The post-anesthesia care unit has been identified as a vulnerable area for the occurrence of adverse events. Here, the nursing staff is responsible for managing and taking care of patients.
ObjectiveTo explore the perception of the professional nursing staff about the performance of the post-anesthesia care unit, and portray certain aspects of its operations.
Materials and methodsThis is a mixed sequential study including an observational, descriptive and quantitative cross section phase and a qualitative, descriptive, interpretative phase, using grounded theory.
ResultsNurses perceive the PACU as “a place for care” with weak processes such as patient handover and monitoring, communications among care providers, lack of specific skills of the ancillary staff and lack of team work. Work overload, extended administrative tasks that take away focus from patient care, in addition to a lack of compliance with protocols, are all conducive to the occurrence of adverse events.
ConclusionsNurses perceive the unit as a place of complex processes and particular characteristics that make the unit prone to adverse events. Institutional factors, work team and professional-related aspects become threats that undermine the safety environment that should always prevail in every PACU. Specific strategies are discussed to turn the recovery unit into a safe care service for the surgical patient.
La unidad de cuidados postanestésicos se ha identificado como un sitio vulnerable para la presentación de eventos adversos; en este lugar es el personal de enfermería quien se encargan del manejo y cuidado de los pacientes.
ObjetivoExplorar las percepciones que tiene el personal de enfermería profesional acerca del funcionamiento de la Unidad de cuidados postanestésicos y caracterizar algunos aspectos de su funcionamiento.
Materiales y MétodosEstudio con enfoque mixto secuencial: una fase cuantitativa descriptiva observacional de corte transversal y una cualitativa de tipo descriptivo interpretativo utilizando teoría fundamentada.
ResultadosLos enfermeros perciben la unidad de cuidados postanestésicos como “un sitio para el cuidado” con debilidades en procesos como la entrega y monitoreo de pacientes, la comunicación del personal asistencial, falencia en habilidades específicas del personal auxiliar y ausencia de trabajo en equipo. La sobrecarga de trabajo, un aumento de labores administrativas que desplazan el cuidado del paciente, así como la falta de adherencia a protocolos, son percibidos como situaciones que facilitan la presentación de eventos adversos.
ConclusionesLa unidad es percibida por los enfermeros como un lugar de procesos complejos y características particulares que la hacen susceptible de eventos adversos. Factores a nivel de la institución, el grupo de trabajo y el profesional se convierten en amenazas que socavan el ambiente de seguridad que debería prevalecer en un servicio de recuperación postanestésica. Se proponen estrategias específicas que impulsen a la unidad de recuperación como un servicio de atención segura para el paciente quirúrgico.
The development of surgical specialties has brought about increasing volumes and growing complexity of procedures, with larger number of interventions in elderly and multiple comorbidities patients. This trend impacts the post-anesthesia care unit (PACU), which has been identified as a vulnerable place for the occurrence of care-related adverse events.1–5
The publications available in the literature have focused on describing the events, the frequency thereof, and intraoperative anesthesia-related factors. Based on the analytical models for adverse events,6 additional considerations such as communication, training, workload, inter alia, are also relevant.7–10
Although the anesthesiologist is responsible for the patient in the PACU, the professional and LPNs staff is in charge of managing and caring for the patient. In the case of complex patients or patients with multiple comorbidities, the role of professional caregivers is even more crucial. However, we are not aware of the perception professional nurses have about the unit in this setting. The objective of the research was to explore the perceptions of the professional nursing staff about the operation of the PACU and portray some functional aspects.
Materials and methodsA mixed approach, with sequential implementation study was undertaken, including a cross sectional observational, descriptive and quantitative phase and a descriptive, interpretative qualitative phase.
Professional nurses from around the country from the FEPASDE (Special Fund for Solidary Assistance in Claims) database were included. These nurses are currently working or worked for at least two years at a PACU in level 2–4 institutions; however, nurses working in surgery but not making shifts in the PACU were excluded. For the qualitative phase, nurses who were involved in an adverse event (AE) in the PACU during the past year were included. The final number of nurses and their distribution was based on a theoretical sampling, excluding nurses with less than tree months of work experience in the unit or that had participated in opinion studies over the last six months.
