To determine the prevalence of chronic kidney disease mineral bone disorder (CKD-MBD) and its association with morbidity and mortality among hemodialysis patients.
DesignObservational study.
Patients100 patients on maintenance hemodialysis were studied over 12 months at the Lilavati Hospital and Research Centre, Mumbai, India.
ResultsSerum calcium and serum phosphorus levels were monitored as per the recommended guidelines in only 8% of patients. Serum parathyroid hormone (PTH) levels were monitored in only 21% of patients. Majority of patients had high PTH values (>300pg/ml). Patients with low PTH (<150pg/ml) had a higher mortality and morbidity as compared to those with normal and high PTH.
ConclusionThis study shows that calcium/phosphorus/PTH monitoring is not done as per recommendations even in a tertiary care centre in India. The small magnitude of the associations observed in this study should serve to highlight the need to pursue other means of improving bone health among hemodialysis patients.
Determinar la prevalencia de las alteraciones del metabolismo óseo en la enfermedad renal crónica (CKD-MBD) y su asociación con la morbilidad y la mortalidad entre pacientes sometidos a hemodiálisis.
DiseñoEstudio observacional.
PacientesEn el Lilavati Hospital and Research Centre, Mumbai, la India, durante 12 meses, se estudió a 100 pacientes sometidos a hemodiálisis de mantenimiento.
ResultadosTan sólo en el 8% de pacientes se supervisaron los valores séricos de calcio y fósforo según las guías recomendadas. Los de parathormona (PTH) sólo se supervisaron en el 21% de pacientes y en la mayoría se detectaron valores altos (>300pg/ml). En pacientes con valores bajos (<150pg/ml) se evidenció una mayor mortalidad y morbilidad, comparado con aquéllos con valores normales y altos de la hormona.
ConclusiónEl presente estudio revela que, en la India, ni siquiera en un centro de asistencia terciaria se implementa la supervisión de los valores séricos de calcio/fósforo/PTH según lo recomendado por las guías. La pequeña magnitud de las asociaciones observadas en el presente estudio debería servir para destacar la necesidad de aplicar otros medios de mejorar la salud ósea entre pacientes sometidos a hemodiálisis.
Chronic kidney disease-mineral and bone disorder (CKD-MBD) is a systemic syndrome involving abnormalities in serum phosphorus, calcium and parathyroid hormone (PTH) concentrations, together with abnormalities in vitamin D metabolism and bone turnover.1 Abnormalities in serum phosphorus, calcium and PTH levels, common among patients with chronic kidney disease, have been associated with increased cardiovascular calcification,2–4 arterial dysfunction,5,6 morbidity and mortality.7,8
Recent studies have shown thatlevels of serum phosphorus, calcium and PTH outside clinical guidelines9–13 are associated with increased mortality and cause-specific hospitalization among hemodialysis patients. Our study presents the levels of CKD-MBD markers as well as their associations with clinical and mortality outcomes in patients undergoing maintenance hemodialysis (MHD).
AimTo evaluate chronic hemodialysis population in a tertiary care hospital based dialysis unit for:
- (1)
Frequency of biochemical assessment of MBD on MHD.
- (2)
What is the pattern of renal bone disease in our hemodialysis population?
- (3)
Outcome with respect to complications and survival.
- (4)
Are we following recommended guidelines, and achieving recommended goals?
- •
This is an observational study conducted at the Lilavati Hospital and Research Centre, Mumbai, India from 1/1/2009 to 31/12/2009.
- •
100 patients undergoing maintenance hemodialysis were observed over 12 months.
- •
Frequency of assessment of serum calcium, phosphorous, PTH and vitamin D were noted, including baseline values if available.
- •
Prescription patterns were analyzed, to note down if any changes were made after reports.
- •
All events on dialysis and at home were noted.
- •
The mean and standard deviation are reported for continuous variables and number and percentage are reported for categorical variables.
- •
Chi-square test was used to compare 2 variables and p value of <0.05 was significant.
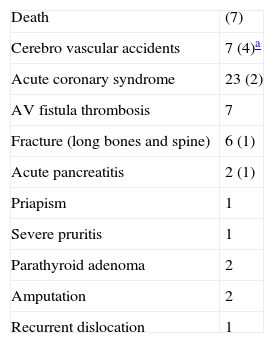
Hundred patients who are on maintenance hemodialysis (MHD) were included in this study. Mean age of the patients studied are 53.9±13 years. Mean duration on MHD is 16 months (Table 1). Majority of patients (71%) are undergoing thrice a week MHD (Fig. 1). Only 21 patients out of 100 got their serum parathyroid hormone (PTH) levels checked every 3–6 months, in last one year period and 7 out of 100 patients got their vitamin D3 levels (Fig. 2) and their values are shown in Table 2. At baseline, before entry into our HD program, 25% patients did not have serum calcium and phosphorus estimation in last 3 months and baseline PTH and vitamin D3 levels were not done in >90% of patients. Serum calcium and phosphorus levels were monitored every 1–3 months in 8% of patients only, where as most patients (74%) did it once in >3 months in spite of advise to do it monthly. Mean values of serum calcium is 9.04±0.9mg/dl and serum phosphorus is 5.59±1.8mg/dl and 39% had elevated calcium-phosphorus product (Table 3). Majority of patients in whom serum PTH values were measured (10 out of 21) had higher PTH values (>300pg/ml) (Fig. 3). 52 adverse events including 7 deaths were noted during this one year period (Table 4). Patients with low PTH had a higher mortality and morbidity as compared to those with high PTH (Figs. 4–6).
