Surgical thinking around errors and patient safety has changed dramatically over the past 15 years. The relevance of effective teamwork, both within the operating theatre but also across the entire perioperative pathway, is acknowledged as a critical component of safe and effective surgical care, resulting in good outcomes and quick recovery for the surgical patient.1 Consequently, significant efforts have been made to understand how teams work within surgical care pathways and how to improve teamwork.
The study by Amaya A,2 and colleagues reported in this issue of the Journal is one such well-articulated attempt. The authors report a detailed approach to evaluating surgical and obstetric teams at baseline, then introducing a complex team-based intervention, and finally re-evaluating these teams to establish whether their team effectiveness improved. It is refreshing to see an integrated approach to team training taken here: the authors utilised elements of well-established team programmes (TeamSTEPPS) and approaches to team working (systems approach, crisis resource management principles (CRM)). They also integrated the theory with practical tools, like the WHO Checklist adapted for local application and team briefings/debriefings. On the evaluation side, it is encouraging to see an attempt to implement a psychometrically solid approach to team evaluation, using a culturally adapted instrument in the form of the ‘Observational Teamwork Assessment for Surgery – Spanish version’ (OTAS-S) applied by trained evaluators. Amaya Arias et al. reported positive results – they found that their teams exhibited better team behaviours, especially in areas such as leadership and team situation awareness where deficiencies were identified at baseline. Not least, it is important that this improvement intervention was carried out in Colombian theatres – i.e. outside the ‘usual suspects’, large US, UK, or Australian university hospitals that are typically well-resourced.
‘Teams create safety’In the past, when things went wrong in surgery, almost instinctively the technical skills of the operating surgeon were questioned and scrutinised. Completely overlooked were the ‘softer’ non-technical (social and cognitive) skills of both the surgeon but also the wider team – including the anaesthetist and nurses in theatre. Over the past 15 years, the conceptualisation of surgical safety has significantly changed; there is growing awareness that the skills required to consistently achieve safe surgery extend well beyond the technical knowledge and skills of the operating surgeon.3 Teamwork, defined as a ‘set of interrelated behaviours, actions, cognitions and attitudes that facilitate the required task work that must be completed’,4 is increasingly regarded as an essential component of safe surgery. Teams are essential when ‘errors lead to severe consequences; when the task complexity exceeds the capacity of an individual; when the task environment is ill defined, ambiguous, and stressful; when multiple and quick decisions are needed; and when the lives of others depend on the collective insight of individual members’.5 The importance of teamwork to safety and efficiency of operations has long been recognised and consequently embedded into the education, training and assessment of workers in many industries.6 The concept that ‘teams create safety’ 7 is finally appearing to be embraced by the healthcare community.
Teamwork assessment: the foundation for improvementThe old management adage ‘you can’t manage what you don’t measure’ is very appropriate when discussing team effectiveness and teamwork improvement in any industry, including healthcare. How are we to improve team function if the subject matter remains nebulous and ill-defined? It follows that the ability to evaluate with accuracy and validity the team skills of operating theatre teams is a foundation for improvement and a prerequisite to integrating teamwork into training and work-place based assessments. Team assessment provides a means of structuring feedback to team-members (including trainees), identifying and prioritising training needs, and determining the effectiveness of training interventions (such as the one reported by Amaya Arias et al.). A large amount of research to date has been devoted to identifying the key non-technical skills required for safe and effective team function in the perioperative setting and the development of assessment instruments designed specifically to capture the quality of these skills. Attempts to identify how perioperative teamwork is understood and applies across different national settings,8,9 and efforts to develop guidelines for training faculty to evaluate their teams, and implement team training have recently began to emerge in the literature.10
Teamwork training: the vehicle for improvementSimply bringing together experts does not ensure that they will merge into an expert team. Coupled with existing evidence suggesting that teamwork in the operating theatre, at times, is far from harmonious or effective, the importance of training theatre teams to work effectively together is gaining international acceptance as a key strategy to maximise surgical safety. The development of team training interventions, to provide theatre teams with the knowledge, skills, and attitudes (KSAs) that underpin effective team performance, has become an increasingly prominent feature in the surgical, anaesthetic, and nursing literatures. Indeed, anaesthesia has been described as a leading medical speciality in addressing issues surrounding adverse events – as the discipline was one of the first to discover and embrace CRM and teamwork training more than 20 years ago. Other interventional specialties, like surgery and obstetrics followed – a trend that was facilitated by the development of high-fidelity training models and simulators.
The three most common training strategies employed to deliver training are information based (e.g. lecture/workshop based), demonstration based (trainees observe the required skills e.g. videos) and practice based (e.g. role play, hands-on-practice, simulation). Simulation-based training has become increasingly popular in the perioperative setting (and indeed elsewhere) to deliver skills training. Simulation has been suggested as an attractive and complementary training environment to clinical practice, offering the advantage of allowing teams to learn teamwork skills in an structured and tailored learning environment, where ‘permission to fail’ is granted and mistakes do not jeopardise patient safety. The evidence shows that multidisciplinary simulations offer a valuable strategy to improve operating theatre teamwork.
An often asked question is how effective team training is in imparting skills and, ultimately, in improving patient outcomes. Given the considerable financial and organisational burden of initiating (cost and difficulty of releasing staff to attend team training) and sustaining training (recurrent training, refresher courses and reinforcement of training) this is a fair question – evidence supporting the effectiveness of training is essential for widespread adoption. On the surface, the question as to whether team training ‘works’ is deceptively simple. In reality, evaluating the effectiveness of team training is complex and depends not only on how ‘effectiveness’ is defined but also on the availability of suitable metrics to assess effectiveness accurately.