Structured e-mail surveys were conducted among all nurses in the FEPASDE database and the surveys were completed on line. An initial literature review allowed for the identification of issues regarding the occurrence of adverse events in the PACU and this information was the basis for the design of the survey, including the most frequent complications in the PACU, critical structural aspects, human resources, processes, and documentation in the medical record. Questions were asked about PACU patient handover, perception about the level of training of the ancillary nursing staff, as well as about the available resources for patient management and workload. No validated instruments were found in the literature to evaluate these aspects. The reference criteria for processes such as patient handover and staff competencies were taken from the clinical practice.11,12
Based on the survey, nurses involved with AEs in the past year and that met the inclusion criteria for the qualitative phase were identified. A semi-structured interview guide was developed including questions related to on-the-job experience, PACU roles, and handling of protocols. The central nucleus and the peripheral system were built on the basis of the AEs in the PACU, using the Social Representations Theory for guidance.13 Five nurses from level two, five nurses from level three, and eight nurses from level four institutions were interviewed, to fulfill the various categories. The interviews were conducted by professionals in social sciences and were audio recorded for future transcription and analysis.
The STATA® 12 software was used for the quantitative analysis, showing central trend and scatter for continuous numerical variables. The absolute and relative frequencies are presented for nominal variables. ANOVA was used to compare the results based on the level of complexity of the institutions, in case of normal distribution; otherwise, the Kruskal–Wallis test was performed. For nominal variables, the chi square or Fisher's test was used as appropriate, with a significant p≤0.05 value.
The analysis of the qualitative data was done using the method of the open, axial, and selective level coding grounded theory that allowed for a strict handling of the data, reducing dependability, identifying cross-referencing and saturation of coding. PACU and adverse event-associated linguistic networks were identified. The ATLAS.TI® version 6.2 software was used.
The research protocol was approved by S.C.A.R.E.’s ethics committee. The informed consent was required and completed (online for the quantitative phase and in person for the qualitative phase).
ResultsThe nursing staff154 nurses completed the online survey (34% response). 50% of the nurses were 33 years of age or younger, (interquartile range: 10). 38.4% worked at level III institutions and an equal percentage at level IV institutions with no age differences between the groups (p=0.86). The qualitative phase included working men and women between 27 and 58 years of age, with a seniority in their job ranging from 3 to 20 years. Henceforth, the word “survey” shall refer to the quantitative phase, while the word “interview” refers to the qualitative phase.
The interviews identified that workdays are 8–12h long, which in the latter case are considered exhausting in terms of length of time and as a result off the highly demanding tasks. There are few breaks and time management is difficult. Often nurses have several jobs to raise their income and leisure time is devoted to activities that separate them from their routine (from family life to high-impact sports).
Their personal interests include altruism (major motivation for being a nurse) and personal development through training and graduate programs to improve their profile.
Nurses perceive that their role impacts the patient's outcome, they enjoy what they do and are motivated by efficient teams, though in their opinion this is seldom the case in the PACU. Work overload was repeatedly mentioned. In accordance with the survey on administrative tasks, these limit the time nurses have to devote to patient care and remove them from the professional role they are expected to fulfill.
PACU description50% of the nurses surveyed have two or more stretchers in the recovery room per each operating room. 50% report having a monitor available per one to five patients. 66% of the nurses surveyed report not having neuromuscular relaxation monitoring available in the PACU. None of the variables was related to the level of complexity of the institution they work for (p<0.05).
