The laryngeal mask has become an alternative to manage the pediatric airway. This is a clinical case of an infant with VACTERL association requiring anesthesia for tracheoesophageal fistula closure and esophageal anastomosis; the infant was successfully managed with laryngeal mask upon failed intubation.
The use of the laryngeal mask is an option for the management of the airway in neonates and infants with craniofacial malformations, either alone or as an adjuvant for tracheal intubation and also in neonates with normal airway for complex surgeries, including heart surgery. The evidence points to the use of second-generation devices that allow for an improved airway seal and suction of the GI tract (Proseal® or Supreme®). It is also an alternate device during neonatal resuscitation in patients over 2000g that cannot be properly managed with a face mask or intubated.
La máscara laríngea se ha convertido en una alternativa para el manejo de la vía aérea en el paciente pediátrico. Se presenta un caso clínico de un lactante con asociación VACTER que requiere anestesia para cierre de fistula traqueoesofágica y anastomosis esofágica, el cual no se logra intubar y es manejado exitosamente con una máscara laríngea. El uso de la máscara laríngea es una opción en el manejo de la vía aérea de neonatos y lactantes con malformaciones craneofaciales como manejo único, o como adyuvante para la intubación traqueal, y también en neonatos con vía aérea normal para cirugías complejas, incluso cirugía cardiaca. La evidencia apunta hacia el uso de dispositivos de segunda generación que permiten un mejor sello de la vía aérea y la succión de la vía digestiva (Proseal® o Supreme®). Es también un dispositivo alterno durante la reanimación neonatal en pacientes más de 2.000 g que no se pueden manejar adecuadamente con máscara facial y no pueden ser intubados.
Male patient with a history of prematurity and suspected VACTERL Association: atrial septal defect, esophageal atresia with distal trachea-esophageal fistula, imperforate anus.
The patient was born through cesarean section at 28 weeks due to preterm delivery on September 17, 2011. Birth weight was 1100g, Apgar score 6-8-8, induced neonatal adaptation, tracheal intubation due to respiratory distress. The patient was admitted to the neonatal intensive care unit for comprehensive management. At 2 days of age the infant underwent colostomy and continued hospitalized in the NICU with mechanical ventilation, surfactant administration and dobutamine for inotropic support. At 37 days of age the infant was intervened for trachea-esophageal fistula closure and esophageal anastomosis via thoracotomy. Two days later the infant presented clinical impairment with signs of inflammatory response and required inotropic support. The chest X-ray was compatible with right pleural effusion and pneumothorax. The patient was re-operated and the findings included dehiscence of the esophageal anastomosis in addition to short ends that prevented a re-anastomosis. The decision was to do a cervical esophagectomy with distal end closure, gastrostomy and placement of a right chest tube. The patient continued to be managed at the intensive care unit with adequate clinical evolution, weight gain and progressive weaning of the inotropic support. After three months with mechanical ventilation the patient was extubated, though the requirement for oxygen supplementation persisted, as well as wheezing episodes.
On January 18, the patient was evaluated by anesthesiology for esophagostomy closure and esophageal re-anastomosis. At 4 months of age, corrected gestational age of 46 weeks, the body weight was 4000g and the patient was still hospitalized in basic neonatal care with gastrostomy feeding. Treatment included enalapril, spironolactone, beclometasone, salbutamol and oxygen administered through a nasal tube. The baby had good physical appearance, was active, with mild respiratory distress, pulmonary auscultation with occasional ronchi, cardiac bruit with baseline systolic murmur foci and functional gastrostomy and colostomy. Complete blood count with mild anemia and ECG with sound bi-ventricular function, atrial septal defect with no hemodynamic impact and mild pulmonary hypertension. Surgery was authorized and the patient was classified as ASA 3; a bed and 15cc/kg of red packed cells were reserved in the ICU.
The pre-anesthetic evaluation missed the recent chest thorax review that could have been useful to assess the airway. No fibrolaryngoscope or second-generation laryngeal masks were available then at the IMI.
