Total intravenous anesthesia is a widely used technique that relies on the use of intravenous anesthetics, propofol being the most frequently used and studied. At present, there are pharmaceutical and pharmacokinetic tools that are used to generate mathematical models to ensure the safe and moderately effective use of this technique. However, the depth of anesthesia is determined purely on the clinical findings and this requires neurological monitoring such as the bi-spectral index (BIS) in order to correlate the data derived from the pharmacokinetic models used for the administration of the anesthetic with the determination of its desired clinical effect.
We designed an operating system for automated control of the propofol infusion that provides feedback on the basis of the data generated by the BIS monitor. The system is programmed to increase or decrease the propofol infusion within a specific BIS range and, consequently, in accordance with the needs of the individual patient.
We describe anesthetic management using this technique in a female patient taken to surgery for prosthetic mammary implantation under general anesthesia at the University Hospital. An intraoperative record was generated including the depth of anesthesia and its action on propofol concentration at the effective site using the automated administration and control system.
We concluded that the use of closed-loop total intravenous anesthesia under neurologic monitoring is the next step in the evolution of this technique. It is less reliant on the pharmacokinetic models available at present, and is better suited to adapt to the specific needs of individual patients and to the type of surgical intervention.
La anestesia total intravenosa es una técnica ampliamente utilizada que tiene como base el uso de anestésicos intravenosos para su realización, siendo el propofol el más usado y estudiado para tal fin. Actualmente se dispone de herramientas farmacéuticas y farmaco-cinéticas que generan modelos matemáticos para el uso de esta técnica de manera segura y moderadamente eficaz. Sin embargo, la profundidad del estado anestésico es una medida netamente clínica que requiere el uso de monitorización neurológica tipo índice biespectral, el cual permite correlacionar los datos generados por los modelos farmacocinéticos empleados para la administración del anestésico y su efecto clínico deseado. Para tal efecto diseñamos un sistema operativo que retroalimenta y controla de manera automática la infusión de propofol tomando como base los datos generados por un monitor de índice biespectral, sistema que se programa para aumentar y disminuir la infusión de propofol de acuerdo a un rango específico de valor del índice biespectral, y por ende las necesidades especificas de cada paciente. Describimos el manejo anestésico con esta técnica en una paciente sometida a implante de prótesis mamaria bajo anestesia general en la IPS Universitaria en la cual se logro generar un récord intraoperatorio de la profundidad anestésica y su consecuente acción sobre la concentración de propofol en sitio efectivo usando este sistema de administración y control automático. Concluimos que el uso de la anestésica total intravenosa de lazo cerrado con monitorización neurológica es el siguiente paso en la evolución de esta técnica, la cual ofrece menor dependencia a los modelos farmacocinéticas usados en la actualidad y mayor capacidad de adaptación a las necesidades particulares de cada paciente y tipo de intervención quirúrgica.
Total intravenous anesthesia as a form of general anesthesia has gained more acceptance among anesthesiologists in recent decades as a result of the increasing availability of various pharmacokinetic models and software packages that make it safer and more reliable. Currently in the world, the trend is to optimize its use by means of monitoring tools that enable a more physiological approach to general anesthesia. With this in mind, we have developed a closed-loop total intravenous anesthesia system using the bi-spectral index (BIS) as an automatic control variable of blood concentrations of propofol in a target-controlled infusion (TCI) system. An older publication1 describes the implementation, with optimal results, of a software developed for open-loop propofol administration. However, we believe that these systems need to evolve to real time control, closer to the state of anesthesia. Along those lines, we present here the case of a patient undergoing a surgical operation under general anesthesia using a TCI system with propofol under closed-loop control.