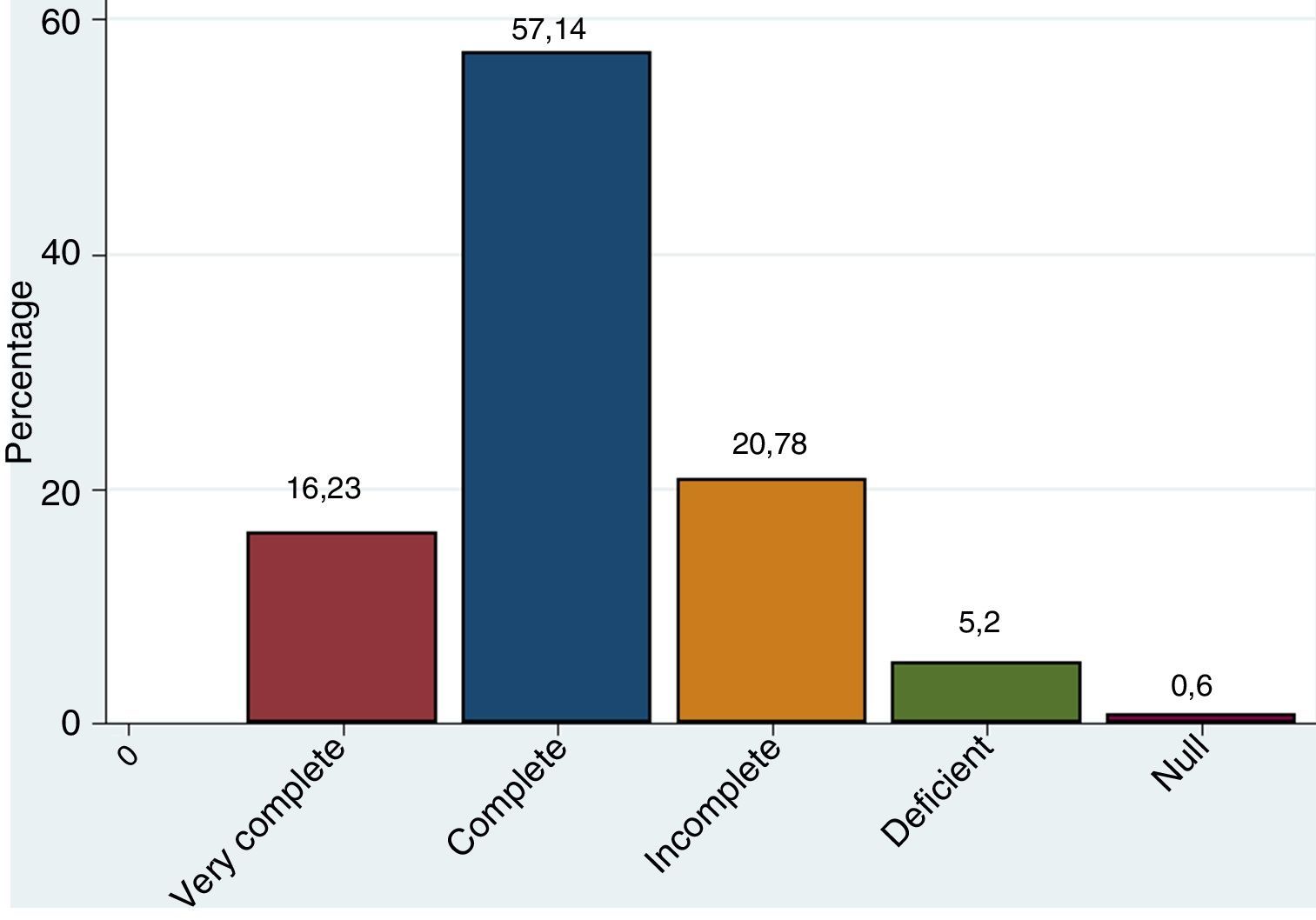
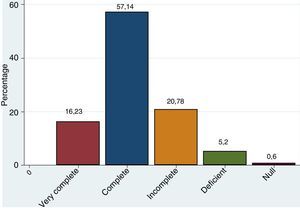
Patient handover at the PACU64% of the nurses surveyed said that the anesthesiologists handover the patient at the PACU, 32% said that the handover is the responsibility of the LPN. Although 57% of the nurses surveyed feel that the handover information is of good quality, 26% consider it incomplete (Fig. 1). No relationship was found between the level of complexity of the institution and the quality of information (p=0.77).
