We present a clinical case report of a child with scimitar syndrome and a review of the literature in order to describe the main surgical and anesthetic implications of these patients. Child, 4 months old, weight 4700g, diagnosed with pneumonia and left lobar emphysema requires mechanical intubation and ICU care. The associated diagnoses are failed extubation, severe pulmonary hypertension and scimitar syndrome confirmed with echocardiography. He was scheduled for pulmonary lobectomy. His mother signed an informed consent authorization for anesthesia and surgery. The child entered surgery, intravenous anesthetic induction was performed and a central venous catheter, an arterial line, urinary catheter and pre-and post-ductal pulse oximeters were inserted. He required vasopressor support with dopamine and transfusion of red blood cells. No adverse events during surgery. At the end of the surgery he was carried back to pediatric ICU and intubated with a chest tube. Extubation was successfully performed 2 days later with favorable progress. Scimitar syndrome is characterized by an anomalous right pulmonary venous return associated with congenital heart disease and pulmonary malformations. It has a low prevalence in the population but a very high perioperative morbidity and mortality, especially in children. With this report we present the main standards and practices for anesthetic management, monitoring and hemodynamic goals with these patients.
Se presenta un reporte de caso clínico de un niño con Síndrome de Cimitarra y revisión de la literatura existente con el fin de describir las principales implicaciones quirúrgicas y anestésicas de estos pacientes. Niño de 4 meses de edad, peso de 4700 grs. Ingresó por cuadro de neumonía con enfisema lobar izquierdo que requirió intubación mecánica y manejo en la Unidad de Cuidados Intensivos. Los diagnósticos asociados son extubación fallida, hipertensión pulmonar severa y Síndrome de Cimitarra confirmada por ecocardiografía. Es programado para lobectomía pulmonar izquierda. La madre firmó consentimiento informado para la anestesia y para la cirugía. Ingresa a cirugía; se realiza inducción anestésica intravenosa y se coloca cateter venoso central, línea arterial, sonda vesical y pulsoximetros pre y posductal. Requirió soporte vaopresor con dopamina y transfusión de glóbulos rojos. No eventos adversos durante la cirugía, se lleva de nuevo a la UCI pediátrica intubado, con tubo a torax y se logra extubar dos días después con evolución favorable. El Síndrome de Cimitarra se caracteriza por un drenaje venoso pulmonar anómalo derecho asociado a cardiopatías congénitas y malformaciones pulmonares. Tiene una prevalencia baja dentro de la población pero una morbimortalidad perioperatoria muy alta sobretodo en niños. Con este reporte se presentan unas pautas concretas y prácticas para el manejo anestésico, la monitorización y las metas hemodinámicas de estos pacientes.
Scimitar syndrome belongs to the group of venolobar syndromes associated with pulmonary sequestration and congenital heart anomalies1. It has a low incidence of 1–5 per 100000 births2. It is characterized an anomalous right pulmonary venous return and cardiovascular compromise3. Its presentation in childhood requires early surgical interventions to correct the illness. The goal of this case report is to review the literature addressing this type of anomalies to describe the main goals for anesthetic management and to achieve good perioperative results.