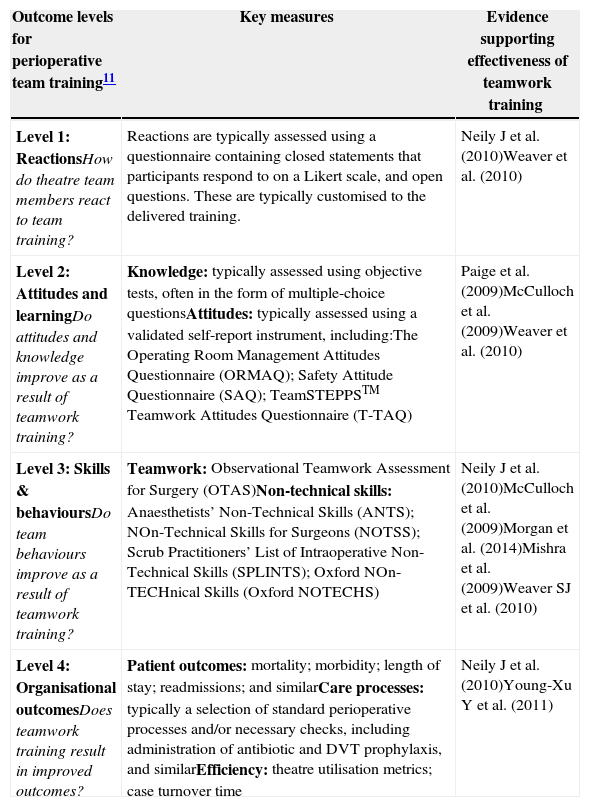
Overall, the short answer to whether team training is effective is ‘yes’. The more nuanced answer requires an understanding of how a complex training intervention may work. Kirkpatrick11 provides a well-established, useful framework for understanding the impact of perioperative team training across 4 evaluation levels. Table 1 provides a brief overview of the evidence base using Kirkpatrick's outcome framework.
Detailed evaluation of the effectiveness of perioperative team training – outcome levels, related measures and the evidence base.
| Outcome levels for perioperative team training11 | Key measures | Evidence supporting effectiveness of teamwork training |
|---|---|---|
| Level 1: ReactionsHow do theatre team members react to team training? | Reactions are typically assessed using a questionnaire containing closed statements that participants respond to on a Likert scale, and open questions. These are typically customised to the delivered training. | Neily J et al. (2010)Weaver et al. (2010) |
| Level 2: Attitudes and learningDo attitudes and knowledge improve as a result of teamwork training? | Knowledge: typically assessed using objective tests, often in the form of multiple-choice questionsAttitudes: typically assessed using a validated self-report instrument, including:The Operating Room Management Attitudes Questionnaire (ORMAQ); Safety Attitude Questionnaire (SAQ); TeamSTEPPSTM Teamwork Attitudes Questionnaire (T-TAQ) | Paige et al. (2009)McCulloch et al. (2009)Weaver et al. (2010) |
| Level 3: Skills & behavioursDo team behaviours improve as a result of teamwork training? | Teamwork: Observational Teamwork Assessment for Surgery (OTAS)Non-technical skills: Anaesthetists’ Non-Technical Skills (ANTS); NOn-Technical Skills for Surgeons (NOTSS); Scrub Practitioners’ List of Intraoperative Non-Technical Skills (SPLINTS); Oxford NOn-TECHnical Skills (Oxford NOTECHS) | Neily J et al. (2010)McCulloch et al. (2009)Morgan et al. (2014)Mishra et al. (2009)Weaver SJ et al. (2010) |
| Level 4: Organisational outcomesDoes teamwork training result in improved outcomes? | Patient outcomes: mortality; morbidity; length of stay; readmissions; and similarCare processes: typically a selection of standard perioperative processes and/or necessary checks, including administration of antibiotic and DVT prophylaxis, and similarEfficiency: theatre utilisation metrics; case turnover time | Neily J et al. (2010)Young-Xu Y et al. (2011) |
Source: Authors
Effective teamwork in the operating theatre is a necessity, not a luxury – better teams have better outcomes. In spite of the increasing recognition of the importance of teamwork to surgical patient safety, and the significant efforts taking place globally to improve team functioning through team training, it is still a common expectation of healthcare professionals to morph effortlessly into an effective team without sufficient team training in place. Availability of regular team training remains limited to a relatively small number of hospitals, typically driven by enthusiastic and committed individuals and often in response to an adverse event. Swaying healthcare providers to invest in team training, is likely to require concerted ongoing effort. This will include additional empirical evidence demonstrating positive impact on outcomes, but also clinical leadership, embedding team training into the early stages of residency curricula, and advocacy efforts on the part of patients and society at large.
FundingHull and Sevdalis are affiliated with the Imperial Patient Safety Translational Research Centre (www.cpssq.org), which is funded by the UK's National Institute for Health Research.
Conflicts of interestHull and Sevdalis deliver regular teamwork and safety training on a consultancy basis in the UK and internationally.
Please cite this article as: Hull L, Sevdalis N. Teamwork and safety in surgery. Rev Colomb Anestesiol. 2015;43:3–6.