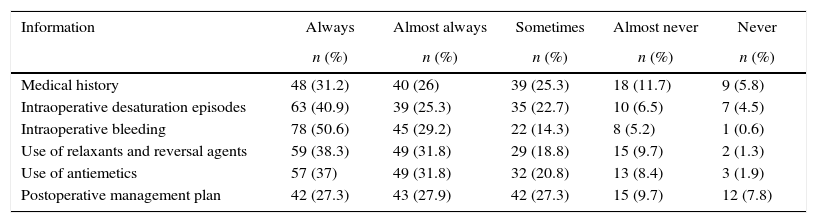
With regards to the question on how often is specific pre or intra-operative information reported at handover in the PACU, 20–45% felt that the information provided was incomplete. Table 1 illustrates the frequency of the answers.
Response rate about the information report at patient handover in the PACU.
| Information | Always | Almost always | Sometimes | Almost never | Never |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Medical history | 48 (31.2) | 40 (26) | 39 (25.3) | 18 (11.7) | 9 (5.8) |
| Intraoperative desaturation episodes | 63 (40.9) | 39 (25.3) | 35 (22.7) | 10 (6.5) | 7 (4.5) |
| Intraoperative bleeding | 78 (50.6) | 45 (29.2) | 22 (14.3) | 8 (5.2) | 1 (0.6) |
| Use of relaxants and reversal agents | 59 (38.3) | 49 (31.8) | 29 (18.8) | 15 (9.7) | 2 (1.3) |
| Use of antiemetics | 57 (37) | 49 (31.8) | 32 (20.8) | 13 (8.4) | 3 (1.9) |
| Postoperative management plan | 42 (27.3) | 43 (27.9) | 42 (27.3) | 15 (9.7) | 12 (7.8) |
During the interviews, the lack of knowledge about the patient's “baseline condition prior to surgery” is considered a limitation for management; the workload prevents them from having a comprehensive enquiry about the patient's history and any intraoperative events in the medical record.
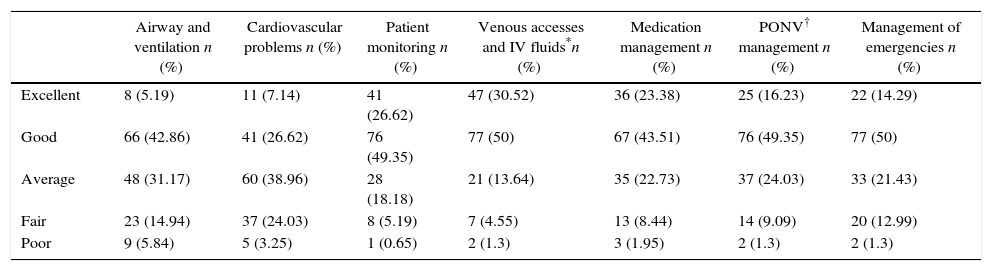
Perception about the level of training of the LPN staffThere is a variable perception among professional nurses about the level of training of LPNs (Table 2). With regards to skills such as “monitoring”, “venous accesses”, and “medication management”, the level of training is perceived to be high; in terms of cardiovascular problems, airway issues and emergencies, the rating is mostly negative. The qualitative phase found across the board, that head nurses find deficits in the training of LPNs for dealing with emergencies and other situations typical of a PACU. Moreover, nurse assistants are usually temporarily removed from the unit in order to assist in other services, which increases the workload for the rest of the staff.
Nurses perception about the level of training of LPNs on the various competencies required at the PACU (n=154).
| Airway and ventilation n (%) | Cardiovascular problems n (%) | Patient monitoring n (%) | Venous accesses and IV fluids*n (%) | Medication management n (%) | PONV† management n (%) | Management of emergencies n (%) | |
|---|---|---|---|---|---|---|---|
| Excellent | 8 (5.19) | 11 (7.14) | 41 (26.62) | 47 (30.52) | 36 (23.38) | 25 (16.23) | 22 (14.29) |
| Good | 66 (42.86) | 41 (26.62) | 76 (49.35) | 77 (50) | 67 (43.51) | 76 (49.35) | 77 (50) |
| Average | 48 (31.17) | 60 (38.96) | 28 (18.18) | 21 (13.64) | 35 (22.73) | 37 (24.03) | 33 (21.43) |
| Fair | 23 (14.94) | 37 (24.03) | 8 (5.19) | 7 (4.55) | 13 (8.44) | 14 (9.09) | 20 (12.99) |
| Poor | 9 (5.84) | 5 (3.25) | 1 (0.65) | 2 (1.3) | 3 (1.95) | 2 (1.3) | 2 (1.3) |
During the interviews, work overload was frequently mentioned as usual, both in terms on number of tasks and in terms of number of work hours. In accordance with the surveys, the average number of patients assigned to a LPN per shift is four, and for professional nurses the number is eight.
