Throughout the years, several methods have been developed to help determine injury severity and obtain accurate prognoses in trauma patients. Trauma scores that have been used for more than 40 years are extremely useful in clinical practice as well as in research.
ObjectiveTo conduct a review of the most relevant literature on trauma and to make a description of each of the scoring tools, focusing on their limitations and their application in clinical trials.
Materials and methodsNarrative review conducted in different databases such as PubMed, ScienceDirect and OVID. A manual search was also conducted of articles on the subject in both English and Spanish.
ResultsThe review articles provided an adequate description of each of the scores, the way they are calculated, the main limitations in their application, and the most relevant findings in the literature.
ConclusionThere is a wide range of severity scores used in trauma patients for anticipating clinically significant outcomes with varying degrees of accuracy. Creating and validating a single, universally valid score is a huge challenge; consequently, the selection of the scoring tool is based, to a large extent, on experience, the context and the available evidence.
a lo largo de la historia se han creado varios métodos para evaluar la gravedad de las lesiones y brindar un pronóstico exacto en pacientes con trauma. Los puntajes en trauma que se han utilizado por más de 40 años son una herramienta de gran utilidad tanto para el contexto clínico como investigativo.
Objetivoelaborar una revisión de la literatura más relevante sobre los puntajes en trauma y hacer una descripción de cada una de estas herramientas, haciendo énfasis en sus limitaciones y en la aplicación en estudios clínicos.
Materiales y Métodosrevisión narrativa, se consultaron diferentes bases de datos como PubMed, ScienceDirect y OVID; además, se hizo búsqueda manual de artículos en inglés y en español sobre el tema.
Resultadoslos artículos revisados permitieron hacer una descripción adecuada de cada uno de los puntajes, de la forma en que se calculan, sus principales limitaciones al momento de aplicarlos y los hallazgos más notables en la literatura.
Conclusiónexiste una gran variedad de puntajes de gravedad para pacientes con trauma que permiten anticipar con diferente exactitud los desenlaces clínicamente significativos. La creación y validación de un único puntaje universalmente válido es todo un reto; por ello la selección de esta herramienta está basada en gran parte en la experiencia, el contexto y la evidencia disponible.
In trauma, scores are used to obtain a numerical description of the severity of an individual's injuries and clinical condition, which in turn is associated with prognosis.1,2 Scores have been used for more than 40 years since the initial Injury Severity Score (ISS) was proposed3 and they are still used for different purposes: as a common language for the healthcare community, as a means to compare mortality rates based on severity, as a basis for clinical decision-making, and for research, among others.1
Mortality becomes the indicator used to evaluate the accuracy of trauma scores, taking into consideration two characteristics:
Discrimination: the ability of the score to make a distinction between survivors and non-survivors, usually determined on the basis of the area under the curve of the receiving operating characteristics (AUC-ROC).
Calibration: the ability of the score to predict mortality and the concordance between prediction and actual observation. It is usually measured with the Hosmer–Lemeshow (HL) test for goodness of fit.1,4
The purpose of this review is to make a detailed description of the scores in order to help with their knowledge and understanding, based on the most important findings in the literature.
Narrative review of the medical literature on trauma. A search was conducted in several databases including PubMed, ScienceDirect and OVID; an additional manual search of articles on the subject in English and Spanish was also conducted. The final sources reviewed included 48 articles related to the assessment of trauma patients, published since 1974; of these, 9 were prospective and the rest were databases of trauma registries. All the original articles had been published in English and dealt with emergency or pre-hospital care cases.
ResultsDepending on the variables assessed, scores may be classified into anatomical, physiological and combined. Results are presented in chronological order and four aspects are developed for each score: general description, calculation, limitations, and relevant findings in the literature.
Anatomical scoresAIS (Abbreviated Injury Scale)General description: Developed by the U.S Association for the Advancement of Automotive Medicine (AAAM), this score is used as a basis for other scores, including the ISS.3 This tool has been updated 7 times since its introduction in 1971, the most recent being the 2008 update.2
Calculation: This score includes more than 2000 diagnoses in which each injury is assigned a number from 1 to 6, where 1 is a minor injury, 5 is a critical injury and 6 is an intractable, fatal injury.5
Limitations: There are performance drawbacks in penetrating injuries, hypothermia, burns, electric injuries and smoke inhalation.6 Being just a scoring system, it cannot be used to predict outcomes, and concomitant use of other tools is needed for that purpose.
