Perioperative hypothermia is a common condition associated with serious complications and perioperative mortality. The incidence of perioperative hypothermia is between 30 and 70%.
ObjectiveTo determine the status of perioperative monitoring and thermal protection in clinics and hospitals of high complexity in Colombia and the establishment of minimum safety standards of the Colombian Society of Anesthesiology to this respect.
MethodsA survey with voluntary answers was administered to leaders of anesthesiology departments and surgical services of high complexity institutions in Colombia. The questionnaire had 20 items with an adaptive structure and was sent by email to a randomized list. Only fully completed questionnaires were analyzed.
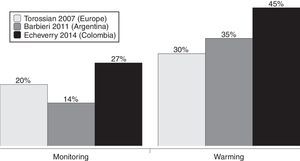
Results135 surveys were analyzed. Measurement of temperature is reported always or almost always in 27% of cases, while 45% have at least one method of intraoperative thermal protection. Barriers for monitoring temperature and for thermal protection were explored.
ConclusionsTemperature monitoring and perioperative thermal protection is insufficient in the sample studied. The reasons are: limited availability of devices for monitoring and protection and lack of interest toward the subject. There is no acceptance of minimum safety standards of the Colombian Society of Anesthesiology (S.C.A.R.E.) because of the limited availability of thermometers, poor monitoring of intraoperative temperature and misuse of heating strategies.
La hipotermia perioperatoria es una condición frecuente que se asocia a complicaciones serias que en algunos casos pueden ser potencialmente letales. La incidencia de hipotermia perioperatoria oscila entre 30 y 70%.
ObjetivoDeterminar la situación de la monitorización y protección térmica perioperatoria en instituciones prestadoras de servicios de salud de alta complejidad en Colombia y la apropiación de las normas mínimas de seguridad de la Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.) sobre este aspecto.
MétodosSe realizó una encuesta cerrada por internet de diligenciamiento voluntario. El cuestionario de 20 ítems tenia una estructura adaptativa, fue administrado por correo electrónico, y se dirigió a líderes de departamentos de anestesiología y servicios quirúrgicos de alta complejidad en Colombia. Solo se analizaron cuestionarios completamente respondidos.
ResultadosSe analizaron 135 encuestas. Los encuestados refirieron realizar la medición de la temperatura siempre o casi siempre en 27% de los casos, mientras que 45% disponen de al menos un método de protección térmica intraoperatoria. Se exploraron las barreras para la monitorización y la protección térmica perioperatoria.
ConclusionesLa monitorización de la temperatura y la protección térmica perioperatoria es insuficiente en la muestra estudiada. Esto como consecuencia de poca disponibilidad de dispositivos para monitorización y protección y por falta de interés frente al tema. No hay apropiación de las normas mínimas de seguridad de la S.C.A.R.E., dada la poca disponibilidad de termómetros, la escasa monitorización de la temperatura intraoperatoria y el uso inadecuado de las estrategias de calentamiento.