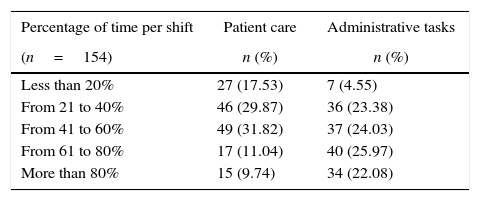
Nurses report a considerable administrative burden including: documentary management, medication entries to the system, coordinating admission and discharge of patients, LPNs supervision, diet lists, reaching the anesthesiologist as needed, and be the liaison between the anesthesiologist and the nurse assistants. Their level of responsibility for the service is high, though they have little time to devote to patient care (Table 3). LPNs are in closer contact with the patient and their obligations are related to healthcare, although their level of responsibility for service activities is lower.
Response rate about the percentage of time devoted to patient care versus administrative tasks.
| Percentage of time per shift | Patient care | Administrative tasks |
|---|---|---|
| (n=154) | n (%) | n (%) |
| Less than 20% | 27 (17.53) | 7 (4.55) |
| From 21 to 40% | 46 (29.87) | 36 (23.38) |
| From 41 to 60% | 49 (31.82) | 37 (24.03) |
| From 61 to 80% | 17 (11.04) | 40 (25.97) |
| More than 80% | 15 (9.74) | 34 (22.08) |
According to the interviewees, the anesthesiologist in the PACU is responsible for the patient handover, making evaluations, deciding on management of post-anesthesia complications and being constantly in touch with the physician who operated on the patient. The length of time the anesthesiologist remains in the unit depends on the patient's complexity. Contact between the surgeon and the recovery nurse is usually through the anesthesiologists.
Perception about the forms used in the PACUThe importance of record-keeping was acknowledged during the surveys; however, the lack of time and of training prevent proper documentation of all processes. Hand records are time-consuming and sometimes illegible, while digital forms are faster, although some types of software are complex. The delay in making records due to a shortage of computers and the “cut-and-paste” practice are a limitation to the quality of the information recorded.
Often there is failure to document information about the intra-operative period, nausea and vomiting, pain assessment and doctor's orders. Regardless of the level of complexity, the surveys showed that 51% of the nurses do not routinely use the recovery scale at admission to the PACU (p=0.17); the Aldrete scale is the most popular, though 16% of the nurses administering the scale fail to record the scores.
According to the interviews, when the patient is discharged from the PACU some forms may not be completed such as the surgeon's postoperative recommendations and the proof of understanding of the caregiver regarding care recommendations, because processes tend to be slow and time-consuming.
