Physical activity is one of the mainstays of treatment for type 1 diabetes mellitus (DM1). When done safely, it is beneficial for improving metabolic control and patient quality of life, and for reducing the chronic complications of diabetes.1 With the aim of establishing a consensus regarding safe sports activities in these patients, the Spanish Society of Endocrinology and Nutrition developed the RECORD guidelines, addressing assessment before, during and after exercise, as well as intervention in risk situations.2
A cross-sectional observational study was carried out, based on a specifically designed survey using vocabulary adapted to the age of the subjects, to assess the adherence of patients with DM1 to the sports activity recommendations of the RECORD guidelines2 (Table 1). The survey was targeted independently to both the patients (if over 8 years of age) and to their main caregivers. A joint interview was conducted when the results did not prove consistent. All patients with DM1 under 18 years of age and controlled in the Pediatric Endocrinology outpatient clinic of Hospital Universitario Río Hortega in Valladolid (Spain) were included in the study. At the start, the participants received diabetes education, including the sports activity measures recommended by the RECORD guidelines. All patients were duly informed about the study, and the corresponding consent form was signed by at least one of the parents or guardians, and by the patients in person if over 12 years of age. The study was approved by the Research Ethics Committee of Área Oeste (Valladolid, Spain). The Pearson chi-square test was used to analyze associations between the study variables. If the number of cells with expected values of <5 was greater than 20%, the corresponding likelihood ratio (LR) was calculated. The Student t-test for two independent samples was used for the comparison of mean values, while analysis of variance (ANOVA) was used when more groups were involved. The alternative nonparametric tests were the Mann-Whitney U-test (for two groups) or the Kruskal–Wallis H test (for more than two groups). Statistical significance was considered for p<0.05.
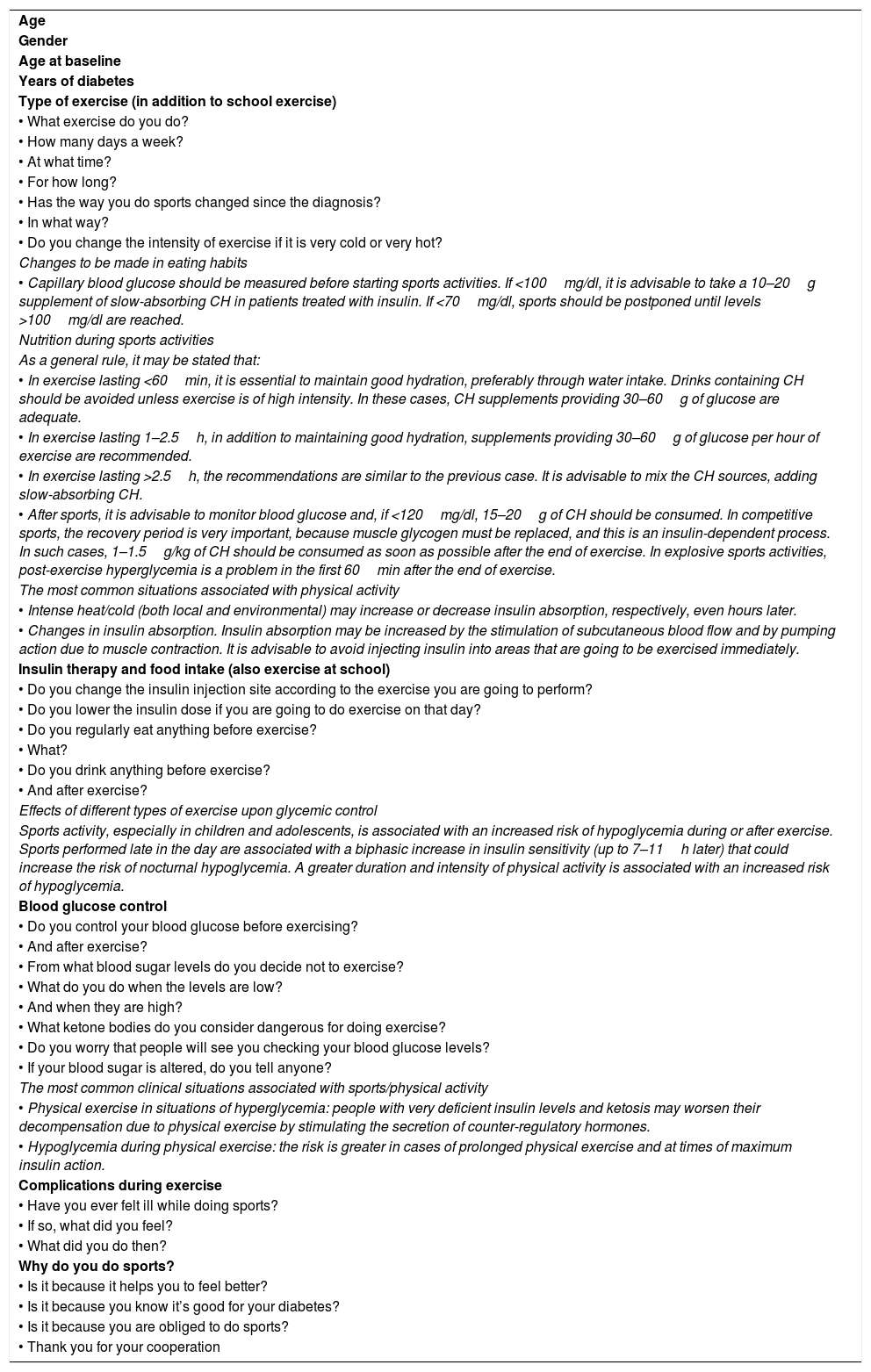
Adherence questionnaire.