Perioperative hypothermia is a very frequent condition resulting from anesthetic and surgical procedures. It is associated with very serious complications that, in some cases, can be lethal.1 Perioperative hypothermia is defined as a core temperature ≤35.9°C, and its incidence varies between 30 and 70%.2–4 A heterogeneous cohort studied in Colombia showed that the frequency of perioperative hypothermia is similar to the same condition in other countries, and that close to 6% of patients are found to be hypothermic before the induction of anesthesia.5 The study also found that the incidence of hypothermia is influenced by age, weight, preoperative body temperature, ambient temperature, and the duration of the surgical procedure.5 These findings are consistent with those of other studies.6–8 Perioperative hypothermia has been associated with several complications such as chills, thermal discomfort, increase in the duration of some pharmaceuticals, increase in post-anesthetic recovery time and hospitalization time, and in the most serious cases, increase in the risk of infection of the surgical site, risk of cardiac event (arrhythmias and ischemia) and increase in surgical bleeding.9–12
Currently, the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.) recommends in its Minimum Safety Standards that temperature monitoring is obligatory in heart surgery, in moderate or severe trauma, in surgeries performed on newborns and small children, in surgeries of more than 3h, and in those in which blood loss is predicted to be more than one blood volume.13 It also recommends that it is highly desirable to have methods of avoiding cooling available, in order to warm the patients.13
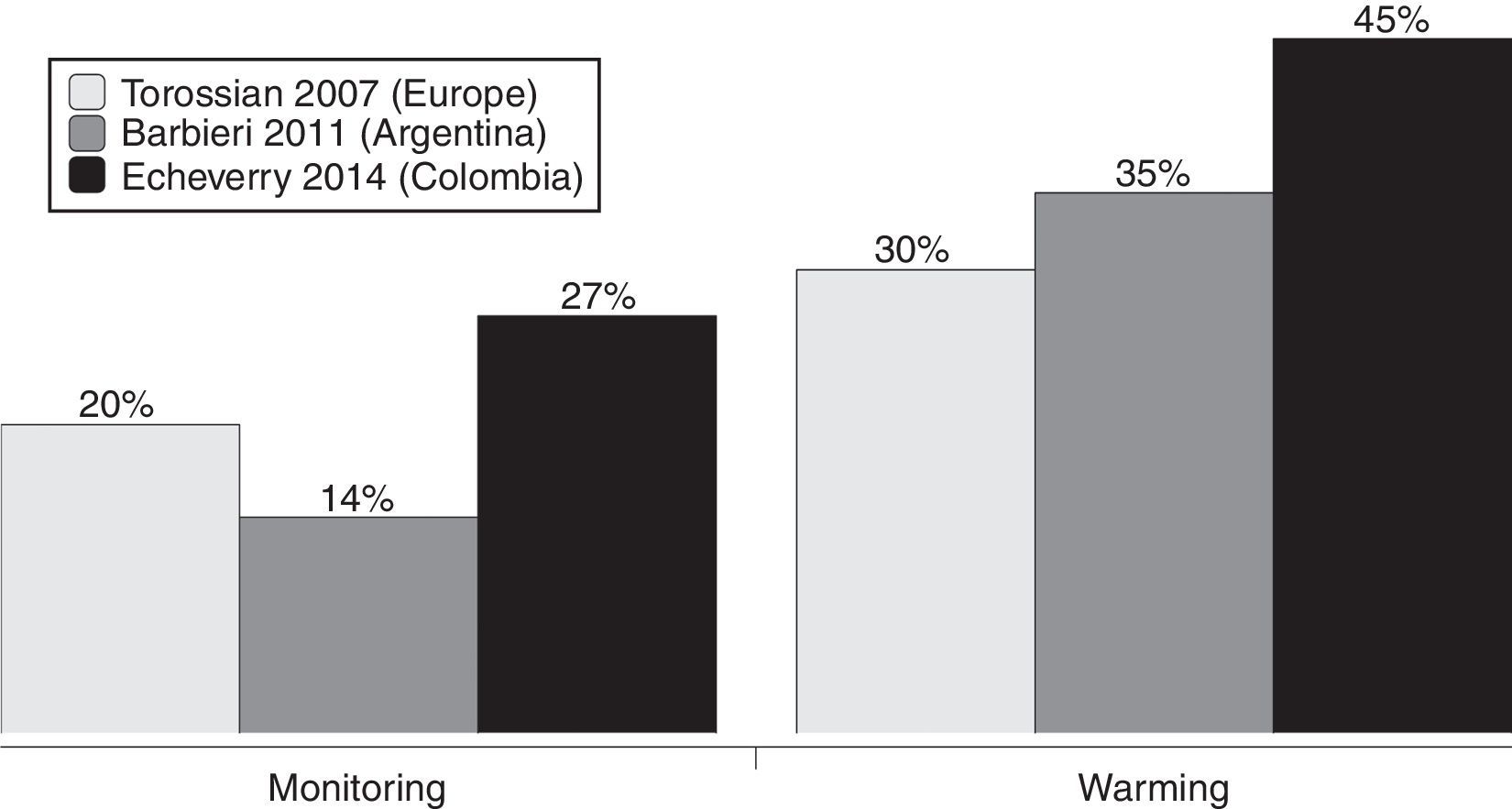
Some surveys have characterized the attitudes of anesthesiologists toward perioperative hypothermia. In the TEMPP study, performed in Europe, it was found that monitoring of intraoperative core temperature is an uncommon practice (between 6% and 25% of cases) and, as a consequence, the use of active warming methods is insufficient.14 An Argentine study found that only 14% of anesthesiologists use routine temperature monitoring, and between 30% and 40% use active warming methods.15
The main objective of this survey is to determine the situation of intraoperative temperature monitoring in high complexity clinics and hospitals in Colombia, and the degree of adherence to the minimum safety standards established by the S.C.A.R.E. with respect to perioperative thermal protection and monitoring.
MethodsAn online, closed, voluntary survey was administered via email to the leaders of anesthesiology departments and surgical services of high complexity clinics and hospitals in Colombia. The study was approved by the scientific subdirectorate of the S.C.A.R.E.’s department of research and the ethics committee of the Faculty of Medicine of the Universidad Nacional de Colombia (minutes: 016-160-15).
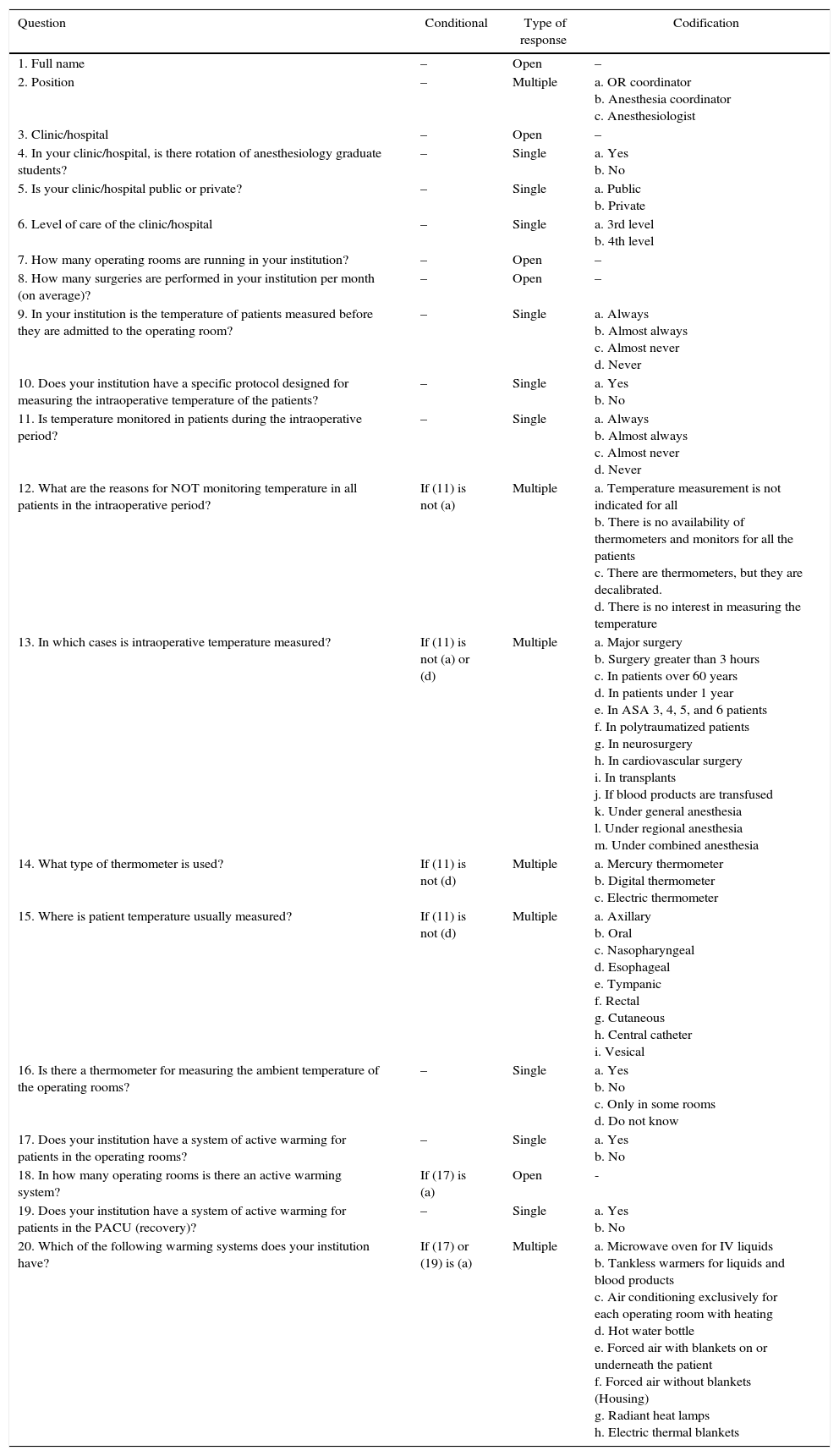
An adaptive questionnaire (with conditional items) was designed to reduce the number and the complexity of the questions (Appendix A). The questionnaire was developed through a process of discussion and consensus among three researchers (PE, DARV, AGMC). Once designed, it was submitted to a process of evaluation of user-friendliness and technical functionality before being sent to the participants. The complete questionnaire contained 20 items, distributed across four screens. Four or five items were included in each screen.