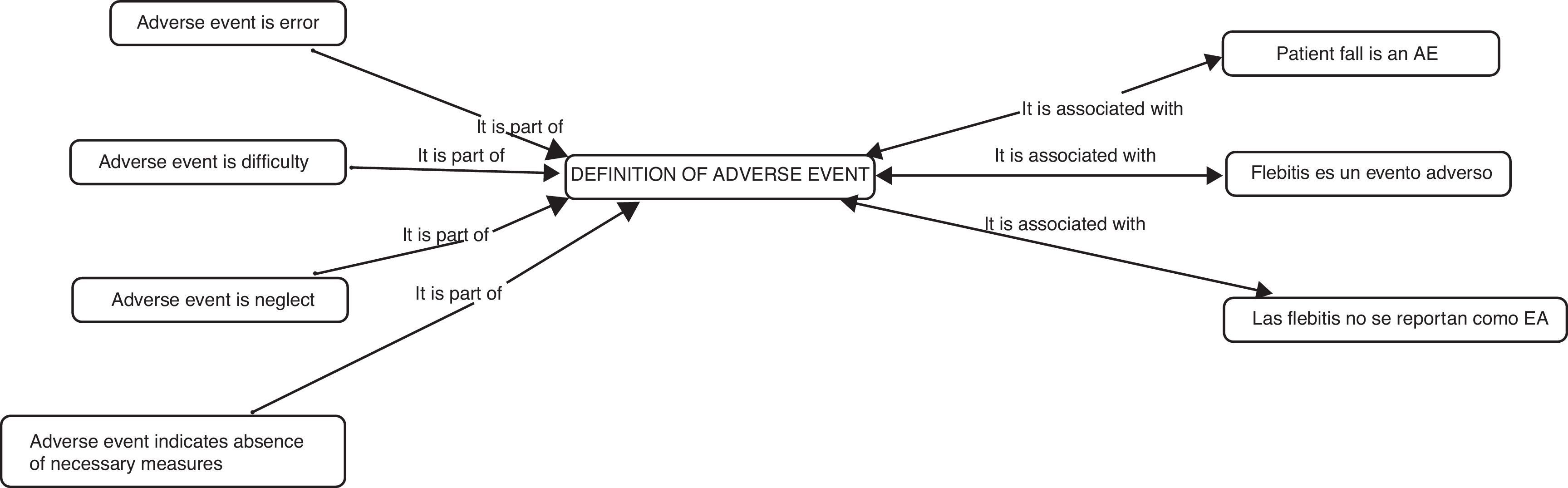
Social representation of adverse eventsThe verbatim analysis of the interviews indicates that the central nucleus of the social representation of the AE is associated with patient complications. Reference is made to non-preventable situations or situations that could not be controlled (Fig. 2). All the qualitative phase participants experienced an AE (whether directly or indirectly) and mentioned the key role of anesthesiologists for a successful resolution in most of these events.
In the opinion of the interviewees, an AE report may change based on the severity of the associated damage. The more severe, the more evident the need to report the event. In case of low severity events, the report may be disregarded or if the report is submitted (phlebitis, pressure sores), it may lead to social punishment but does not necessarily translate into enhanced policies.
Some of the risk factors that nurses perceive as AE-associated include working conditions under shortage of staff, high volume of patients, and the current trend of focusing on administrative chores. Psychosocial factors are also reported, such as high level of stress, long workdays, few hours of sleep, and lack of active breaks. Excessive self-confidence in performing their roles that “justifies” the failure to comply with the protocols, in addition to automation of some tasks that has removed the “human touch”.
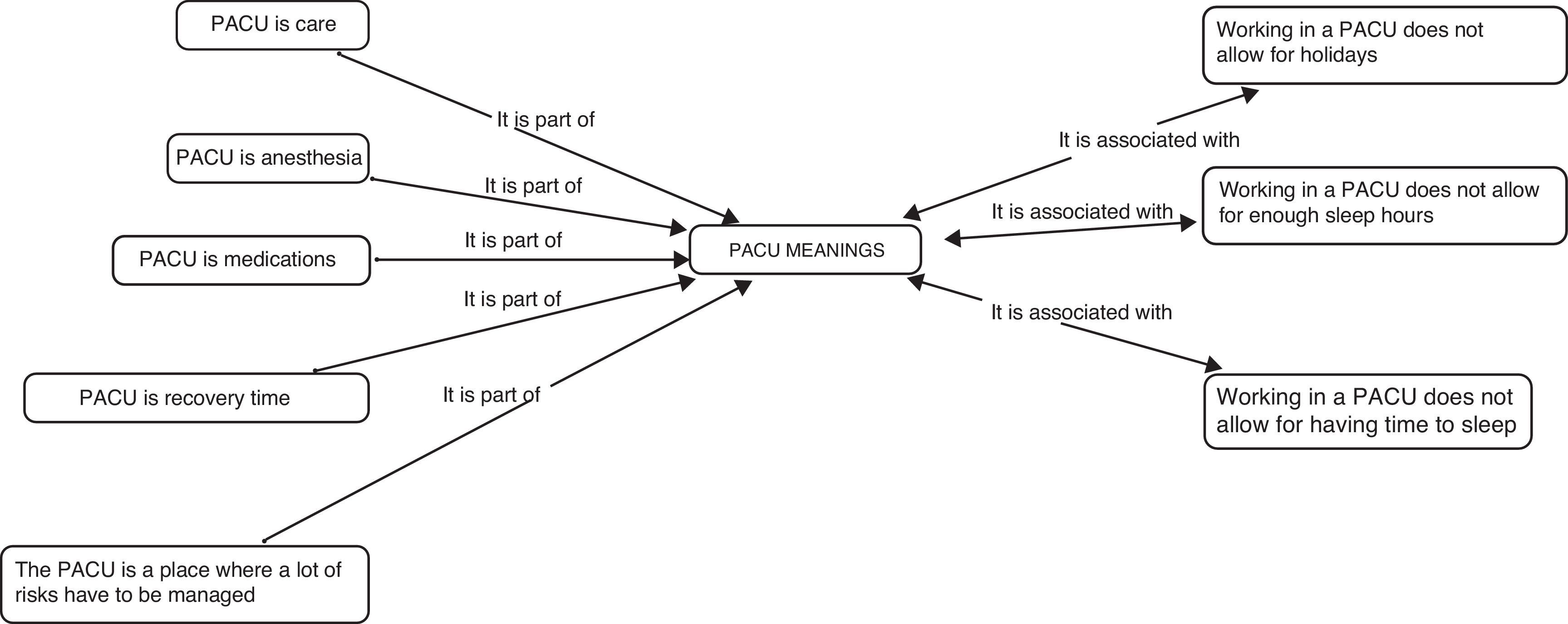
Social representation of the PACUThe PACU-associated words included: care, anesthesia, and medications (Fig. 3). The functional and operating characteristics of the PACU were highlighted, as well as the poor emphasis on the fact that they “manage a patient in pain”; this helps to understand the automation of tasks as reported by the participants. Another aspect emphasized by the interviewees with regards to ideas of the PACU, is team work, and they claim that “nothing can be done on your own”. However, the social representations identified fail to associate the PACU with team work. This means that the concept has not been internalized since it is not part of their daily activities. Various roles are associated with some activities, but a common action is not identified.