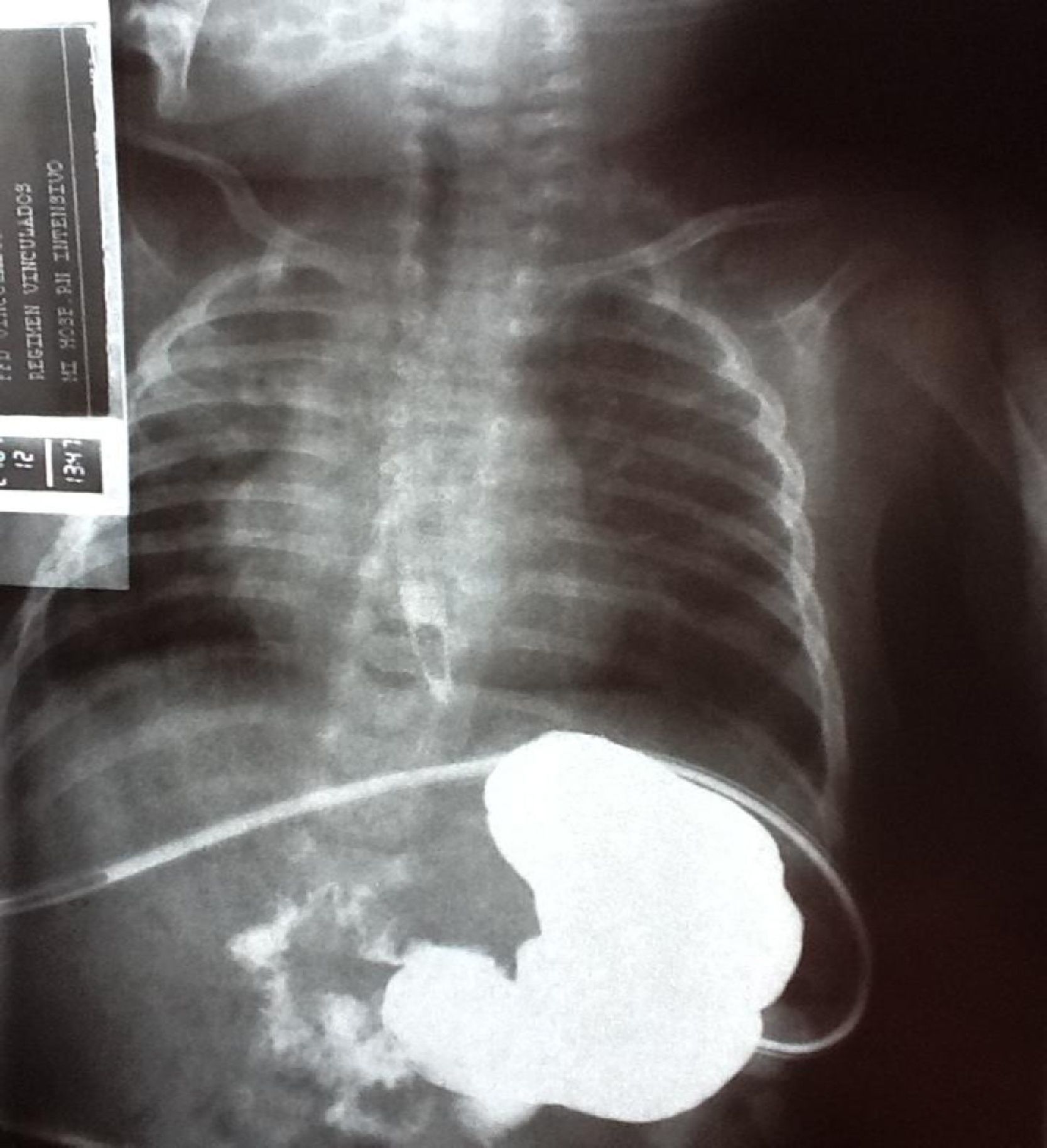
The patient was operated on January 20; the infant was taken to the OR under supplementary oxygen, placed in a radiant-heat cradle and monitored. The initial vital signs were: heart rate 147beats/min, respiratory rate, 26bpm, blood pressure 95/47mmHg and arterial oxygen saturation 91%. Inhaled sevoflurane was used for induction and a right upper limb vein was catheterized with an intravenous 22-gauge catheter. The induction with inhaled sevoflurane was supplemented with propofol 15mg (4mg/kg), remifentanil 15mcg (4mcg/kg) and rocuronium 2mg (0.5mg/kg). Easy facemask ventilation; direct laryngoscopy with straight #blade provided proper glottis visualization. An attempt to insert a #40 tube without pneumoplug but it could not get through beyond the vocal folds; additional tracheal intubation failed attempts were made with #3.5, 3.0 and 2.5. In between the repeated intubation attempts the patient was ventilated using a facial mask, maintaining the oxygen saturation above 90% at all times. Help from a second anesthesiologist was requested, but the patient could not be intubated. The chest X-rays were studied (Fig. 1) and a severe subglottic obstruction was identified and hence the decision was made to place a 1.0 laryngeal mask (Fig. 2), obtaining a satisfactory airway seal (according to the clinical evaluation of manual ventilation), with symmetric ventilation and positive capnography. A switch was made to pressure controlled mechanical ventilation with maximum inspiratory pressure of 18cm H2O, respiratory rate of 18bpm, inspiration–expiration ratio of 1:2. Caudal analgesia was administered and the surgical procedure was initiated. The oxygen saturation and end tidal saturation during the procedure were within the normal range: 96% and 34mmHg, respectively (Fig. 3). The surgery lasted for 2.5h with no complications. The patient was transferred to the neonatal intensive care unit (NICU) with the laryngeal mask and spontaneous breathing. The patient was delivered to the NICU in a stable condition, with no respiratory distress and adequate oxygenation (96%): the laryngeal mask was removed 10min later and the nasal tube was replaced. The patient evolved satisfactorily and was discharged from the NICU the next day after surgery.
Prior to 1988, when Dr. Brain introduced the laryngeal mask (LM), the only two airway management options were the facemask and tracheal intubation (the recommendation for preterm babies is the tracheal tube no. 2.5).1 Thousands of articles and chapters published have ascertained the usefulness of the laryngeal mask as an extra-glottic device.2 A broad range of devices modified from the original design have been introduced in the last 20 years, with a view to allow for adequate ventilation and oxygenation, easy placement and minimum risk of pulmonary aspiration.