| Age |
| Gender |
| Age at baseline |
| Years of diabetes |
| Type of exercise (in addition to school exercise) |
| • What exercise do you do? |
| • How many days a week? |
| • At what time? |
| • For how long? |
| • Has the way you do sports changed since the diagnosis? |
| • In what way? |
| • Do you change the intensity of exercise if it is very cold or very hot? |
| Changes to be made in eating habits |
| • Capillary blood glucose should be measured before starting sports activities. If <100mg/dl, it is advisable to take a 10–20g supplement of slow-absorbing CH in patients treated with insulin. If <70mg/dl, sports should be postponed until levels >100mg/dl are reached. |
| Nutrition during sports activities |
| As a general rule, it may be stated that: |
| • In exercise lasting <60min, it is essential to maintain good hydration, preferably through water intake. Drinks containing CH should be avoided unless exercise is of high intensity. In these cases, CH supplements providing 30–60g of glucose are adequate. |
| • In exercise lasting 1–2.5h, in addition to maintaining good hydration, supplements providing 30–60g of glucose per hour of exercise are recommended. |
| • In exercise lasting >2.5h, the recommendations are similar to the previous case. It is advisable to mix the CH sources, adding slow-absorbing CH. |
| • After sports, it is advisable to monitor blood glucose and, if <120mg/dl, 15–20g of CH should be consumed. In competitive sports, the recovery period is very important, because muscle glycogen must be replaced, and this is an insulin-dependent process. In such cases, 1–1.5g/kg of CH should be consumed as soon as possible after the end of exercise. In explosive sports activities, post-exercise hyperglycemia is a problem in the first 60min after the end of exercise. |
| The most common situations associated with physical activity |
| • Intense heat/cold (both local and environmental) may increase or decrease insulin absorption, respectively, even hours later. |
| • Changes in insulin absorption. Insulin absorption may be increased by the stimulation of subcutaneous blood flow and by pumping action due to muscle contraction. It is advisable to avoid injecting insulin into areas that are going to be exercised immediately. |
| Insulin therapy and food intake (also exercise at school) |
| • Do you change the insulin injection site according to the exercise you are going to perform? |
| • Do you lower the insulin dose if you are going to do exercise on that day? |
| • Do you regularly eat anything before exercise? |
| • What? |
| • Do you drink anything before exercise? |
| • And after exercise? |
| Effects of different types of exercise upon glycemic control |
| Sports activity, especially in children and adolescents, is associated with an increased risk of hypoglycemia during or after exercise. Sports performed late in the day are associated with a biphasic increase in insulin sensitivity (up to 7–11h later) that could increase the risk of nocturnal hypoglycemia. A greater duration and intensity of physical activity is associated with an increased risk of hypoglycemia. |
| Blood glucose control |
| • Do you control your blood glucose before exercising? |
| • And after exercise? |
| • From what blood sugar levels do you decide not to exercise? |
| • What do you do when the levels are low? |
| • And when they are high? |
| • What ketone bodies do you consider dangerous for doing exercise? |
| • Do you worry that people will see you checking your blood glucose levels? |
| • If your blood sugar is altered, do you tell anyone? |
| The most common clinical situations associated with sports/physical activity |
| • Physical exercise in situations of hyperglycemia: people with very deficient insulin levels and ketosis may worsen their decompensation due to physical exercise by stimulating the secretion of counter-regulatory hormones. |
| • Hypoglycemia during physical exercise: the risk is greater in cases of prolonged physical exercise and at times of maximum insulin action. |
| Complications during exercise |
| • Have you ever felt ill while doing sports? |
| • If so, what did you feel? |
| • What did you do then? |
| Why do you do sports? |
| • Is it because it helps you to feel better? |
| • Is it because you know it’s good for your diabetes? |
| • Is it because you are obliged to do sports? |
| • Thank you for your cooperation |
Italics show the section of the RECORD guidelines which the questions refer to. This text did not appear in the patient survey.
The data are expressed as percentages to facilitate understanding of the results, except in the case of small groups where the data are expressed as whole numbers. Quantitative variables are reported as the arithmetic mean and standard deviation (SD).