The invitations were sent in an email to a random and stratified sampling of leaders of departments of anesthesiology and surgical services. No other method was used for the divulgation of the survey. Stratification was by geographical region. The domain was taken from the database of high complexity clinics and hospitals of the special record of health services of the Directory for Health Service Provision and First Aid of the Ministry of Health and Social Protection of Colombia (available at: http://201.234.78.38/habilitacion/). The database was consulted in May, 2012. The logistic coordination of the East, Coffee Zone, Southwest, and Atlantic Coast regions was handled from Bogotá, Medellín, Cali, and Barranquilla, respectively, and was the responsibility of at least one researcher per region. The message that each participant received informed them of the estimated time required to complete the survey, the data management and storage procedures, the identity of the research group, and the purpose of the study. All participants received the same message. Implied consent from the participants was assumed if they responded to the survey with knowledge of this information. Respondents received no economic or material incentive for their participation.
By email, the participants received a link to an Internet system that took the identity information of each of the survey participants and stored the information automatically. This record prevented the submission of two or more survey entries by one participant. The information system encuestafacil.com was used. This website did not provide the survey participants with any information about clinical thermometry or body warming methods. The system allowed the participants to review and change their responses before submitting the questionnaire. Furthermore, it guaranteed that only completed questionnaires could be submitted. All participants responded to the same questionnaire. Each survey participant had one week to finish the questionnaire. Since the personal data of the participants was collected, a password protected account was used, accessible only by one person responsible for keeping the password. The writing of the final manuscript of the questionnaire followed the CHERRIES recommendations.16
Statistical aspectsA sample of 168 participants was calculated, considering a reliability of 95% and a margin of error of 5% in a domain of 298 high complexity clinics and hospitals. Statistical tests were not used to corroborate the reliability of the instrument. Proportions were used for the description of the categorical items, and for the description of numeric items medians and ranges were used. Only completed surveys were analyzed.
ResultsA total of 176 invitations to participate in the survey were sent out. Of these, 135 (77%) completed the questionnaire. Four responses were excluded for being incomplete. The data were collected over a period of two months. The usual time for the completing of the survey was one day. The margin of error for the results obtained varied between 3.5% and 6.3% per item.
89% of the participants are heads of departments of anesthesiology, while 20% are coordinators of operating rooms. In other words, 9% exercise both functions.