The term extra-glottic devices are currently used to refer to any airway management device that bypasses the larynx, including those with peri-glottic components.2
The classical size 1 laryngeal mask for neonates was implemented back in 1994 and 12 years later an improved version was introduced: the Proseal size 1 mask that provides better safety and improved sealing of the airway, and has a drainage channel.3,4 Currently, when the second-generation devices are not available, the classical mask is indicated (as shown in this case).
The laryngeal mask is available in sizes 1 and 1.5 for use in neonates and infants less than 5kg and from 5 to 10kg, respectively. In contrast to the facemask in neonates, it requires no head, neck or mandible manipulation, avoids the facial nerves compression, releases the operator's hands, yields better seal pressure and hence results in adequate positive pressure ventilation, in addition to adequate ventilation of patients with craniofacial malformations (Pierre–Robin and Treacher–Collins syndromes).5,6 In a meta-analysis of 52 prospective trials, the advantages of the laryngeal mask versus the facemask were: easy to place by unskilled personnel; better arterial oxygen saturation and enhanced surgical conditions during ear surgery in children.7
When compared to tracheal intubation, the laryngeal mask allows for easier and successful placement by anesthesiologist and unskilled personnel; less respiratory tract invasion; lower hemodynamic stress during placement and removal8, which theoretically would reduce the incidence of intracerebral hemorrhage in neonates and premature babies. There are reports of safe use in patients with malformations compromising the upper airway and hindering facialmask ventilation and laryngoscopy; in addition to causing a lower increase of intraocular pressure and avoiding the use of muscle relaxants.6,7
Some of the key disadvantages associated with the use of the laryngeal mask in neonates include gastric insufflation, the risk of aspiration and inadequate alveolar ventilation since the new born babies require higher airway pressures to achieve adequate tidal volumes. These issues may be probably solved with the availability of the Proseal® laryngeal mask in 1 and 1.5 sizes.9–12 Another disadvantage is the inability to suction the airway or to administer endotracheal medications.6
So, according to these characteristics, the laryngeal mask has three probable scenarios to be used in neonates: surgery anesthesia, resuscitation and intensive care.