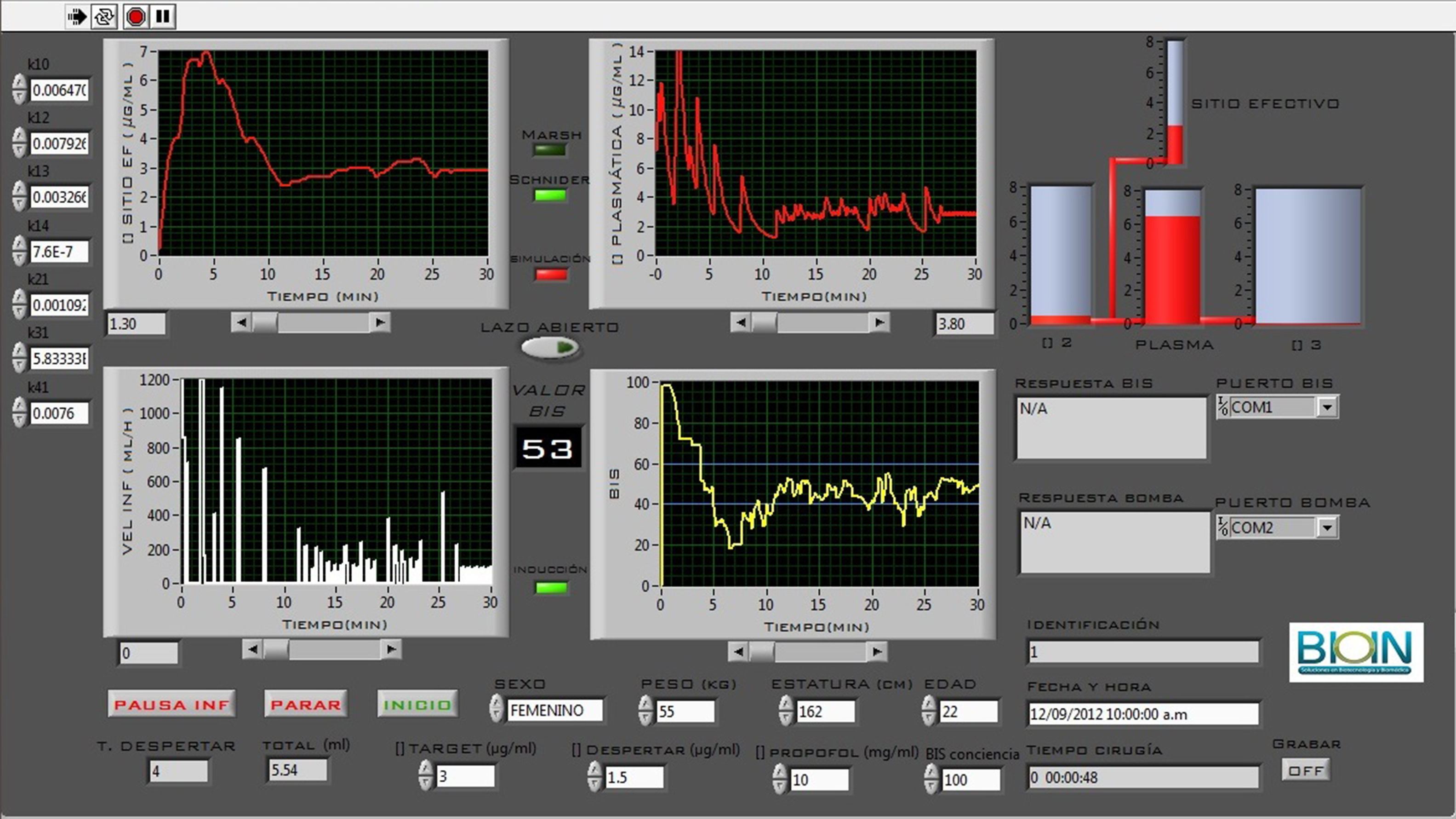
MethodsThe control system, designed on the Labview platform, contains the Marsh and Schnider pharmacokinetic models and the communication protocols needed to receive information from the BIS Vista monitor and to control the Graseby 3400 infusion pump. The system monitors the BIS signal every 5s and makes predictive decisions every time it checks; proportional and integrative decisions are made every 2min, depending on the difference between the desired BIS value, preset at 50, and the value of the acquired BIS signal. Hence, when the patient is in a deeper state of hypnosis, the system lowers the target concentration at the effective site, and when the patient is in a lighter state, the system increases the concentration. With the push of a button, the system allows to change the control type from open loop to closed loop and vice versa, which means that total consistency between the two control types is mandatory in order to provide high stability to the patient, even if the change from closed loop to open loop occurs several times during the same procedure. To achieve this, the software changes the set point of the system instead of doing a baseline analysis of each patient that creates the need to change control parameters. In other words, when the system is operating in the closed loop mode, it does not abandon the pharmacokinetic model adopted from the start of surgery, but rather changes the target concentration systematically at the effective side, always using the same model and the same pharmacokinetic constants.