All of the data were analyzed by subgroups, depending on whether they came from clinics and hospitals with or without a teaching-service agreement (TSA). Later, it was decided that Fisher's exact test would be applied in order to reject the null hypothesis of no difference between the subgroups. This statistical test was applied to the items regarding the measurement of intraoperative temperature and the availability of thermal protection in operating rooms (Table 1). For the other items, no tests were applied in order to avoid problems of statistical multiplicity.17
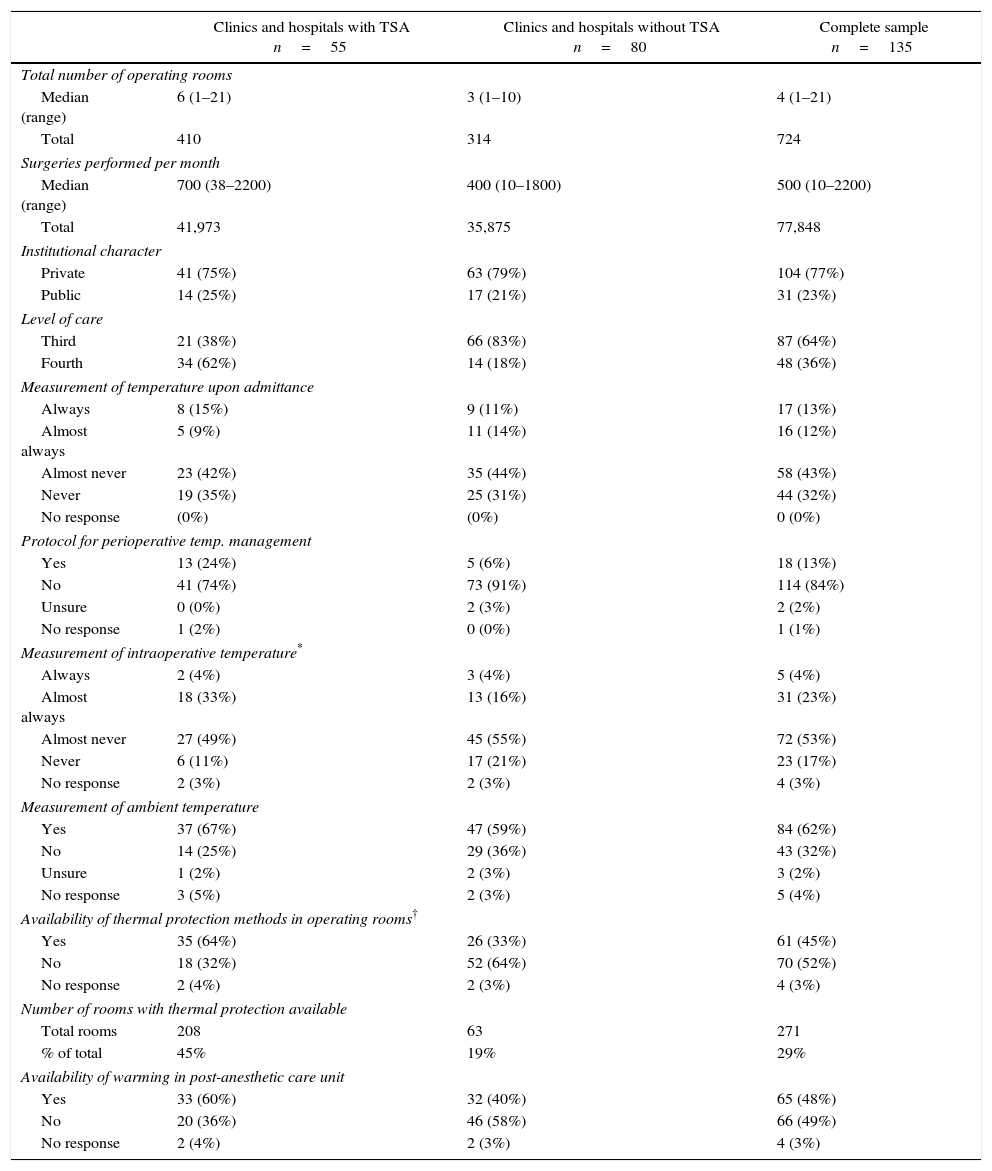
Characterization of the participating clinics and hospitals and the attitudes toward perioperative thermal monitoring and protection.
| Clinics and hospitals with TSA n=55 | Clinics and hospitals without TSA n=80 | Complete sample n=135 | |
|---|---|---|---|
| Total number of operating rooms | |||
| Median (range) | 6 (1–21) | 3 (1–10) | 4 (1–21) |
| Total | 410 | 314 | 724 |
| Surgeries performed per month | |||
| Median (range) | 700 (38–2200) | 400 (10–1800) | 500 (10–2200) |
| Total | 41,973 | 35,875 | 77,848 |
| Institutional character | |||
| Private | 41 (75%) | 63 (79%) | 104 (77%) |
| Public | 14 (25%) | 17 (21%) | 31 (23%) |
| Level of care | |||
| Third | 21 (38%) | 66 (83%) | 87 (64%) |
| Fourth | 34 (62%) | 14 (18%) | 48 (36%) |
| Measurement of temperature upon admittance | |||
| Always | 8 (15%) | 9 (11%) | 17 (13%) |
| Almost always | 5 (9%) | 11 (14%) | 16 (12%) |
| Almost never | 23 (42%) | 35 (44%) | 58 (43%) |
| Never | 19 (35%) | 25 (31%) | 44 (32%) |
| No response | (0%) | (0%) | 0 (0%) |
| Protocol for perioperative temp. management | |||
| Yes | 13 (24%) | 5 (6%) | 18 (13%) |
| No | 41 (74%) | 73 (91%) | 114 (84%) |
| Unsure | 0 (0%) | 2 (3%) | 2 (2%) |
| No response | 1 (2%) | 0 (0%) | 1 (1%) |
| Measurement of intraoperative temperature* | |||
| Always | 2 (4%) | 3 (4%) | 5 (4%) |
| Almost always | 18 (33%) | 13 (16%) | 31 (23%) |
| Almost never | 27 (49%) | 45 (55%) | 72 (53%) |
| Never | 6 (11%) | 17 (21%) | 23 (17%) |
| No response | 2 (3%) | 2 (3%) | 4 (3%) |
| Measurement of ambient temperature | |||
| Yes | 37 (67%) | 47 (59%) | 84 (62%) |
| No | 14 (25%) | 29 (36%) | 43 (32%) |
| Unsure | 1 (2%) | 2 (3%) | 3 (2%) |
| No response | 3 (5%) | 2 (3%) | 5 (4%) |
| Availability of thermal protection methods in operating rooms† | |||
| Yes | 35 (64%) | 26 (33%) | 61 (45%) |
| No | 18 (32%) | 52 (64%) | 70 (52%) |
| No response | 2 (4%) | 2 (3%) | 4 (3%) |
| Number of rooms with thermal protection available | |||
| Total rooms | 208 | 63 | 271 |
| % of total | 45% | 19% | 29% |
| Availability of warming in post-anesthetic care unit | |||
| Yes | 33 (60%) | 32 (40%) | 65 (48%) |
| No | 20 (36%) | 46 (58%) | 66 (49%) |
| No response | 2 (4%) | 2 (3%) | 4 (3%) |
Clinics and hospitals with TSA corresponded to 40% of the sample, and were generally larger with an average of six operating rooms in service, and an average of 700 surgeries per month. They also had a higher level of complexity of care, since they offered cardiovascular surgery services, solid organ and bone marrow transplants. As such, they classified as fourth level of care (62% of clinics and hospitals with TSA, compared to 18% of clinics and hospitals without TSA). In both groups, the majority of the clinics and hospitals were private (77%). The measurement of intraoperative temperature is performed always or almost always in 37% of TSA clinics and hospitals, and in 20% of clinics and hospitals without TSA (p=0.154).
