuronium 30mg is administered, maintaining cricoid pressure. Laryngoscopy using curved blade 3 Macintosh indicates Cormack–Lehane grade 1, visualizing a normal wide larynx and a single-attempt atraumatic, fast and smooth intubation was performed with a No. 8 tube, without using a guide or stylet. The tube was inserted and the pneumo-tamponade balloon inflated with 3–5ml of air with mild closure pressure over the laryngeal mucosa. The tube placement was verified through inspection and auscultation of both lung fields; the end-tidal CO2 curve is observed and the tube is fixed and coupled to the Dragger Primus anesthesia machine according to the following parameters: tidal volume 8ml/kg of body weight; respiratory rate 12rpm; inspiration/expiration ratio=1:2; 100% FiO2 for a peak inspiratory pressure of 17mmHg. Sevorane was administered at a 1MAC to achieve the level of hypnosis required and IV remifentanil at 0.1mcg/kg/min was initiated and titrated as needed. After the cardiorespiratory parameters were stabilized following the induction of anesthesia, the patient was placed in a left lateral decubitus position to proceed to surgery. The duodenoscope was introduced by mouth with some degree of resistance probably due to anatomic alterations and it fails to advance beyond 20cm of the labial commissure. A few minutes later the oral cavity and the nostrils begin to bleed but no communication was established with the lower airway. There is no blood flow through the endotracheal tube, which upon aspiration does not show any signs of blood secretions. The respiratory monitoring – particularly peak pressure, expired tidal volume, and capnography – is normal. A structure, which is not consistent with the esophageal mucosa or the larynx, is visualized through the endoscope. Then a smaller gauge duodenoscope was introduced and a tear of the posterior pharyngeal wall is identified, with bleeding and mucosal integrity down to the stomach. Subcutaneous emphysema is identified, with involvement of the neck and the anterior aspect of the thorax. The procedure is then interrupted and the patient is maintained intubated and ventilated. Further evaluation of the patient by the general surgeon includes chest X-rays, evidencing emphysema of the right segment of the neck and the right hemithorax, with no hemothorax or pneumothorax, no mediastinal or pneumopericardium widening. The patient is maintained intubated under conscious sedation, and the parameters monitored remained stable. The patient is transferred to the higher level of care ICU for better follow-up, evolution and behavior.
A bronchoscopy performed in the ICU indicated the absence of lesions from the carina all the way up to the glottis; however, there is evidence of tear of the layers of the posterior pharyngeal wall. In view of the characteristics of the lesion and the risks inherent to the patient, surgery is not an option. Conservative therapy is adopted, including ventilation support and antimicrobial therapy. No data have been made available from the institution where the patient was admitted and consequently the patient's evolution is unknown.
DiscussionA number of factors must be considered for a diagnostic, etiological and topographic approach of the airway and GI tract, when procedures involving the patency and protection of the airway are performed, with endotracheal intubation and GI endoscopy.
The rate of complications associated with diagnostic GI tract procedures is one in 1000 studies and a maximum of one death per 10,000 procedures. Perforations are extremely rare, with an incidence of 0.03% but it is associated with a high morbidity and mortality. These are more frequent in the cervical esophagus at the level of the hypopharynx and may be the result of instrumental complications or patient-related complications such as weakness, malnutrition, old age, and caustic stenosis. The patient-associated risk factors include the presence of Zenker diverticulum, tumors, stenosis, achalasia, anterior osteophytes of the cervical spine, and removal of foreign bodies.5
A preliminary evaluation is a must to prevent the above complications. Particular tests such as coagulation tests, CBC or biochemical testing, chest X-ray, ECG, are not strictly required among the healthy population, due to the low prevalence of abnormalities; however, these are usually prescribed for improved safety and should absolutely be required based on the patient's medical record ad physical examination.5
Perforation of one or more sites of the airway secondary to endotracheal intubation is a rare but potentially lethal complication.6 The risk factors involved with this complication are the presence of several intubation attempts in difficult airway patients, the use of metallic guides or stylets, large gauge endotracheal tubes such as double lumen tubes and Combitube, elderly patients with loss of the elastic and muscle fibers of GI tract tubular structures and overdistention of the respiratory tract, female patient, inexperienced practitioner, and emergency situations.7 In this particular patient, the only factors present were old age and female gender, so the probability of injury to the posterior pharynx were negligible.