This means that the target concentration goes through small adjustments every 5s, depending on the slope and the trend of the BIS signal, and larger adjustments every 2min, depending on the absolute difference and the area under the curve of the BISerror.(*) signal.
The system is in compliance with the regulations in place in the territory of Colombia for the clinical use of prototype medical and biomedical devices.2
Clinical caseThis was a case of a 22-year-old patient, ASA I, with no relevant personal, family or surgical history, scheduled for prosthetic breast implantation. The patient was asymptomatic and in adequate physical condition, with no predictors of a difficult airway, and in a state of cardiorespiratory stability. Pre-operative tests showed Hb at 13.2, platelets at 309,000 and normal coagulation times. The procedure was authorized, and the anesthetic risks were explained, including those of closed-loop TIVA with BIS. The patient understood and signed the informed consent.
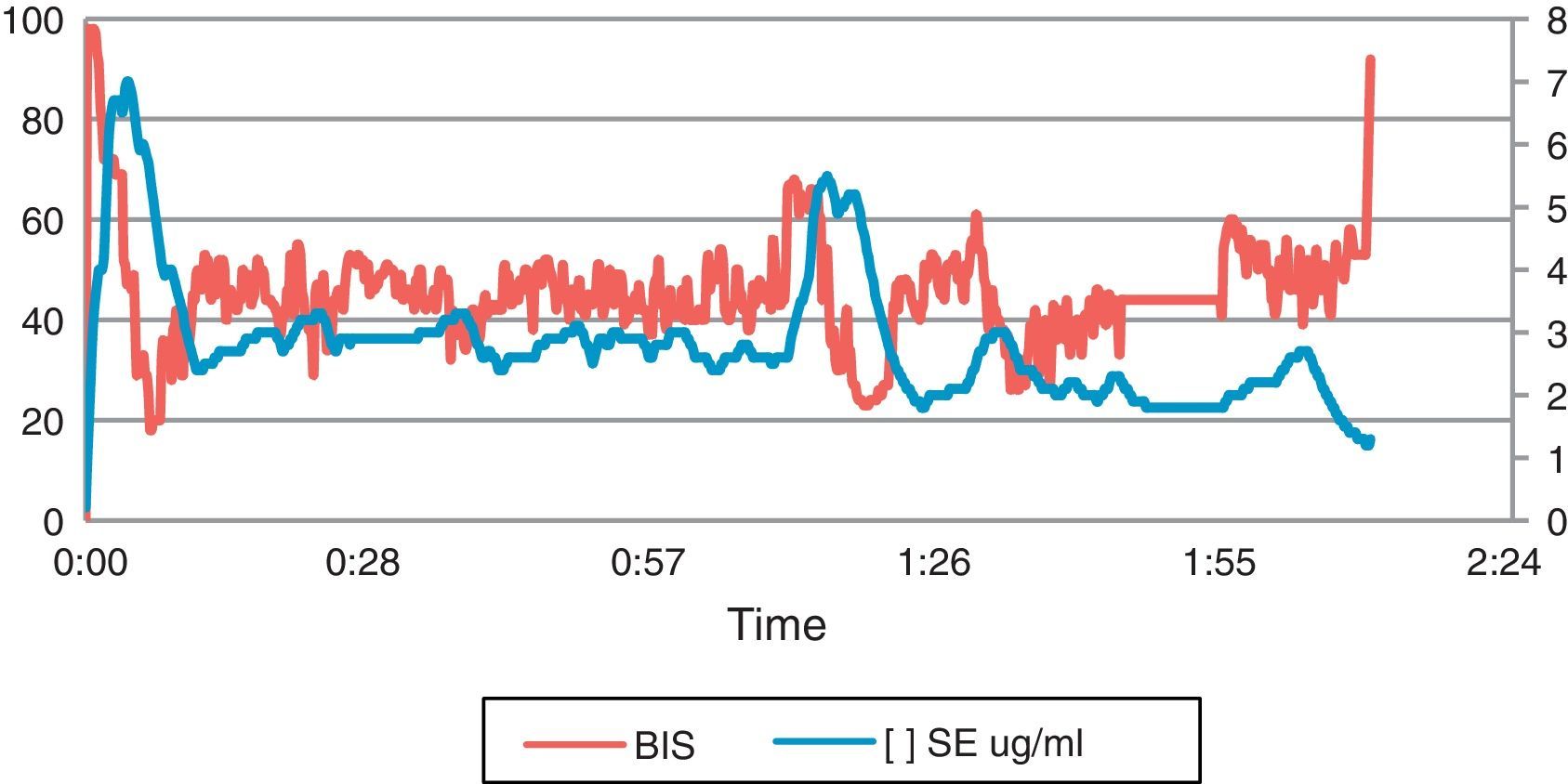
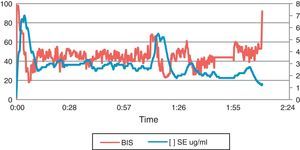
The patient was admitted to the operating room of the university hospital with no changes in the physical status. The patient was reminded about the anesthesia technique, and the basic ASA monitoring was instituted. The BISvista® monitor interface was adjusted with the closed-loop TCI system and the feedback process was initiated. Anesthesia induction was started with fentanyl 100μg, lidocaine 100mg, rocuronium 10mg, dexamethasone 4mg, and TCI propofol using the Schnider pharmacokinetic model with an effective site concentration of 6.5μg/ml until a BIS 50 was obtained. At that point, a number 3 laryngeal mask was introduced and a continuous infusion of remifentanil was started at 0.15μg/kg/min; closed-loop TCI propofol was added to maintain the BIS within the 40–60 range. The surgical procedure was initiated at that point. Below is the record obtained in the TCI system, representing the BIS reading versus effective site concentration, which the software adjusted throughout the entire procedure (Fig. 1).