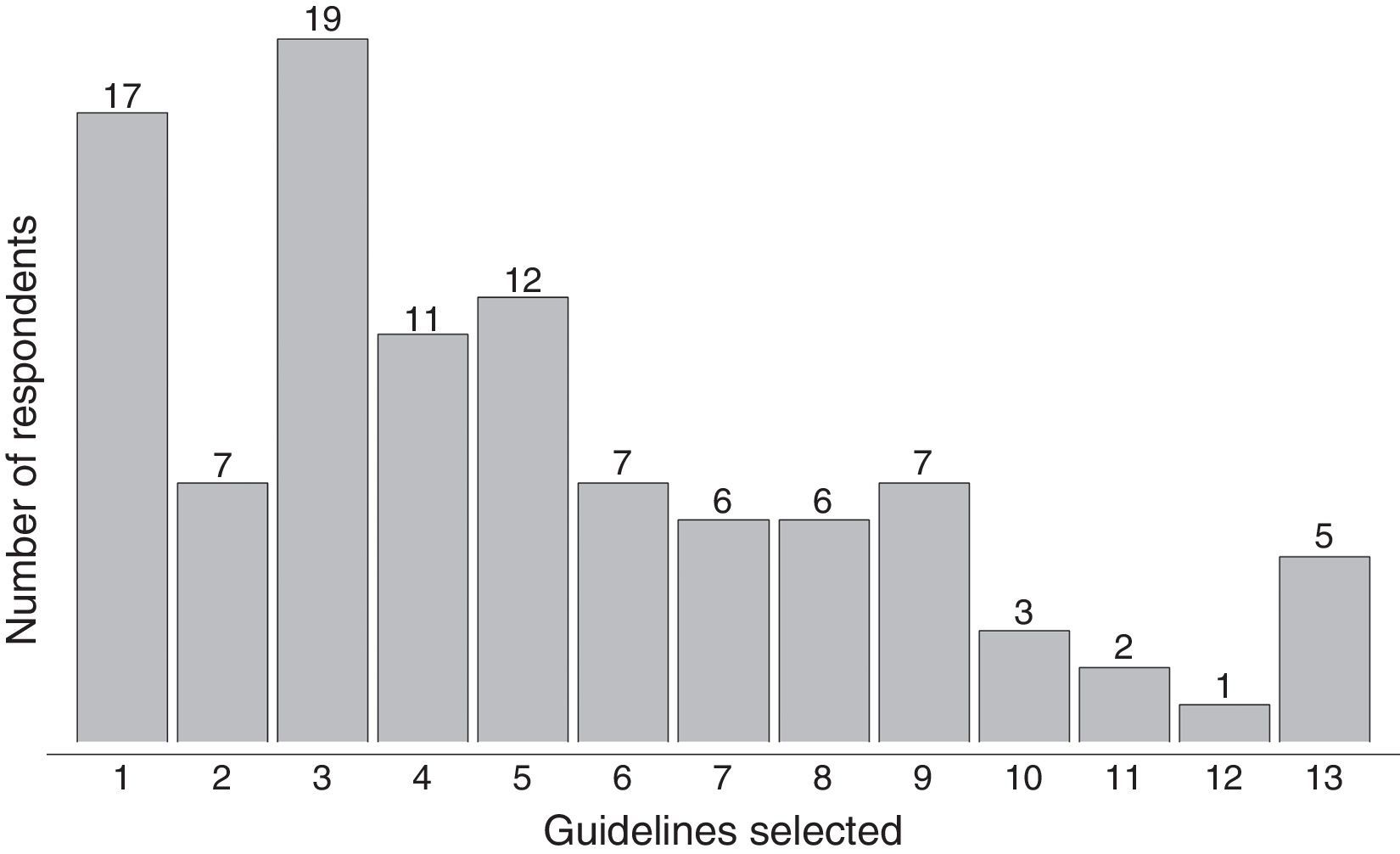
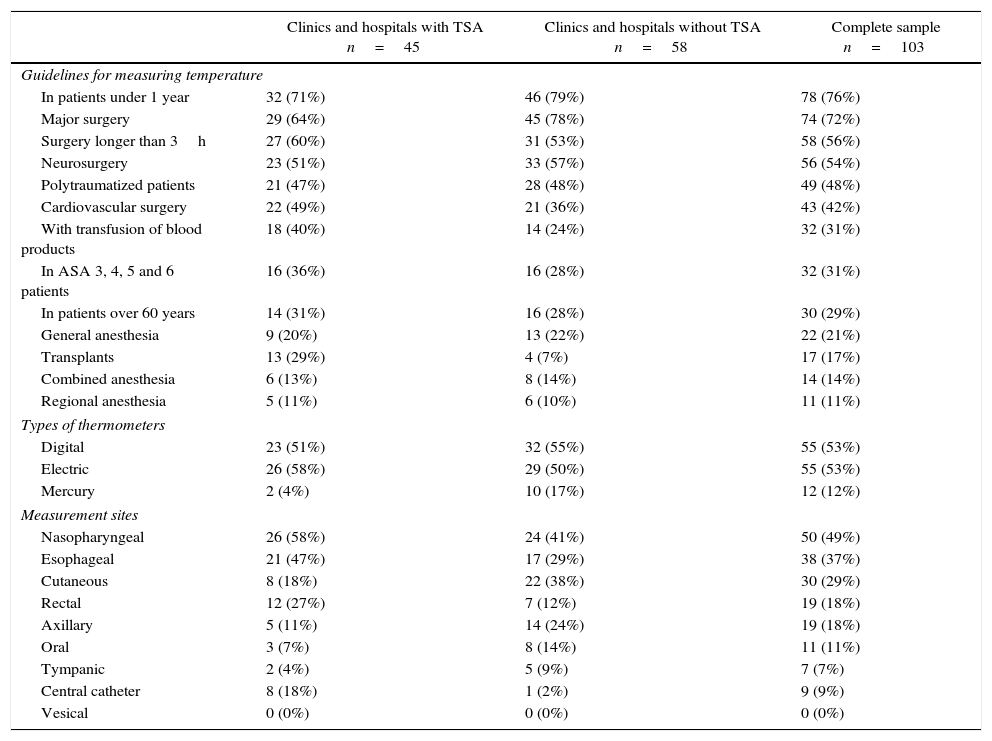
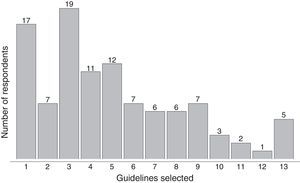
That characterization of the participating clinics and hospitals, and the attitudes of the survey respondents about perioperative thermal monitoring and protection are described in Table 1. The temperature monitoring guidelines, devices and sites used by the respondents are described in Table 2. Five of the respondents identified all of the options available as intraoperative temperature monitoring guidelines used in clinical practice (Fig. 1).