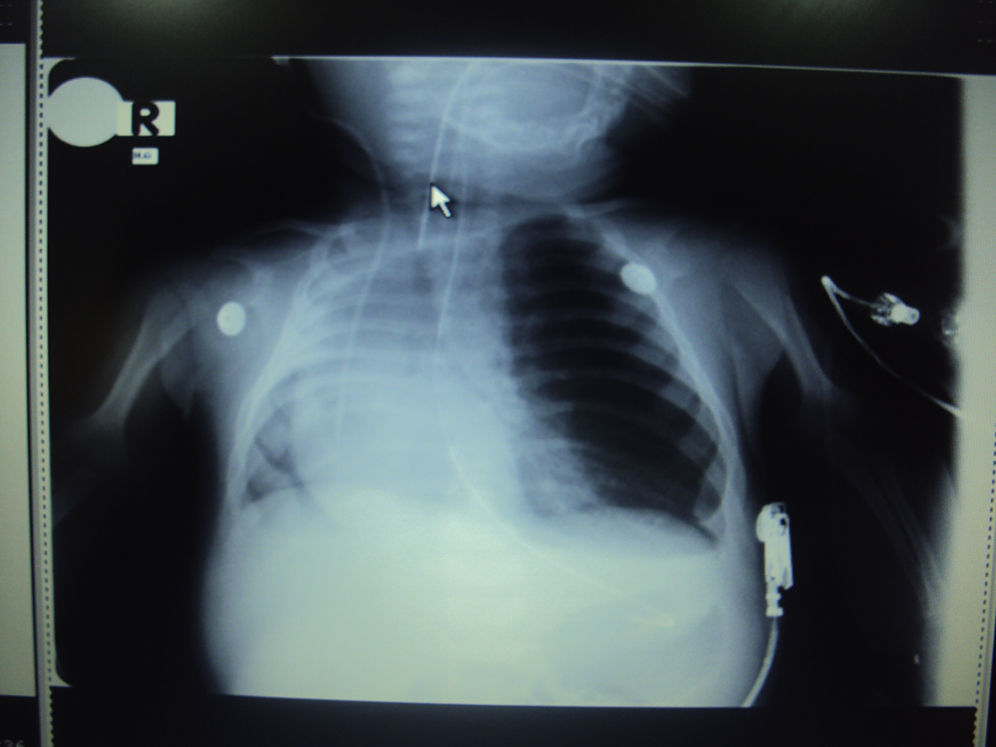
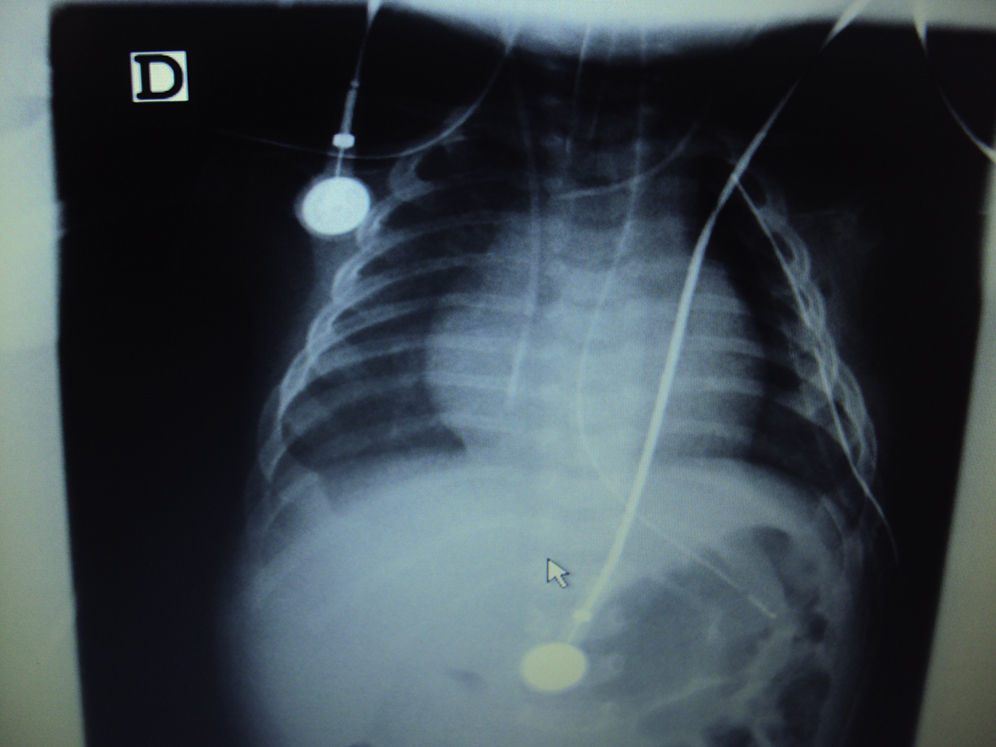
Case reportBoy of 4 months of age, 4700g, with diagnoses of pneumonia and left congenital lobar emphysema with collapse in the right lung.
