Physical activity (PA) is highly recommended in type 1 diabetes (T1D). Few studies have reported the amount of PA performed by individuals with T1D in their daily life, and there is no information about changes over time.
Material and methodsCross-sectional study in patients with T1D from a referral hospital recruited in two different periods: data from the Biobank registers from 2009 and data from patients attending visits at the hospital in 2019, on a consecutive basis. Data included clinical characteristics and the PA assessment through the International Physical Activity Questionnaire-short form (IPAQ-SF).
ResultsIn 2019, participants with T1D (n=135) reported a lower sedentary lifestyle and greater levels of high PA compared to subjects with T1D (n=355) from 10 years earlier (6.7% vs. 14.1% sedentariness, p=0.015; and 52.6% vs. 25.4% of high PA, p<0.001, respectively). Similar results were identified when the groups were divided according to sex. Both groups presented similar distribution by sex (women, 54% vs. 55%), age (40 vs. 39 years old), years with diabetes (20 vs. 18 years), BMI (25 vs. 24kg/m2) and glycated haemoglobin (7.5% vs. 7.5%, respectively; p>0.05 for all comparisons). Sex and age groups were not determinant for sedentary lifestyle in the different years studied.
Analysing all the 490 participants, there was an inverse correlation of age with sitting hours (p=0.024, r=−0.102), total METs (p<0.001, r=−0.146) and HbA1c (p=0.038, r=−0.097). No correlations were found between PA and HbA1c or BMI.
ConclusionsThe findings indicate that PA has significantly increased in subjects with T1D over the last 10 years. Future studies are needed to assess whether these healthier habits translate into better outcomes in this high-risk population.
La actividad física (AF) es altamente recomendada en la diabetes tipo 1 (DM1). Pocos estudios han mostrado la cantidad de AF realizada por los individuos con DM1 en su vida diaria, y no hay información sobre los cambios en el tiempo.
Material y métodosEstudio transversal en pacientes con DM1 de un hospital de referencia reclutados en dos periodos diferentes: datos de registro del Biobanco en 2009 y datos de pacientes que estaban en visitas en el hospital en 2019, incluidos de forma consecutiva. Los datos incluyeron las características clínicas y la valoración de la AF mediante el International Physical Activity Questionnaire-short form (IPAQ-SF).
ResultadosEn el 2019, los participantes con DM1 (n = 135) refirieron un menor sedentarismo y mayores niveles de AF alta, en comparación con los sujetos con DM1 (n = 355) de 10 años previos (6,7 vs. a 14,1% de sedentarismo, p = 0,015; y 52,6% vs. 25,4% de AF alta, p < 0,001, respectivamente). Resultados similares fueron identificados cuando los grupos fueron divididos por sexo. Ambos grupos presentaron una distribución similar por sexo (mujeres, 54 vs. 55%), edad (40 vs. 39 años), años de evolución de la diabetes (20 vs. 18 años), índice de masa corporal ([IMC] 25 vs. 24 kg/m2) y hemoglobina glicada ([HbA1c] 7,5 vs. 7,5%; respectivamente; p > 0,05 para todas las comparaciones). El sexo y los grupos de edad no fueron determinantes para el sedentarismo en los diferentes años estudiados.
Analizando el total de los 490 participantes, se identificó una correlación inversa entre edad y horas-sentado (p = 0,024, r = -0,102), MET totales (p < 0,001, r = -0,146) y HbA1c (p = 0,038, r = -0,097). No fueron identificadas correlaciones entre AF y HbA1c o IMC.
ConclusionesLos resultados indican que la AF ha aumentado significativamente en los sujetos con DM1 en los últimos diez años. Son necesarios futuros estudios para evaluar si estos hábitos más saludables se traducen en mejores resultados en esta población de alto riesgo.
Physical inactivity is increasing and represents a leading risk factor for global mortality.1 There is clear evidence demonstrating that physical activity (PA) contributes to overall health.2 In people with type 1 diabetes (T1D), PA has additional benefits such as improvement in glycaemic control, and helps to decrease cardiovascular risk factors, chronic complications, cardiovascular disease and overall mortality.3–8 However, when performing PA, patients with T1D must manage fluctuations in glycaemic control which can hinder its practice.9
Few studies have reported the amount of PA performed by individuals with T1D in their daily life, and there is no information about changes over time. We aimed to evaluate self-reporting of usual PA levels in two different samples of participants with T1D recruited 10 years apart.