Intraoperative temperature monitoring guidelines, devices, and sites.
| Clinics and hospitals with TSA n=45 | Clinics and hospitals without TSA n=58 | Complete sample n=103 | |
|---|---|---|---|
| Guidelines for measuring temperature | |||
| In patients under 1 year | 32 (71%) | 46 (79%) | 78 (76%) |
| Major surgery | 29 (64%) | 45 (78%) | 74 (72%) |
| Surgery longer than 3h | 27 (60%) | 31 (53%) | 58 (56%) |
| Neurosurgery | 23 (51%) | 33 (57%) | 56 (54%) |
| Polytraumatized patients | 21 (47%) | 28 (48%) | 49 (48%) |
| Cardiovascular surgery | 22 (49%) | 21 (36%) | 43 (42%) |
| With transfusion of blood products | 18 (40%) | 14 (24%) | 32 (31%) |
| In ASA 3, 4, 5 and 6 patients | 16 (36%) | 16 (28%) | 32 (31%) |
| In patients over 60 years | 14 (31%) | 16 (28%) | 30 (29%) |
| General anesthesia | 9 (20%) | 13 (22%) | 22 (21%) |
| Transplants | 13 (29%) | 4 (7%) | 17 (17%) |
| Combined anesthesia | 6 (13%) | 8 (14%) | 14 (14%) |
| Regional anesthesia | 5 (11%) | 6 (10%) | 11 (11%) |
| Types of thermometers | |||
| Digital | 23 (51%) | 32 (55%) | 55 (53%) |
| Electric | 26 (58%) | 29 (50%) | 55 (53%) |
| Mercury | 2 (4%) | 10 (17%) | 12 (12%) |
| Measurement sites | |||
| Nasopharyngeal | 26 (58%) | 24 (41%) | 50 (49%) |
| Esophageal | 21 (47%) | 17 (29%) | 38 (37%) |
| Cutaneous | 8 (18%) | 22 (38%) | 30 (29%) |
| Rectal | 12 (27%) | 7 (12%) | 19 (18%) |
| Axillary | 5 (11%) | 14 (24%) | 19 (18%) |
| Oral | 3 (7%) | 8 (14%) | 11 (11%) |
| Tympanic | 2 (4%) | 5 (9%) | 7 (7%) |
| Central catheter | 8 (18%) | 1 (2%) | 9 (9%) |
| Vesical | 0 (0%) | 0 (0%) | 0 (0%) |
Listed in order of frequency. The sum of the percentages does not add to 100% due to questions with multiple response options.
ASA=ASA (American Society of Anesthesiologists) physical state classification; TSA=teaching-service agreement.
Source: Authors.
With regard to the guidelines for monitoring temperature in operating rooms, only five of the respondents selected all 13 guidelines provided. The rest only selected a few. Of these, the most frequently selected were: patients under 1 year or age, major surgery, surgery lasting more than three hours, polytraumatized patients, and neurosurgery (Table 2).
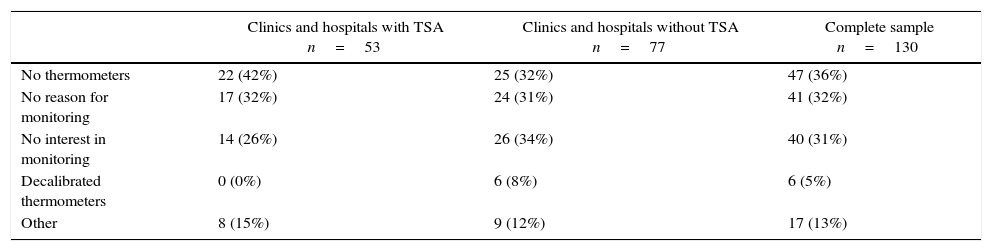
The reasons that the respondents identified as barriers to intraoperative temperature monitoring are described in Table 3. The perioperative warming methods used are described in Table 4.
Barriers to intraoperative temperature monitoring.
| Clinics and hospitals with TSA n=53 | Clinics and hospitals without TSA n=77 | Complete sample n=130 | |
|---|---|---|---|
| No thermometers | 22 (42%) | 25 (32%) | 47 (36%) |
| No reason for monitoring | 17 (32%) | 24 (31%) | 41 (32%) |
| No interest in monitoring | 14 (26%) | 26 (34%) | 40 (31%) |
| Decalibrated thermometers | 0 (0%) | 6 (8%) | 6 (5%) |
| Other | 8 (15%) | 9 (12%) | 17 (13%) |
Listed in order of frequency. The sum of the percentages does not correspond to 100% due to the option to select multiple responses.
TSA=teaching-service agreement.
Source: Authors.