Patient characteristics.
Adverse events in last one year.
| Death | (7) |
| Cerebro vascular accidents | 7 (4)a |
| Acute coronary syndrome | 23 (2) |
| AV fistula thrombosis | 7 |
| Fracture (long bones and spine) | 6 (1) |
| Acute pancreatitis | 2 (1) |
| Priapism | 1 |
| Severe pruritis | 1 |
| Parathyroid adenoma | 2 |
| Amputation | 2 |
| Recurrent dislocation | 1 |
KDIGO (Kidney Disease: Improving Global Outcomes) is an international initiative with a key mission of developing clinical practice guidelines in the area of chronic kidney disease (CKD). KDIGO recently published an evidence-based clinical practice guideline for the prevention, diagnosis, evaluation, and treatment of metabolic bone disease in individuals with CKD.14 KDIGO proposed a definition for CKD-mineral and bone disorder (CKD-MBD) and for renal osteodystrophy.15 The KDIGO guideline addresses the evaluation and treatment of abnormalities of CKD-MBD in adults and children with CKD stages 3–5 on long-term dialysis therapy or with a kidney transplant. Tests considered are those that relate to laboratory, bone, and cardiovascular abnormality detection and monitoring.
KDIGO recommend monitoring serum levels of calcium, phosphorus, PTH, and alkaline phosphatase activity beginning in CKD stage 3. Guidelines also suggest that it is reasonable to base the frequency of monitoring serum calcium, phosphorus, and PTH on the presence and magnitude of abnormalities, and the rate of progression of CKD. Reasonable monitoring intervals In CKD stage 5, including 5D would be: for serum calcium and phosphorus, every 1–3 months; and for PTH, every 3–6 months.14 They also suggest that in patients with CKD stage 5D, 25(OH)D (calcidiol) levels might be measured, and repeated testing determined by baseline values and therapeutic interventions. In our study only 8% of patients adhered to the KDIGO guidelines and got their serum calcium and phosphorus values checked every 1–3 months. Only 21% of patients got their serum PTH checked as per KDIGO and only 7% got their 25(OH)D levels checked during our study period. This could be attributed to high renal replacement therapy (RRT) costs in India. India has no governmental reimbursement for dialysis, and only a small percentage of patients with ESRD have employer sponsors or health insurance that pays for RRT.
In the Dialysis Outcomes and Practice Patterns Study (DOPPS) the distribution of PTH levels was wide and markedly skewed.16 Large differences in PTH distributions were observed across phases and countries, especially in Italy, the United Kingdom, and Australia and New Zealand. No significant trend was seen in mean PTH levels in the overall DOPPS population. Our study showed that majority of patients (10 out of 21) had increased PTH values.
Distributions of baseline serum calcium and phosphorus levels in DOPPS study was 9.3±0.9mg/dl and 5.5±1.8mg/dl, respectively.16 Mean values of serum calcium and phosphorus in our study was 9.04±1.1mg/dl and 5.59±0.7mg/dl.
DOPPS study showed that PTH levels of 100pg/mL or less were associated with significantly greater cardiovascular mortality only in time-dependent models.16 Significantly greater all cause mortality risk was observed for PTH levels greater than 600pg/mL (ng/L). In contrast to these findings as well as findings from previous studies, our study showed patients with low PTH had a higher mortality and morbidity as compared to those with high PTH. Our study showed that patients with low PTH had greater cardiovascular mortality, consistent with DOPPS study results.
This is an observational study; our findings can indicate associations, but not causal relationships, between mineral metabolism indicators and mortality. Bone biopsy was not done in our study population, we are defining the type of bone disease based on PTH levels. The study period was too less and we acknowledge that calcium, phosphorus, and PTH have not been validated as surrogate markers for such hard end points as mortality.
ConclusionGuidelines for CKD-MBD are clear about monitoring of bone health in dialysis patients, however even in a tertiary care centre, with majority patients taking thrice a week HD, calcium/phosphorus/PTH monitoring is not done as per recommendations.
It is possible that interventional studies will show a link between calcium, phosphorus, PTH and morbidity and mortality among hemodialysis patients and that appropriate treatment of these derangements according to current practice guidelines will result in improved bone health and quality of life.
Conflict of interestThe authors declare no conflict of interest.