The procedure lasted approximately 2h and there were no anesthetic or operative complications. Analgesia included morphine 5mg+Dipirone 2g+diclofenac 75mg IV, apart from bilateral intercostal blockade. The patient woke up when the BIS was at 88 and [] at the effective site was 1μg/ml. In the immediate post-operative period, the patient did not report nausea or vomiting or intra-operative recall, and pain on the VAS scale was 1/10.
Fig. 2 shows a screenshot of the software control panel, highlighting the central knob that is used to exit the closed loop so that the anesthesiologist may take control of the delivered dose.
DiscussionOur goal with this case was to assess the performance of a closed TCI system with BIS in a patient taken to ambulatory plastic surgery. The need for hypnotics varies from patient to patient and, more often still, between types of surgeries in the same class of patient. In traditional practice, given the lack of monitoring of the depth of anesthesia, most of the time the agents were underdosed or overdosed, depending on the context.3,4 The bi-spectral index monitor (BIS) is a passive EEG analyzer that allows for titration of hypnotics over a specific range of cortical activity,5 enabling real-time adjustments to the required dose according to the individual patient's anesthetic requirements. This results in lower anesthetic consumption, lower rates of intra-operative recall and more predictable recovery.4,6 Manual propofol infusion is based on linear pharmacokinetic models that predict blood and effective site concentrations, as well as washout.7 When the infusion is corrected in accordance with the BIS value (pharmacokinetic/pharmakodynamic correlation), the anesthesiologist estimates the dose needed to be infused to maintain a constant BIS level.7 In an open loop system, the intervention of the physician is required for adjusting the dose on the basis of the clinical response to the set dose.8 The main issue with this method is the difficulty in adjusting the accurate dose throughout the process, considering that it is difficult to make adjustments every 5 or 10min.