Use in anesthesia: Baker et al. report a case of a neonate with non-syndromic disgnatia who was managed with laryngeal mask during an intra-partum ex utero therapeutic procedure (EXIT).13
It has been successfully used in patients with associated syndromes, with craniofacial disorders (Pierre–Robin and Treacher–Collins), for both, emergency management due to airway obstruction, and during anesthesia,14–16 even facilitating the passage of the firbobronchoscope through the laryngeal mask.17 In short lasting procedures,18 the Proseal® mask has been used in elective heart surgery, allowing for a better quality airway approach and much higher peak pressures and tidal volumes when contrasted against the classical laryngeal mask.19 Not only have these devices shown ease of use (100% success rate after two attempts), but also safety in terms of regurgitation, pulmonary aspiration, stridor and dysphagia.20,21
Use for resuscitation: A systematic review of neonatal resuscitation with facemask versus laryngeal mask in 2005 was unable to identify any controlled trials comparing both interventions.22 Only one trial was found comparing the use of the laryngeal mask versus a tracheal tube, with no significant differences. A prospective, quasi-randomized trial compared neonatal resuscitation with laryngeal mask versus facemask. 369 neonates requiring positive pressure ventilation were included; the rate of successful resuscitation was significantly higher (p<0.001) in the laryngeal mask group. In the severely compromised group of neonates with one minute Apgar score of 2-3, the laryngeal mask allowed for adequate resuscitation in 7 of 9 patients, while in the facemask group all required tracheal intubation. The first attempt of successful introduction of the LM was 98%.
The current recommendation of the 2010 resuscitation guidelines (AHA-European council)23,24 is to indicate the laryngeal mask for neonatal resuscitation as a valid alternative when facemask ventilation has not been effective and when the intubation attempts have failed or are not feasible. The LM allows for positive ventilation in neonates over 2000g or over 34 weeks of age. There is no evidence in younger patients to make a recommendation. There are no studies to indicate its use in the case of meconium aspiration, during chest compression or for the administration of intra-tracheal medication.
Intensive care use: Trevisanuto et al. reported a trial in 8 31-week old preterm babies, with an average weight of 1700g, who received surfactant through a laryngeal mask.25 After 3h of the administration the blood pressure and the alveolar oxygen concentration increased with no complications.
A systematic review in 2011 found just one study in 26 preterm babies with respiratory distress syndrome comparing the administration of surfactant through the LM versus no treatment and found that the fraction of inspired oxygen required for adequate arterial saturation was lower in the treated group. No differences were found in terms of the number of days in mechanical ventilation or pneumothorax-like complications.25
ConclusionThe laryngeal mask is a device that allows for adequate ventilation in neonates during anesthesia and is a valid option in patients with airway dysfunction, whether due to craniofacial malformations or to laryngeal and subglottic disorders like the patient described in this case. Second generation devices provide an enhanced airway seal and GI tract suction (Proseal® or Supreme®). These are considered alternate devices during neonatal resuscitation in patients over 2000g that cannot be properly managed with a facemask or intubated. Some studies recommend their use for administering surfactant to preterm neonates with respiratory distress syndrome.26,27
FundingAuthors own resources
Conflicts of interestThe authors declare not to have any conflicts of interest.
Please cite this article as: Páez L JJ, Navarro V JR. Uso de máscara laríngea en un lactante con estenosis subglótica. Reporte de caso y revisión de la literatura. Rev Colomb Anestesiol. 2013;41:150–4.