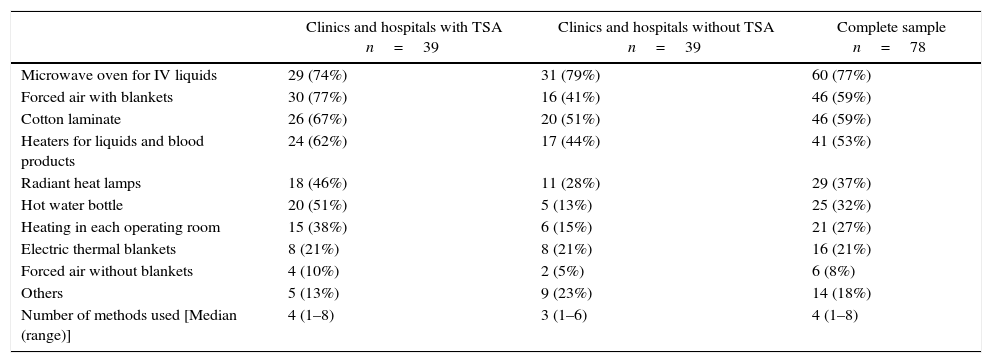
Perioperative warming methods.
| Clinics and hospitals with TSA n=39 | Clinics and hospitals without TSA n=39 | Complete sample n=78 | |
|---|---|---|---|
| Microwave oven for IV liquids | 29 (74%) | 31 (79%) | 60 (77%) |
| Forced air with blankets | 30 (77%) | 16 (41%) | 46 (59%) |
| Cotton laminate | 26 (67%) | 20 (51%) | 46 (59%) |
| Heaters for liquids and blood products | 24 (62%) | 17 (44%) | 41 (53%) |
| Radiant heat lamps | 18 (46%) | 11 (28%) | 29 (37%) |
| Hot water bottle | 20 (51%) | 5 (13%) | 25 (32%) |
| Heating in each operating room | 15 (38%) | 6 (15%) | 21 (27%) |
| Electric thermal blankets | 8 (21%) | 8 (21%) | 16 (21%) |
| Forced air without blankets | 4 (10%) | 2 (5%) | 6 (8%) |
| Others | 5 (13%) | 9 (23%) | 14 (18%) |
| Number of methods used [Median (range)] | 4 (1–8) | 3 (1–6) | 4 (1–8) |
Listed in order of frequency. The sum of the percentages does not correspond to 100% due to the option to select multiple responses.
TSA=teaching-service agreement.
Source: Authors.
Of 298 high complexity clinics and hospitals in Colombia, 176 were selected to respond to the survey and thereby obtain a level of reliability of 95% with a margin of error 5%. The questionnaire was completed by 77% of those contacted within an acceptable period of time. With this sample, a margin of error of between 3 and 6.5% was obtained, which is to be expected giving the size of the sample.
In this sample, it was found that temperature is always measured at patient admittance in 15% of the clinics and hospitals with TSA, and in 11% of the clinics and hospitals without TSA. What is surprising about this finding is that, despite the fact that preoperative monitoring is an infrequent practice, it is more common than intraoperative monitoring, since this is only performed always in 4% of the clinics and hospitals studied. This leads us to suppose that the temperature is measured at the admittance of the patients when their life signs are recorded, usually as part of nursing care, but once they have entered the operating room, patient temperature is not monitored by the anesthesiologists.
The warming strategies are available in the operating rooms in 64% of the clinics and hospitals with TSA and in 33% of the clinics and hospitals without TSA. When asked about the availability of these devices in the post-anesthetic care units (PACU), it was found that they were available in 60% of clinics and hospitals with TSA and in 40% of the clinics and hospitals without TSA. The most common warming strategies were microwave ovens, forced air with blankets, cotton laminate, tankless heaters for liquids and blood products, and radiant heat lamps (Table 4). It should be highlighted that, of these alternatives, the microwave oven and the cotton laminate are passive warming strategies.18,19
Although the TSA clinics and hospitals have better indications with regard to perioperative temperature monitoring, they continue to be insufficient, which leads us to believe that, from the academic and educational point of view, there is no strict commitment toward or an adequate awareness of perioperative hypothermia among teaching and instructional anesthesiologists. With respect to the contrast in the numbers regarding the availability of a protocol for the management and prevention of perioperative hypothermia (13%) and routine temperature monitoring, it can be supposed that anesthesiologists disregard the guidelines established by the state, the S.C.A.R.E., and by the clinics and hospitals themselves.
The other important aspect to consider is the measurement of ambient temperature, which occurs in 67% of the clinics and hospitals with TSA and 59% of the non-TSA clinics and hospitals. This finding is worrying, considering that the measurement of ambient temperature in the operating rooms is obligatory according to the guidelines for authorizing the provision of health services. Reasons that may explain this result include the existence of faults in the implementation of the guidelines in the operating rooms, ignorance of the guidelines, or ignorance from surveyed anesthesiologists of the presence of thermometers in the operating rooms.
The availability of warming methods is more frequent than temperature monitoring. This indicates that thermal protection of patients is done blindly, without knowledge of their temperature. The case of the PACU is no different, since it is more difficult to manage temperature post-operatively, where then permanent measurement of the central temperature is less feasible, and in most cases only peripheral temperature thermometers are available. In these cases, the thermal protection strategies are guided by subjective methods of measurement such as the patient feeling cold, the presence of shivering, and skin temperature, especially in the extremities.
The results also show that the measurement of intraoperative temperature is always or almost always done in 27% of the clinics and hospitals surveyed. This contrasts with the behavior of this indicator in other surveys performed in Europe, where it is around 20%,14 and in Argentina 14%.15 Warming strategies are available in 45% of clinics and hospitals in Colombia, 30% in Europe, and 35% in Argentina (Fig. 2).14,15 It appears that this attitude toward temperature monitoring and control is global, since several studies have shown consistencies between local, regional, and international practices.5,6,14,15
All of the findings of this study are alarming if the adverse effects associated with hypothermia are considered along with the fact that anesthesiologists are conscious of the importance of avoiding and correcting unnoticed hypothermia in operating rooms, especially in high-risk patients or those undergoing major surgery.20,21
All of the above should be analyzed with the knowledge that, in addition to the minimum safety guidelines of the S.C.A.R.E., the single approval system in Colombia (resolution 1043 of 2006 of the Ministry of Health and Social Protection of Colombia), which establishes the conditions that health service providers must comply with in order to legally provide services, indicates that central temperature monitoring must be present when surgery is done on newborns and children, as well as for cardiovascular surgery, trauma surgery, and procedures lasting more than three hours. In addition, they stipulate that warming systems for the rapid infusion of liquids and blood products must be available. With respect to the ideal moment for measuring temperature, the NICE guides recommend that it should be measured before patients enter the operating room and that, if the patient has a central temperature below 37°C, surgery should be postponed in order to initiate the active warming process until achieving a temperature above that value.22 This practice provides a safety range for avoiding moderate or severe hypothermia after the induction of anesthesia since a patient's central temperature may drop by between 1 and 1.5°C in the first hour of surgery, quickly leading to hypothermia.23
LimitationsThis study has limitations related to the veracity of the information obtained from the survey that depends completely on the respondents and their interest in reporting better adherence to practices in their surgical service. Furthermore, since it is a voluntary survey, a selection bias may be present, since it is probable that those who responded to the questionnaire are more interested in the subject and, therefore, the survey may overestimate the performance of the high-complexity clinics and hospitals in terms of temperature monitoring and perioperative thermal protection in Colombia.