Graph 1 shows the rapid response of the system at around minute 67 when, due to a strong pain stimulus, the BIS signal rose above 60, even though the concentration at the effective site remained stable. The concentration was increased by the system almost immediately triggering a controlled propofol bolus. This resulted in a lowering of the BIS signal down to an adequate range in less than 3min.
The implementation of new technologies has resulted in a trend toward developing closed-loop automatically controlled intravenous anesthesia.9 At present, automated delivery systems are based on feedback from different clinical signals, reducing the risk of inadequate control which is clearly evidenced in the usual clinical practice based on open loop systems.10 In this regard, closed loop systems have the theoretical advantage of improving the quality of anesthesia because of the high level of vigilance maintained throughout the procedure.11 Multiple closed loop systems have been designed worldwide based on different control variables: Auditory Evoked Potentials (AEPs), EEG-derived indices such as BIS or M-Entropy.12,14,15 However, there are very few papers to date in the literature regarding its application with real patients in clinical practice. Our system initially integrates the BIS control variable to determine the levels of hypnotics required for maintaining the desired anesthesia state. Although it is true that a more objective representation of the depth anesthesia like AEPs may be more reliable when it comes to implementing this type of system, most closed-loop systems reported in the literature are based on the BIS signal, making it a general standard for monitoring anesthetic unconsciousness.13–21
The effect of the co-administration of remifentanil and propofol on the BIS during general anesthesia has been a controversial issue. It is believed that opioids have a variable effect on the EEG because of their action on non-cortical structures.21 An additive interaction has been reported with propofol but, within a clinical range (usually <8ng/ml), remifentanil has little effect on the BIS.13,14,22,23 In this report, a low-to-moderate dose of remifentanil was used in order to maintain a basal level of analgesia based on a pharmaceutical model. However, it has been widely demonstrated that, ideally, remifentanil administration must be based on pharmacokinetic models,24 which was not the case in this patient because of exceptional operational reasons. However, it is our wish to design and assess a dual control system – propofol and remifentanil – maintaining control over pharmacokinetic as well as pharmacodynamic variables with the help of the BIS.
Another limitation of automated BIS-driven anesthetic administration is precisely hypnotic adjustment based only on a single variable, which might eventually override the physician's clinical judgment. Although BIS is a reliable measurement, it is not a perfect parameter. In any case, the closed-loop system that we propose with this case has been shown to be safe as long as it is under direct control of the attending anesthesiologist. It is the anesthesiologist who determines the relevant adjustments to the system, taking into consideration the rest of the clinical variables in order to adapt it to the patient's situation. Consequently, the closed-loop system is not intended to replace the anesthesiologist but rather to improve his/her performance and efficiency.
ConclusionWe were able to develop and evaluate an anesthesia delivery system which does not depend on the various pharmacokinetic models currently available, but rather adapts the pharmacokinetic models to the context and needs of each individual patient. We expect to conduct a study to assess the operational conditions in a larger population, comparing this system with an open loop system which we designed previously, and then go on to determine the performance of a propofol/fentanyl closed-loop setup.
FundingThe author's own resources.
Conflict of interestNone of the authors claim conflicts of interest.
Please cite this article as: Gómez Oquendo FJ, et al. Anestesia total intravenosa en un sistema de lazo cerrado: reporte del primer caso en Colombia. Rev Colomb Anestesiol. 2013;41:306–310.