DiscussionThis research describes the perception of professional nurses about the PACU, identifying flaws in the operational activities and in the way the technical and staff needs are being met. There is a perceived weakness in the patient handover process at the PACU, particularly with regards to the postoperative management that could potentially compromise the continuity of care. There is a strong reliance on verbal communications. Milby14 in 2013 described low frequency in delivering information such as the ASA status and fluid management. Moreover, the amount of information remembered by the recipient at the PACU is estimated at only 47%.15
From the qualitative perspective, hierarchical barriers to communication were identified (between surgeons, anesthesiologists, and both professional nurses and LPNs). These deficits may be due to the absence of structured information reporting systems as previously described in other studies16 and may be evidenced in the failure to use recovery scales as well as specific reporting forms.
Specific interventions to improve patient handover between different services, particularly using multimodal strategies during the postoperative period.17 The use of structures electronic forms, web-based tools, training in communication process simulation and post-training feedback has been recently described.18 A systematic review published in 2013 showed that the implementation of structured handover protocols and interventions to improve communication skills, improve the patient handover in the PACU, when measured as an outcome of missing information at the time of handover and technical errors. This interventions did not increase the average patient handover time in PACU patients.19
The low frequency in the availability of neuromuscular relaxation monitoring in the PACU should be noted, despite being a requirement under the current standards. Residual relaxation is still an issue frequently reported at arrival to the PACU in up to 56% of the cases20; this, in addition to the lack of information about the use of relaxants and reversal agents, makes the unit prone to complications derived from residual neuromuscular blockade.
Furthermore, PACU human resources are also perceived as deficient, both in terms of LPNs training deficits and in terms of skills. The staff surveyed identified training deficits in LPNS, and although the scores are variable based on the competency assessed, the lowest rating corresponds to management of critical events in the PACU. Various strategies have documented shortfalls in specific skills of the PACU nursing staff.21–23 Additionally, there is poor knowledge about the most common complications during the recovery period and how to manage such complications.
