Diabetes is the most common metabolic complication during pregnancy, and poses an increased risk of negative effects in relation to the obstetric and perinatal outcomes.1 The prevalence of coexisting pregestational diabetes, mainly type 1 diabetes mellitus (DM1), during pregnancy is 1–2%.1,2
A retrospective study was made of all women diagnosed with pregestational DM1 and their newborn infants during a 7-year period (2010–2017), following the creation of our pregestational diabetes clinic. Both the maternal and the newborn infant complications are described. We excluded patients diagnosed with type 2 diabetes mellitus (DM2), gestational diabetes, and those diagnosed with diabetes mellitus during pregnancy, as well as other types of diabetes.
A total of 39 pregnant women with pregestational DM1 and 33 newborn infants (48.7% girls) were evaluated, since data on 6 infants could not be retrieved. No miscarriages were recorded. A total of 56.4% of the women had undergone preconception consultation, and metabolic control was considered to be adequate for pregnancy.
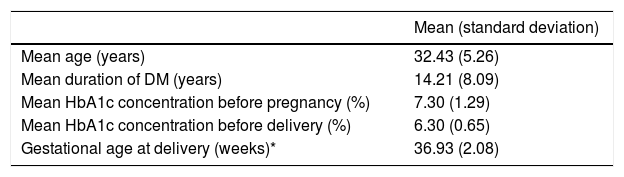
Table 1 shows the main characteristics of the study sample.
Principal characteristics of the study sample.
| Mean (standard deviation) | |
|---|---|
| Mean age (years) | 32.43 (5.26) |
| Mean duration of DM (years) | 14.21 (8.09) |
| Mean HbA1c concentration before pregnancy (%) | 7.30 (1.29) |
| Mean HbA1c concentration before delivery (%) | 6.30 (0.65) |
| Gestational age at delivery (weeks)* | 36.93 (2.08) |
| Percentage | |
|---|---|
| Thyroid disease (%) | 41 |
| Nephropathy (%) | 10 |
| Polyhydramnios (%) | 2.6 |
| Pre-eclampsia (%) | 20.5 |
| Intrauterine growth restriction (%) | 10.3 |
| Threatened preterm labor (%) | 7.7 |
| Genitourinary infections (%) | 30.8 |
| CSII/MDI (%) | 42.1/57.9 |
| Preterm deliveries (%) | 30.8 |
| Caesarean sections (%) | 61.5 |
| Macrosomia (%) | 33.3 |
DM = diabetes mellitus; MDI = multiple dose insulin; CSII = continuous subcutaneous insulin infusion.
Of note was the high proportion of patients receiving subcutaneous insulin infusion, as well as the proportion of patients with autoimmune thyroid disease (25% with Graves-Basedow’s disease, 75% with primary autoimmune hypothyroidism). The mean HbA1c levels exhibited a progressive and significant decrease from before pregnancy to the time before delivery (−1% on average; p < 0.001).
No serious obstetric complications related to diabetes were recorded, though a percentage had diabetic nephropathy with positive microalbuminuria before pregnancy, with no worsening during gestation. There were no macrovascular complications.
A high percentage of preterm deliveries were recorded, with full-term deliveries in 69.2% of the cases. Most deliveries were by caesarean section, versus 20.5% eutocic deliveries and 18% instrumented deliveries. The number of induced deliveries could not be established.
The mean (± standard deviation [SD]) birth weight was 3090.49 ± 747.29 g (range 1260–4290), with a high percentage of macrosomia (weight percentile >90). A positive and significant linear correlation was observed (r = 0.35), between HbA1c concentration and fetal weight during the third trimester (p < 0.05), i.e., the higher the HbA1c value, the greater the fetal weight.
In all, 56.41% of the newborn infants required hospital admission (43.6% in Neonatology, 12.8% in the Neonatal Intensive Care Unit [NICU]), with a mean stay of 10.5 ± 9.5 and 5 ± 5.09 days, respectively. A total of 42.4% presented hypoglycemia, and 85.7% required admission for treatment. In addition, 6.1% presented hypocalcemia, while 15.2% exhibited polyglobulia, and 60% required intravenous fluid therapy. Furthermore, a total of 36.4% presented neonatal jaundice, requiring phototherapy in 50% of the cases. One-third of the infants (33.3%) presented acute respiratory distress (respiratory support proving necessary in 72.7%). There was only one case of perinatal death due to panenterocolitis in the context of extreme prematurity. Echocardiography was performed in 48.6% of the newborn infants, with normal findings in only 6.1%. The most common finding was septal hypertrophy (12.1%).
The objective of strict metabolic control in pregnant women with diabetes is to avoid maternal complications and fetal problems. In fact, observational studies show that the risk of fetal malformations is mainly related to poor glycemic control in the first weeks of pregnancy (i.e., the period of organogenesis); the optimization of control should therefore be started before conception. However, it is well known that a considerable percentage of patients do not plan pregnancy.3,4 Kernaghan et al.4 reported that women who plan pregnancy have a lower HbA1c concentration and therefore a lower obstetric complications rate than women who do not previously plan pregnancy. Wahabi et al.,5 in their meta-analysis, found that pregestational care reduces HbA1c in the first trimester by an average of 1.92%, and that effective pregestational control reduces congenital malformations and perinatal mortality. In our series, the high percentage of women treated with continuous subcutaneous insulin infusion (CSII) reflects attempts to secure the best possible metabolic control before and during pregnancy.
Johnstone et al.,6 in coincidence with our own findings, reported a positive correlation between HbA1c levels in the third trimester and birth weight. They also found this correlation to be negative during the first trimester of pregnancy, because higher HbA1c levels imply lesser placental development, which results in increased intrauterine growth restriction (IUGR) and prematurity. It should be noted that Yves et al.7 reported children of women with DM1 as having greater weight than the control group.
The delivery route depends on both the mother and on fetal monitoring. No specific modality is recommended. Although it has been reported that macrosomic fetuses are characterized by greater cephalic-pelvic disproportion, this does not entail any specific recommendation for caesarean section. Yves et al.7 reported a higher percentage of caesarean sections versus the global obstetric population studied. This was also seen in our series, where the percentage of caesarean sections in these women (61.5%) was much higher than the overall percentage of caesarean sections at the center (24.8%).
Another complication of children of diabetic mothers is cardiac malformations. In this regard, it is important to perform a complete cardiological examination. Septal hypertrophy is the predominant finding, and is due to increased glycogen deposition in the myocardial cells. Passarella et al.8 reported septal hypertrophy in 35.4% of cases. This percentage is greater than in our study, perhaps because echocardiography was not performed in all patients, since echocardiography is not routinely performed in our center in infants born to diabetic mothers.
In conclusion, despite the creation of specific gestational control units, the maternal-fetal complications rate remains high. New tools are needed to facilitate improved metabolic control in this subgroup of patients.
Please cite this article as: González-Lamuño C, Díaz G, García S, Matías V, Alvarez C, Bahíllo Mª.P. Complicaciones obstétricas y perinatales en la diabetes tipo 1: estudio retrospectivo unicéntrico. Endocrinol Diabetes Nutr. 2020;67:556–558.