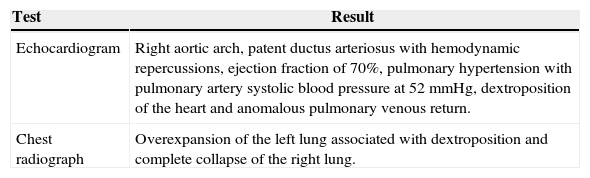
That patient is on mechanical ventilation with a previous failed extubation, severe pulmonary hypertension (PSP 52mmHG), and a diagnosis of scimitar syndrome by echocardiography. The results of the paraclinical tests are described in Table 1.
Results of paraclinical tests.
| Test | Result |
|---|---|
| Echocardiogram | Right aortic arch, patent ductus arteriosus with hemodynamic repercussions, ejection fraction of 70%, pulmonary hypertension with pulmonary artery systolic blood pressure at 52mmHg, dextroposition of the heart and anomalous pulmonary venous return. |
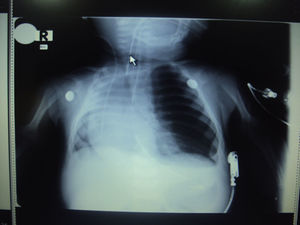
| Chest radiograph | Overexpansion of the left lung associated with dextroposition and complete collapse of the right lung. |
Source: authors.
The patient was scheduled for upper left lobectomy for the resection of the area of the lung with emphysema. The mother signed an informed consent form for anesthesia and surgery (Fig. 1).
Monitoring was carried out with an external left jugular venous catheter, a posterior tibial arterial line, an electrocardiogram, preductal and postductal pulsoximeters, capnography, a urinary catheter, and esophageal temperature.
The induction of anesthesia was performed with 50mcg of fentanyl and 20mg of propofol. For the maintenance of anesthesia, 0.3mcg/kg/min of remifentanil and 1 MAC sevofluorane were administered. The mechanical ventilation was controlled by pressure, with low pressures and volumes and FIO2 at 80% to maintain capnography (30–36mmHg) and oximetry (90–93) within the normal ranges.
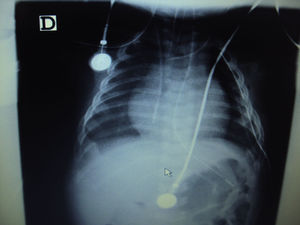
During surgery hypotension was presented, which required the administration of dopamine at 5mcg/kg/min. Intraoperative hemoglobin was 8.7mg/dl, so 70cc of red blood cells were transfused. No adverse events were presented during surgery. The postoperative radiograph of the chest shows improvement in the expansion of the right lung, see Fig. 2.
The patient was transferred to the intensive care unit with ventilatory and vasopressor support under sedation analgesia. He was extubated 2 days later with a satisfactory evolution.
DiscussionScimitar syndrome is a rare congenital disease. The largest series of cases reported to date describe 44 cases in adult patients3 and 16 in children4. The prevalence in the general population is low, which reflects the perioperative challenge associated with these patients and the importance of understanding the anesthetic implications due to its high perioperative mortality rate1,2.