ConclusionsIn summary, this survey shows an evident reality regarding the low level of perioperative temperature management, the lack of interest in thermal protection for patients undergoing surgery, and the inadequate and irrational use of active warming techniques in high-complexity clinics and hospitals in Colombia. There is little adherence to the knowledge and minimal safety guidelines of the S.C.A.R.E.13 This leads us to conclude that there is no situational awareness, that the adverse effects from hypothermia in patients submitted to surgery are not prevented, and that there is no culture of safety.
Less than half of the clinics and hospitals measure patient temperature in the perioperative period. The reasons for this are the low availability of thermometers and the lack of interest in the subject of perioperative hypothermia. Although the panorama is worrying, it is no different from the attitude of anesthesiologists in other countries in which similar surveys have been performed. This study opens up new expectations with respect to inadvertent perioperative hypothermia in Colombia, since it calls for thinking about practices and policies aimed at improving the adherence to the safety guidelines of the S.C.A.R.E. and the approval norms established by the state control organisms.
Ethical approvalProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis study was financed by the Colombian Society of Anesthesiology and Resuscitation (S.C.A.R.E.) and 3M.
Conflict of interestsAll of the authors completed a form for the identification of conflicts of interests (available at www.icmje.org/coi_disclosure.pdf) and declared that PE, DARV, GHR and JHRE received honorariums for their participation in this study; AGMC is an employee of 3M Colombia, and PE has given conferences in 3M Colombia's educational programs. The 3M Company is a multinational company that sells devices for perioperative thermal protection.
| Question | Conditional | Type of response | Codification |
|---|---|---|---|
| 1. Full name | – | Open | – |
| 2. Position | – | Multiple | a. OR coordinator b. Anesthesia coordinator c. Anesthesiologist |
| 3. Clinic/hospital | – | Open | – |
| 4. In your clinic/hospital, is there rotation of anesthesiology graduate students? | – | Single | a. Yes b. No |
| 5. Is your clinic/hospital public or private? | – | Single | a. Public b. Private |
| 6. Level of care of the clinic/hospital | – | Single | a. 3rd level b. 4th level |
| 7. How many operating rooms are running in your institution? | – | Open | – |
| 8. How many surgeries are performed in your institution per month (on average)? | – | Open | – |
| 9. In your institution is the temperature of patients measured before they are admitted to the operating room? | – | Single | a. Always b. Almost always c. Almost never d. Never |
| 10. Does your institution have a specific protocol designed for measuring the intraoperative temperature of the patients? | – | Single | a. Yes b. No |
| 11. Is temperature monitored in patients during the intraoperative period? | – | Single | a. Always b. Almost always c. Almost never d. Never |
| 12. What are the reasons for NOT monitoring temperature in all patients in the intraoperative period? | If (11) is not (a) | Multiple | a. Temperature measurement is not indicated for all b. There is no availability of thermometers and monitors for all the patients c. There are thermometers, but they are decalibrated. d. There is no interest in measuring the temperature |
| 13. In which cases is intraoperative temperature measured? | If (11) is not (a) or (d) | Multiple | a. Major surgery b. Surgery greater than 3 hours c. In patients over 60 years d. In patients under 1 year e. In ASA 3, 4, 5, and 6 patients f. In polytraumatized patients g. In neurosurgery h. In cardiovascular surgery i. In transplants j. If blood products are transfused k. Under general anesthesia l. Under regional anesthesia m. Under combined anesthesia |
| 14. What type of thermometer is used? | If (11) is not (d) | Multiple | a. Mercury thermometer b. Digital thermometer c. Electric thermometer |
| 15. Where is patient temperature usually measured? | If (11) is not (d) | Multiple | a. Axillary b. Oral c. Nasopharyngeal d. Esophageal e. Tympanic f. Rectal g. Cutaneous h. Central catheter i. Vesical |
| 16. Is there a thermometer for measuring the ambient temperature of the operating rooms? | – | Single | a. Yes b. No c. Only in some rooms d. Do not know |
| 17. Does your institution have a system of active warming for patients in the operating rooms? | – | Single | a. Yes b. No |
| 18. In how many operating rooms is there an active warming system? | If (17) is (a) | Open | - |
| 19. Does your institution have a system of active warming for patients in the PACU (recovery)? | – | Single | a. Yes b. No |
| 20. Which of the following warming systems does your institution have? | If (17) or (19) is (a) | Multiple | a. Microwave oven for IV liquids b. Tankless warmers for liquids and blood products c. Air conditioning exclusively for each operating room with heating d. Hot water bottle e. Forced air with blankets on or underneath the patient f. Forced air without blankets (Housing) g. Radiant heat lamps h. Electric thermal blankets |
Source: Authors.
Please cite this article as: Echeverry-Marín PC, Rincón-Valenzuela DA, Monroy-Charry AG, Ruiz-Villa JO, Higuera-Redondo G, Rubio-Elorza JH. Survey about attitudes on perioperative temperature monitoring and thermal protection in Colombia. Rev Colomb Anestesiol. 2016;44:282–291.