A total of 46 surveys were conducted (21 males and 25 females), with a mean age of 11.75 years (SD: 3.08, minimum 4 and maximum: 17.3); 67.4% were adolescents.
A total of 84.8% of those surveyed were involved in sports activities outside school. From the start of the disease, 13% maintained their previous physical activity, 8.6% performed less exercise, and 78.4% performed more exercise. Sports activities were performed an average of 2.57 days a week (SD: 1.63), with a mean duration per session of 1.14h (SD: 0.6).
In 73.9% of the cases sports activities were for fun (with no gender difference; 23 of them being adolescents), while 13% performed exercise because they considered it part of their treatment (4 females and 2 males; 50% adolescents), 10.8% did so due to parental obligation (3 females and 2 males), and the rest performed exercise for more than one of these reasons. The subjects involved in sports obliged by their parents showed significant differences (LR: p<0.05) between adolescents and prepubertal individuals, but not between genders.
As regards metabolic control, blood glucose control was common before exercise in 69.9% of the cases and afterwards in 47.8% of the cases, though 19.6% avoided blood glucose controls because they were embarrassed to be seen by their colleagues. There were no differences between pubertal stage and gender in this group. A total of 19.6% of the patients did not inform anyone of the glycemic control values obtained - most of them (n: 7) being adolescents (LR: p<0.05) - while 21.7% reported the values to their parents - most of them preadolescents (n: 8) - and 58.7% to their teachers or coaches (22 of them being adolescents).
Of those subjects who performed prior blood glucose testing, 6.5% participated in sports activities regardless of the values obtained, while the rest considered consuming carbohydrates before starting physical activity in the presence of low blood glucose levels, defined as 92mg/dl (SD: 31.3). Fifty percent did not perform sports with high glucose levels, taken to represent >258.7mg/dl (SD: 31.3).
With regard to the insulin dose administered in the previous hours, 63% did not modify the dose, 34.8% administered a lesser dose if sport was to be performed, and a single patient required a higher dosage. In turn, 67.4% did not change the site of insulin administration, while 17.4% modified it according to the activity to be performed. The remaining 15.2% had a continuous infusion pump.
Prior to physical exercise, 50% systematically consumed food, while 46% did so afterwards. Hydration was ensured with some type of drink prior to physical activity in 37% of the cases, and in 60.9% afterwards.
Of the patients surveyed, 33 had experienced hypoglycemia episodes during physical activity. The symptoms during these episodes were mainly tiredness (30%) or dizziness (22%). Less frequent symptoms were tremor (n: 6), abdominal pain (n: 2) or headache (n: 1). In the event of hypoglycemia symptoms, all subjects performed blood glucose controls and consumed carbohydrates. The rescue foods in this regard were cookies in 41.7% of the cases, sachets of glucose formulations in 19.4%, fruit juice in 19.4%, energy bars in 11.1%, yogurt drinks in 5.6%, and sachets of sugar in one patient. Cookies and juice were the preferred foods in younger patients, versus glucose tablets in adolescents (LR: p<0.05), with no gender differences.
Although there are a number of publications on the effects of sports activities upon metabolic control in pediatric patients with T1DM1 and on the recommendations for doing sports safely,3–5 we only found one study similar to our own that evaluated compliance with these standards.6 After analyzing our study population, we concluded that patients with DM1 globally perform sports activities adequately adjusted to their age. Behavior should be routinely examined to ensure safe exercise, for as demonstrated by the present study, some recommendations tend to be forgotten over the years. Our patients focused their attention on glycemic control, but often ignored the recommendations referring to intake and hydration before and after exercise. Roberts et al.6 presented similar results regarding changes in insulin administration, though they only included patients with insulin infusion pumps. The percentage of patients who ate immediately before exercise was higher in their series (70% versus 50% in our study). A particularly important aspect is the fact that while most of our patients experienced hypoglycemia during exercise, many of them did not inform anyone around them, with the risk that this implies. Our data coincide with those of other previously published series,7–10 in which adolescence represents a turning point in metabolic control, not only because of hormonal changes inherent to the body, but also because of the rejection of disease control, which leads to less physical activity and less safe exercise. However, the previously published study6 recorded no differences in relation to age, though the mean age of the patients was higher than in our sample, since it comprised patients between 10–18 years of age, their sample being more homogeneous in this regard.
Financial supportThe present study has not received specific financial support from public agencies, the commercial sector or from non-profit entities.
Thanks are due to all the patients who participated in the study.
Please cite this article as: Salamanca-Zarzuela B, Mulero-Collantes I, Morales-Luengo F, Centeno Malfaz F. Adherencia a las recomendaciones de la Guía RECORD en los pacientes con diabetes mellitus tipo 1 menores de 18 años. Endocrinol Diabetes Nutr. 2020;67:553–556.