Workload was a repeated complaint during the interviews and it is also reflected in the patient-to-professional nurse and LPNs ratio. The survey administered reported numbers as high as 20 patients per LPN. Studies have shown that work overload of the nursing staff raises the rates of hospital complications and mortality. Increasing by one more patient the nurse's workload, raises the probability of in-hospital patient death by 7% over the first 30 days upon admission.24 It has been difficult however, to precisely determine the PACU staffing requirements, probably due to the particular characteristics that make the PACU unit different from other hospital services.25,26 Parameters should be established to standardize the right number of skilled staff required in the unit, in accordance with the minimal safety standards in anesthesiology, in addition to appointing an institutional internal control body to reduce nursing work overload to a minimum. There are international guidelines currently available that establish the minimum standards for perioperative management and one of these guidelines addresses nursing in particular.27,28
Professional nurses report lack of time to focus on patient care tasks due to a heavy administrative burden. This results in a feeling of frustration to their vocational motivation. It is indeed contradictory that the staff with the major responsibilities in the service and top level training, has less patient contact.
The social representations of an adverse event are associated with poor care resulting from either the patient's own conditions or from the surrounding labor and institutional conditions. The PACU is represented as a care area with clearly defined roles, but deficient processes in terms of communication, team work, and the overall perception about the patient. The first two issues have been identified in recent qualitative studies.29–31 There were no reports found addressing the issue of social representations as herein described.
This research paper provides information from a combined approach. The quantitative phase was used on nurses around the country, while the qualitative phase – due to limitations in interviewing logistics – took place in Bogotá. Such qualitative approach focuses on learning and understanding the problem; however, the sampling process based on the convenience of the quantitative phase and the characteristics of the qualitative approach, is not intended to generalize or derive probabilistic conclusions.32 It should be noted that the scope of the study is basically exploratory from a novel perspective, that helps to approach the issue from the point of view of stakeholders that had not been previously involved. The results shall be analyzed within the framework of the particular situation at each institution and region in the country. A more in depth knowledge of the way a PACU operates requires a unit-based analysis, comparing the results to the current standards and to the way “things should be” from the patient safety perspective.
Based on the results of this research, the recommendation is to implement and strengthen a patient safety-oriented risk management model, with a preventive rather than reactive approach. Since 1990 the literature refers to the need to use risk management models in the PACU, specifically from the nursing role perspective.33 Including training programs in non-technical skills shall help to strengthen the humanistic approach and the assertive communication processes among the various hierarchical levels in the surgical environment, as well as in the way patients are treated, the team work approach, and systematic reporting of adverse events.
The professional and academic bodies shall also make the institutional health care administrative staff aware of the risks involved in the PACU and of the consequences derived from staff shortages and workload.
The end goal is to evolve toward a comprehensive approach to the “Postsurgical care unit” that actively and in a more participative manner involves all of the perioperative care staff, redefining the importance of the PACU unit.
ConclusionsThe PACU has its own particular processes and characteristics that make it susceptible to adverse events. The complexity of the patients, the staff shortages, the work overload, communications, the allocation of healthcare and administrative tasks, in addition to a poor teamwork definition, are all perceived by the professional nursing staff as drawbacks that undermine the safety environment that should always prevail in a post-anesthesia recovery unit.
In order to minimize the occurrence of AEs and to provide a thorough and proactive management of the patient, the conditions of the institution shall be improved (staffing, training programs, distribution of shifts, improved adverse event management), as well as the conditions of the healthcare professionals and of the patient handover process (baseline information, shared medical records, health and care-related education) in order to ensure comprehensive and preventive management of the surgical patient.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article.
FinancingThis project was funded by the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.).
Conflicts of interestThe authors have no conflict of interest to disclose.
Please cite this article as: Arias-Botero JH, Padrón-Mercado CM. Caracterización del funcionamiento de la unidad de cuidados postanestésicos a partir de la percepción del personal de enfermería profesional. Rev Colomb Anestesiol. 2017;45:16–23.