Findings in the literature: In a recent comparison with the International Classification of Diseases, 9th Revision (ICD-9), prediction based on the AIS was found to be superior.7,8
ISS (Injury Severity Score)General description: This score is used for the classification of multiple-trauma patients. Each injury is given up to 6 points and the score describes six regions of the body3:
External: including all skin injuries such as lacerations, abrasions or burns.
Limbs: including pelvis.
Abdomen: including all internal organs and the lumbar spine.
Chest: including internal organs, diaphragm, rib cage and thoracic spine.
Face: sensory organs and bony structures.
Head and neck: including brain or cervical spine injuries.6
Calculation: The calculation is made using the same codes assigned to each of the 2000 diagnoses included in the AIS, grouped according to the 6 regions of the body. The highest AIS points are taken into consideration, one for every region of the body. These are then squared and then the scores for the three most affected different anatomic regions are added. The sum total is the ISS score, which ranges from 1 to 75. This latter score can be reached only with an AIS score of 5 in three different regions of the body. When an injury is given a score of 6 in the AIS, a score of 75 is assigned automatically in the ISS without considering other areas.3
Limitations: Because it considers only 3 different regions of the body with the highest score and only measures one injury per region, its most important limitation is in penetrating trauma. Consequently, severe injuries with a high score are masked because they are in the same area of the body, given that involvement of other organs is not considered.
Findings in the literature: A cohort study analyzed 2292 patients to explore differences in several ISS and AIS score ranges according to the mechanism of injury.9 A significant difference in mortality was found between patients with blunt trauma and patients with penetrating trauma with an ISS score between 25 and 40 (23.6 vs. 36.1%, respectively, p=0.022). Within this range in the ISS, mortality was higher among patients with penetrating head injuries (75% vs. 37% in blunt trauma).9,10
NISS (New Injury Severity Score)General description: In response to the limitation described for the ISS, in 1997 Osler et al. introduced the NISS,11 proposed as the new gold standard for trauma severity scores.
Calculation: The score is calculated the same way as the ISS (sum square of the three most severe injuries), but without discriminating by body region.12
Limitations: No differences in performance have been found between the ISS and NISS in patients with penetrating trauma, and the NISS could overestimate severity by assigning higher severity to an injury in the same body region than to an injury that is not as severe in another region.13,14
Findings in the literature: A study conducted in Canada in 15,200 patients with blunt trauma compared patients with the worst two lesions in different regions of the body (DR, different region) with patients with the two worst injuries in the same region (SR, Same region), excluding external injuries. It found that patients with DR injuries had a higher risk of dying than those with SR injuries SR (OR=1.69; 95% CI=1.30–2.21).15 A retrospective study with 770 patients evaluated the use of ISS, NISS, APACHE II and prothrombin time (PT) for diagnosis and found that PT and APACHE II provided higher discrimination both in patients that died on the first day as well as in those who died three days after admission (AUC=0.89 and 0.88, respectively), as compared to ISS and NISS (AUC=0.67 and 0.70, respectively).16
TMPM (Trauma Mortality Prediction Model)General description: This model may be applied to the AIS classification, as well as to the ICD-9.17 A regression coefficient is required in order to enter injuries in this model, enabling severity comparisons of individual injuries.
Calculation: The TMPM-AIS assigns a severity value to each of the AIS codes and estimates the probability of death on the basis of the five most severe injuries, by means of logistic regression. Mortality can also be predicted using the TMPM-ICD-9, the difference being the use of the ICD-9, which is the most widely used system in the administrative area8 and is more widely available in our setting.
Limitations: The need for a regression model may make it more difficult to apply. Although several studies have shown superiority of the TMPM, evidence is scant and additional research is required for validation and widespread application.