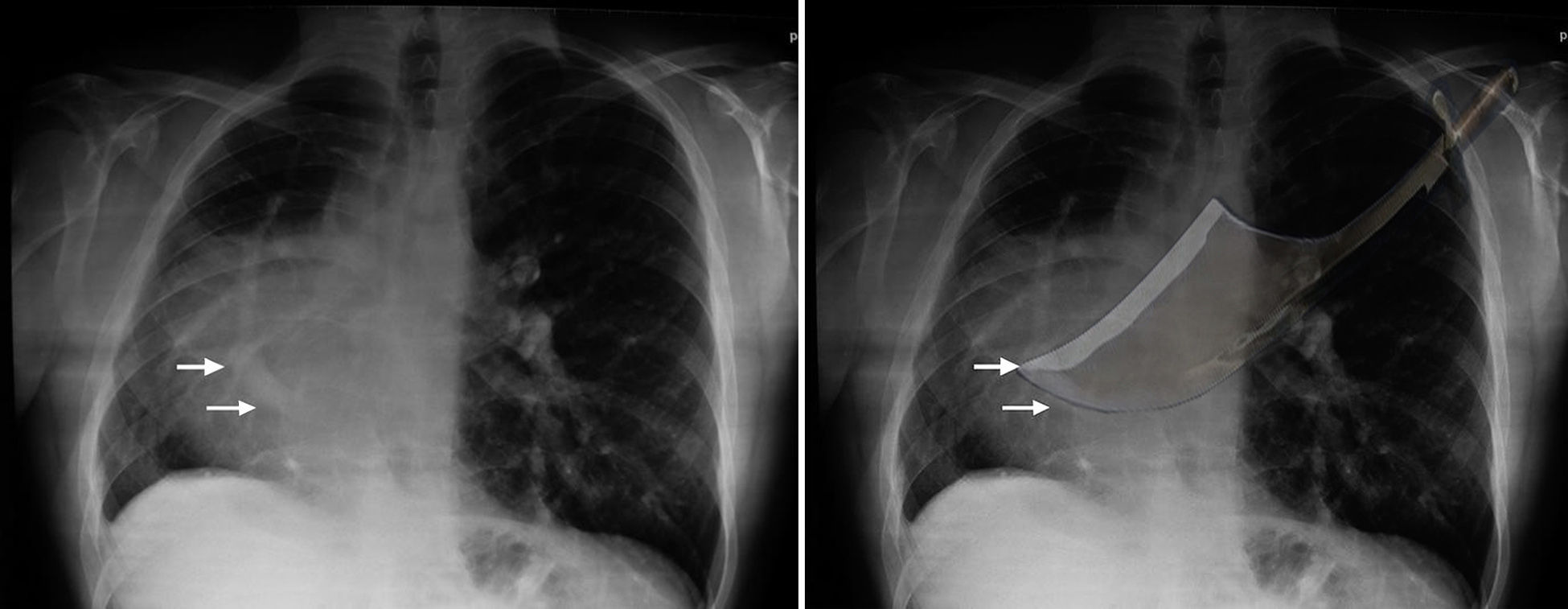
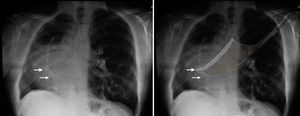
The first case was reported in 1836 by a Doctor Cooper, who gave it its name because of the image as shown on a chest X-ray: long and curved on the right edge of the heart, which corresponds to the anomalous venous return from the right lung in the right atrium or vena cava, similar in shape to the scimitar blade that originated in Persia2,5,6, see Fig. 3.
This syndrome represents 4% of anomalous pulmonary venous returns. It is associated with alterations in pulmonary arterial supply, right pulmonary hypoplasia, and hypoplasia of the right bronchus and right pulmonary artery4,5,7. The most frequent heart alterations are the dextroposition of the heart with displacement of the mediastinum, absence of the pericardium and other malformations, such as atrial septal defect (60–70%) or ventricular septal defect, coarctation of the aorta, and tetralogy of Fallot in 25% of cases3,6,7.
Tow types of presentation have been described: adult and pediatric. In adults, the effects of the short circuit are low, without pulmonary hypertension in 77% of cases, or with slight hypertension in 23%. Usually, treatment is not required. However, when the syndrome appears in the neonatal period, it presents as heart or respiratory failure secondary to pulmonary hypertension and generally requires surgery. The prognosis depends on the severity of the associated anomalies, on the management of the pulmonary hypertension, and on the clinical condition of the child8.
These patients may present recurrent respiratory infections and respiratory failure, depending on the degree of pulmonary hypoplasia. In addition, it may appear with hemoptysis or as an incidental finding, as in adults5,9. Children with symptoms of cardiac arrest due to pulmonary hypertension have a poor prognosis1.
The pulmonary hypertension is caused by a short circuit, from left to right, through the anomalous circulation in the right lung, which, when associated with pulmonary hypoplasia and anomalous pulmonary return, increases the pressure in the right cavities. The pulmonary hypoplasia increases the intrapulmonary short circuit which, associated with the stricture of the pulmonary vein and other congenital malformations, produces persistent pulmonary hypertension10,11. In the physical examination, movement of heart sounds to the right and heart murmurs can be found, and pulmonary auscultation can be normal or reduced.