In terms of the level of difficulty to visualize the different segments of the larynx, the Cormarck–Lehane classification includes 4 grades: Grade 1 is total view of the glottis that requires no additional maneuvers for enhanced visualization and intubation.8 The subsequent grades require ancillary maneuvers such as BURP (back upper right pressure) and the use of alternate devices to facilitate the intubation, such as stylets, guides and the Eschmann guide.9 These were not needed in this patient.
The laryngoscopy technique requires alignment of the oral, pharyngeal and laryngeal axis. Such alignment entails hyperextension of the neck to the classical “sniffing” position. With the patient's mouth open the blade of the laryngoscope is introduced next to the right commissure of the lip, advancing to the glossoepiglottic fold; the tongue is displaced to the left side and pulled anteriorly to elevate the epiglottis and expose the vocal folds.10 Thus, pressure is applied to the free end of the blade of the laryngoscope on the anterior wall rather than the posterior wall where the traumatic lesion was identified, which corresponds to the sliding and advancement over the posterior wall of the free end of the scope from its anterior position in the mouth.
The most frequent cause of pharyngeal-esophageal injury is iatrogenic perforation due to endoscopic instrumentation of the GI tract. With the use of flexible devices such risk is low, but it becomes higher in therapeutic procedures.11 Severe complications such as mediastinitis, respiratory distress and persistent fistulae, in addition to the site of the lesion, delayed diagnosis and timely treatment, are all relevant in determining morbidity and mortality.12
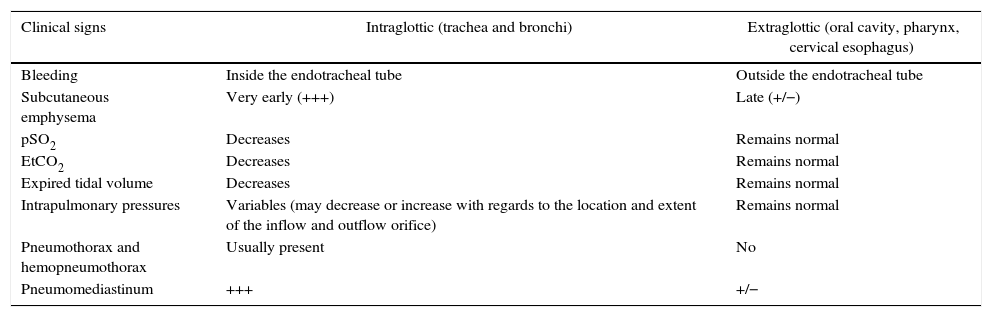
The typical clinical manifestations in conscious patients are pain, difficulty to swallow, fever, and subcutaneous emphysema of the cervical region.13 In this particular case, bleeding by mouth during the attempts to introduce and advance the endoscope, the visualization of a path inconsistent with the esophageal mucosa or the larynx, and then the presence of subcutaneous air with no communication or effect on the lower airway and respiratory function with the patient unconscious under general anesthesia, are all suspicious of the diagnosis that is later confirmed by imaging and endoscopy. A differential diagnosis algorithm is suggested for the potential localization of the lesion, based on the clinical signs identified (Table 1).
Differential diagnosis to identify the probable site of the perforation in the airway/GI tract of the patient under general endotracheal anesthesia.
| Clinical signs | Intraglottic (trachea and bronchi) | Extraglottic (oral cavity, pharynx, cervical esophagus) |
|---|---|---|
| Bleeding | Inside the endotracheal tube | Outside the endotracheal tube |
| Subcutaneous emphysema | Very early (+++) | Late (+/−) |
| pSO2 | Decreases | Remains normal |
| EtCO2 | Decreases | Remains normal |
| Expired tidal volume | Decreases | Remains normal |
| Intrapulmonary pressures | Variables (may decrease or increase with regards to the location and extent of the inflow and outflow orifice) | Remains normal |
| Pneumothorax and hemopneumothorax | Usually present | No |
| Pneumomediastinum | +++ | +/− |
In sum, the perforation of the pharynx during a therapeutic endoscopic procedure is a rare occurrence but both the anesthetist and the endoscopist should be attentive since the pharynx is the only site where the respiratory and the GI tract come together. The history, the sequence and the analysis of the clinical signs are all indicative of the etiological and differential diagnosis that is then confirmed using imaging and endoscopic methods.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FinancingNone declared.
Conflicts of interestNone declared.
Please cite this article as: Fernández-Ramos H, González-Guzmán EF, Ramos-Montero HM, Gualy-Cuchimba DA, Guerrero-Legro VH. Perforacion faringea durante procedimiento endoscopico terapeutico. Informe de caso. Rev Colomb Anestesiol. 2017;45:21–25.