Findings in the literature: A study based on the National Trauma Data Bank (NTDB), conducted between 2001 and 2005 with 702,729 patients found that the TMPM-AIS offered better discrimination (AUC=0.901) and calibration (HL=58, 35–91) than the ISS (AUC=0.871 and HL: 296, 228–357, respectively).17 Another retrospective analysis of the NTDB conducted between 2007 and 2008 compared the TMPM-ICD-9 with the NISS and the ISS in 533,898 patients and found that the TMPM offers better discrimination than the previous models (AUC=0.866 vs. AUC=0.835 and 0.832, respectively).8 Using the same database, a more recent study designed to compare discrimination, calibration and predictive capacity of five scoring systems used in trauma (ISS, NISS, ICD-9-Based Injury Severity Score [ICISS], AIS and TMPM), found TMPM to be superior for mortality prediction, compared to other scores and in a calibration curve close to 45°, indicating excellent match between observed mortality and TMPM-predicted mortality.18
Physiologic scoresGlasgow Coma Scale (GCS)General description: The Glasgow Coma Scale was developed in 1974 in Glasgow University, Scotland.19 It was the first scoring system proposed for quantifying severity of head injury (HI), and allows measurement of the level of consciousness.19
Calculation: It evaluates spontaneous ocular opening, ocular opening in response to a verbal command, or to a painful stimulus, or absence of response. Verbal response classifies the patient as “oriented” when oriented in terms of time, place and person; “confused” when the patient can verbalize phrases or words but is not oriented; “inappropriate words” if only monosyllables or exclamatory speech are used; or “incomprehensible sounds” if no verbal response is obtained but some form of sound is perceived; and “none” if there is no verbal response.20,21 Motor response is assessed initially if there is response to a verbal command. If not, it is assessed using a painful stimulus to determine if the patient localizes the pain, withdraws the part of the body receiving the stimulus, shows abnormal body flexion or extension, or if response is absent.22 The number on the GCS is used to define head injury as mild,13–15 moderate9–12 or severe (less than 8).23–25
Limitations: Although it is a very useful tool, accuracy is lost in patients who are intubated, sedated or with orbital trauma26 and in patients with primary abnormalities of the sensory organs. Prediction of other clinically significant outcomes like ICU length of stay or survival is highly variable.27
Findings in the literature: Motor response is the most important of the three variables because of its significance as a prognostic factor.28 In a study conducted using the American College of Surgeons database in order to assess the predictive ability of the GCS, it was determined that motor response contributes the greatest proportion of the discrimination power (AUC-ROC 0.87), compared to other variables; even when it is the only variable available, it provides a reliable assessment of the patient's condition.29–31
Revised Trauma Score (RTS)/TS (Trauma Score)General description: The TS severity score assesses circulatory system function using systolic arterial pressure (SAP) and capillary filling; of the respiratory system using heart rate (HR) and respiratory expansion; and of the central nervous system (CNS) using the GCS. However, capillary filling and respiratory expansion are difficult parameters to assess, and it has been found that when these were used, the TS underestimated the severity of HI.32 In view of the above, in their review in 1989, Champion et al. decided to exclude these parameters, resulting in an improvement of score accuracy and the development of two new versions: one for triage (T-RTS) and a second one for assessing outcome and monitoring injury severity (RTS).33
Calculation:
T-RTS: It is calculated by adding SAP, HR and the HI score, and it may vary between 0 and 12.
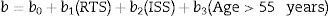
RTS: It is the sum of the values listed above but modified by constants derived from a logistic regression model for mortality. The result ranges between 0 and 7.84, using the following formula29:
The RTS assigns a score for certain GCS, SAP and HR values and is widely used in trauma research as quality control and point of reference. It is part of the Trauma and Injury Severity Score (TRISS) and A Severity Characterization of Trauma (ASCOT).34
Limitations: The sensitivity of the triage version is low (54%) with a result lower than 11, but specificity is acceptable (84%), justifying its use together with other sources of data.30,32
Findings in the literature: A study conducted in 347 patients over 65 years of age to determine the accuracy of ISS and RTS in predicting mortality and length of stay found that these two scores predicted mortality adequately but did not correlate with hospital length of stay.35
Combined scoresTRISS (Trauma and Injury Severity Score)General description: It was developed when Champion et al. observed that the anatomical description of injuries using the ISS needed the additional information of the patient's physiologic response. It was developed based on the data from the Major Trauma Outcome Study36,37 and is an estimate of the probability of survival, with a result between 0 and 1.38
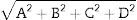
Calculation: Probability of survival (Ps) is calculated using the following formula34:
where “e” is equal to 2.718 and b is calculated in accordance with the trauma classification as closed or penetrating, using the following formula34:Values for the b coefficients are available in the referenced literature.38–41
Limitations: Mortality is the single predicted outcome, the process of gathering the information is complex, coefficients (bx) should be updated constantly, and considering that it is based on the ISS and RTS, it shares the limitations of these two models.30,42 Ps is simply a mathematical outcome and not absolute estimated mortality, meaning that it may fail in one out of every five patients.43,44
Findings in the literature: The British trauma registry, the Trauma Audit and Research Network (TARN), developed its own model for predicting mortality in trauma patients based on the TRISS. The new model was developed on the basis of 100,399 trauma admissions in various hospitals between 1996 and 2001 and includes the following predictors: age, modified ISS, GCS, sex, and sex-age interaction. The original study showed an AUC of 0.947 (95% CI=0.943–0.951).4,45
ASCOT (A Severity Characterization of Trauma)General description: This score uses the physiological parameters of the RTS, age, and the anatomical profile.30,46 It has been useful for penetrating as well as for blunt trauma, for predicting disability, hospital length of stay and use of resources.