Diagnosis is performed with an echocardiogram showing the scimitar vein in 70% of cases. It has greater sensitivity in sever cases of the syndrome and shows associated cardiac alterations3. Three-dimensional tomography or cardiac magnetic resonance imaging are fundamental for visualizing the anomalous pulmonary vein and clarifying the patient's anatomy12. Cardiac catheterization and angiography confirm the diagnosis, giving detailed information about the patient's anatomy and the severity of the pulmonary hypertension. They are useful for surgical planning11–13.
Treatment depends on age and symptomatology. In newborns, it starts with management of the pulmonary hypertension. Surgery is recommended in patients with persistent heart failure, recurrent infectious diseases, or refractory pulmonary hypertension2.
Cases that present pulmonary sequestration require lobectomies and interruption of the anomalous systemic flow through embolization or direct ligation, as well as the closure of the septal defects1.
The prognosis is good when the pulmonary hypertension is slight or disappears. Anomalous arterial supply, the severe obstruction of the pulmonary veins, and congenital cardiopathies are associated with poor prognoses3–5.
Anesthetic implicationsA comprehensive assessment of the patient, with emphasis in heart and respiratory function should be performed. Pre-surgical examinations that may be required, including: CBC, arterial blood gas, blood typing, chest radiograph, and echocardiogram.
Having a reserve of red blood cells is necessary in the intensive post-operative care unit. The most important anesthetic implications are related to the presence of intracardiac short circuits and pulmonary hypertension, for which the patient's conditions before surgery should be optimized.
Surgical monitoring is performed with electrocardiograms and measurements of invasive blood pressure, preductal and postductal oxygen saturation, urinary catheter, capnography, temperature, and a central venous catheter.
The airway should be secured with a tracheal tube. Selective pulmonary intubation is not necessary, since the patients tend to have pulmonary hypoplasia and present ventilation predominantly with the healthy lung. This improves the surgical field. Pressure-controlled mechanical ventilation, to avoid barotraumas or volutrauma, is recommended14. Low volumes (<8ml/kg) and plateau pressure <30cm H2O are recommended.
The risk of cardiac arrest, death, and pulmonary hypertensive crisis is greater in patients with heart failure. The causes of the pulmonary hypertensive crisis should be corrected, including: hypoxia, hypercapnia, metabolic acidosis, hypothermia, pain, and any stimulus of the sympathetic nervous system15.
The anesthetic goals included maintaining an appropriate anesthetic plan, guaranteeing appropriate analgesia, avoiding the increase in pulmonary arterial pressure, and optimizing heart function with normal systemic blood pressure for the age, intubation, and hemodynamic stability. Intravenous induction agents (midazolam, ketamine, propofol) with an opioid (fentanyl or remifentanil) and a non-depolarizing muscle relaxant can be used. The goal is to avoid hypotension with the administration of bolus injections. Inhalatory induction is less effective due to the pulmonary hypoplasia and may produce greater myocardial depression. Anesthetic maintenance can be conducted with inhaled agents and a continuous infusion of opioids15.
In the case of pulmonary hypertensive crisis, pulmonary vascular resistance must be reduced, an adequate cardiac output maintained, and the stimulus that triggered the crisis removed16,17. Management of pulmonary hypertension is performed with slight hyperventilation with 100% oxygen, by correcting metabolic and respiratory acidosis, by using selective pulmonary vasodilators like inhaled nitric oxide, by correcting hypotension and low output (norepinephrine, dopamine, or epinephrine) and by using inodilators like dobutamine or milrinone15–18.
Intravenous analgesia based on opioids or regional analgesic techniques that do not compromise hemodynamic conditions are recommended.
ConclusionScimitar syndrome is a rare disorder that is associated with a range of congenital cardiac and pulmonary anomalies. The management of the patients should be individualized and defined by a multidisciplinary team. The anesthetic considerations should be focused on the management of the pulmonary hypertension, hemodynamic goals, and postoperative analgesia.
Conflicts of interestThe authors have no conflicts of interest to declare.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe authors did not receive sponsorship to undertake this article.
Please cite this article as: Luna-Durán AM, González-Serrano G, Echeverry P. Implicaciones anestésicas del Síndrome de Cimitarra para cirugía no cardiaca. Rev Colomb Anestesiol. 2015;43:245–249.