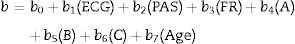
Calculation: RTS and the A, B and C items of the anatomical profile are calculated. The anatomical profile considers severe injuries (AIS ≥3) of the head, brain and spinal cord (A), chest and anterior part of the neck (B) and severe injuries of other regions of the body (C). Mild or moderate injuries (AIS ≤2) are grouped under letter D. Overall, it consists of 4 variables used in the following formula27:
The calculation is similar to the one used for the TRISS (Ps=1/(1+e−b)),where
Values for b coefficients are available in the referenced literature.
Limitations: Compared to the TRISS, it has a slightly higher predictive value, but its calculation is far more complicated.47
Findings in the literature: Champion et al. compared the TRISS and the ASCOT for predictive ability in 14,296 patients and found that the sensitivity of the ASCOT was higher than that of the TRISS (69.3 vs. 64.3), while the AUC-ROC for both scores was found to be >0.90 both for blunt as well as for penetrating trauma.48 Although the calibration and discrimination tests are satisfactory, sensitivity of the two scores is not good.49
RISC (Revised Injury Severity Classification)General description: Developed by the German Society of Trauma, this score includes laboratory parameters such as base deficit, haemoglobin and partial thromboplastin time, and interventions like cardiopulmonary resuscitation (CPR), improving discrimination and calibration when compared with the previous models.36
Calculation: Logistic equation that calculates probability of survival (Ps) using the coefficients for 11 variables: age, NISS, AIS-head, AIS-extremities, GCS, TTP, base excess, cardiac arrest with resuscitation or defibrillation, SAP <90mm Hg, haemoglobin <9mg/dl, and transfusion of more than 9 units of packed red blood cells. The coefficients and the formula are available in the referenced literature.50
Limitations: Complete information, required for this score, is only available from 25% of patients. It was developed from data collected between 1993 and 2000, creating the possibility of overestimating the risk of death if compared with the information from recent years.36
Findings in the literature: Researchers from Witten University in Germany updated the model to the Revised Injury Severity Classification version II (RISC II), including important revisions to age, the mechanism of trauma and comorbidities. The GCS was replaced with motor function assessment, and pupillary reactivity and size were included. In the RISC score, patients with missing data were excluded or normal values were assumed. In contrast, in the RISC II score, missing values are classified in a different category which is assigned a coefficient of zero and does not affect patient prognosis.23
ConclusionThere is currently a wide variety of scores – anatomical, physiological or combined – for the assessment of trauma patients, each with their own advantages and disadvantages. Anatomical scores require more time to complete because of injury assessment and classification and, consequently, they are seldom used during the event. Moreover, variability among evaluators is high. The challenge with physiological scores is to make predictions based on trauma patient physiology, which may vary considerably even in a matter of hours, rendering them inaccurate, and resulting in delayed patient care. Combined scores are the most comprehensive and, therefore, their application is more complex. It is difficult to select the most adequate score and there is a need to take into consideration factors like missing patient information, suitability in terms of outcomes, reproducibility, and variability after trauma, among others. The selection decision is based on practice, evidence and context, because prediction and classification of the individual subject is a process that requires more input than just score. For fast results, as required in the emergency setting, for example, GCS and RTS are suitable. In contrast, TRISS or NISS may be better when it comes to determining prognosis in the hospital. It is difficult to achieve the ideal score, but it is important to be aware of the available scores in order to improve treatment for trauma patients. Present and future research will help determine the true applicability and usefulness of trauma scores, as well as their ability to support decision-making in the individual patient.
FundingPartial funding from CODI (Committee for Research Development), Antioquia University, through the Biomedical and Health Science research project, 2012–2013 (Minutes 656-2013), and Antioquia University sustainability strategy – GRAEPIC 2014–2015.
Conflicts of interestThe authors have no conflicts of interest.
Please cite this article as: Restrepo-Álvarez CA, Valderrama-Molina CO, Giraldo-Ramírez N, Constain-Franco A, Puerta A, León AL, et al. Puntajes de gravedad en trauma. Rev Colomb Anestesiol. 2016;44:317–323.