Patients and methodsPatients with T1D from a referral hospital were recruited in two periods: from 2008 to 2010 (hereinafter 2009) and in 2019. Data from the 2009 group was obtained from the Biobank registers of the hospital. It included clinical characteristics and the International Physical Activity Questionnaire-short form (IPAQ-SF).10 Within the context of their usual clinical visit with an endocrinologist or education nurse, the patients from 2019 were specifically invited to participate in the present study on a consecutive basis.
The following data were registered: age, sex, diabetes duration, use of continuous subcutaneous insulin infusion (CSII) or multiple doses of insulin (MDI) and evaluation of PA by IPAQ-SF. Weight, height, body mass index (BMI) and glycated haemoglobin (HbA1c) were obtained from medical records.
According to the IPAQ-SF score, each individual was classified as high, moderate, or low PA; low PA is also labelled as sedentariness or sedentary lifestyle. In addition, the estimated metabolic equivalent of task (MET) was calculated, and sitting hours per day were registered.
The continuous variables were tested for normality using the Shapiro–Wilk test. Non-parametric variables from the two different periods were compared with the Mann–Whitney U test. The Spearman test was used to establish correlations among variables. The chi-square was used to analyse difference between categorical variables. SPSS v26 (IBM SPSS Statistics, Chicago, IL) was used for statistical analysis. Significance was considered with p<0.05.
ResultsOverall, 355 patients with T1D were studied in 2009 and 135 in 2019. The characteristics of the participants are presented in Table 1. Briefly, the clinical features were similar in both groups, except for the use of CSII, which was more frequently used in 2019 (6.9% vs. 26.7%; p<0.001), and higher BMI was identified in women from 2019 when compared to women from 2009 (p=0.035).
Clinical characteristics of patients in 2009 and 2019. Total and separated by sex.
| 2009 | 2019 | p | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Women | Men | Total | Women | Men | Total | Women | Men | |
| n | 355 | 196 | 159 | 135 | 73 | 62 | 0.45 | – | – |
| Age (years) | 39 [29–48] | 39 [30–48] | 38 [28–49] | 40 [25–52] | 44 [28–53] | 36 [23–51] | 0.572 | 0.126 | 0.453 |
| Diabetes duration (years) | 18 [11–27] | 19 [11–26] | 17 [10–27] | 20 [10–30] | 25 [12–30] | 19 [9–25] | 0.15 | 0.063 | 0.849 |
| BMI (kg/m2) | 24.42 [21.88–26.71] | 23.8 [21.45–26.22] | 24.84 [22.53–26.87] | 25.15 [21.89–28.63] | 25.56 [21.59–29.02] | 24.73 [22.03–28.4] | 0.06 | 0.035 | 0.72 |
| CSII (%) | 6.8 | 9.7 | 3.1 | 26.7 | 32.9 | 19.4 | <0.001 | <0.001 | <0.001 |
| HbA1C(%) | 7.5 [6.7–8.4] | 7.6 [6.7–8.4] | 7.4 [6.8–8.4] | 7.4 [6.8–8] | 7.5 [6.8–8] | 7.3 [6.8–8.2] | 0.512 | 0.523 | 0.761 |
| Sitting hours (hours/day) | 6 [3–8] | 6 [4–8] | 6 [3–8] | 5 [3–7] | 5 [3–7] | 5 [3–7] | 0.258 | 0.359 | 0.466 |
| Total METs (by IPAQ-SF) | 1626 [777–2970] | 1386 [693–2364 | 2079 [942–3930] | 2772 [1485–4679] | 2346 [1386–3870] | 3519 [1902–6624] | <0.001 | <0.001 | <0.001 |
| PA in 3 categories (by IPAQ-SF) | |||||||||
| Sedentariness/low (% in category) | 14.1 | 13.8 | 14.5 | 6.7 | 6.8 | 6.5 | 0.015 | 0.085 | 0.075 |
| Moderate (% in category) | 60.6 | 66.3 | 52.2 | 40.7 | 53.4 | 25.8 | <0.001 | 0.036 | <0.001 |
| High (% in category) | 25.4 | 19.4 | 32.7 | 52.6 | 39.4 | 67.7 | <0.001 | 0.001 | <0.001 |
Bold numbers highlight statistical significant values.
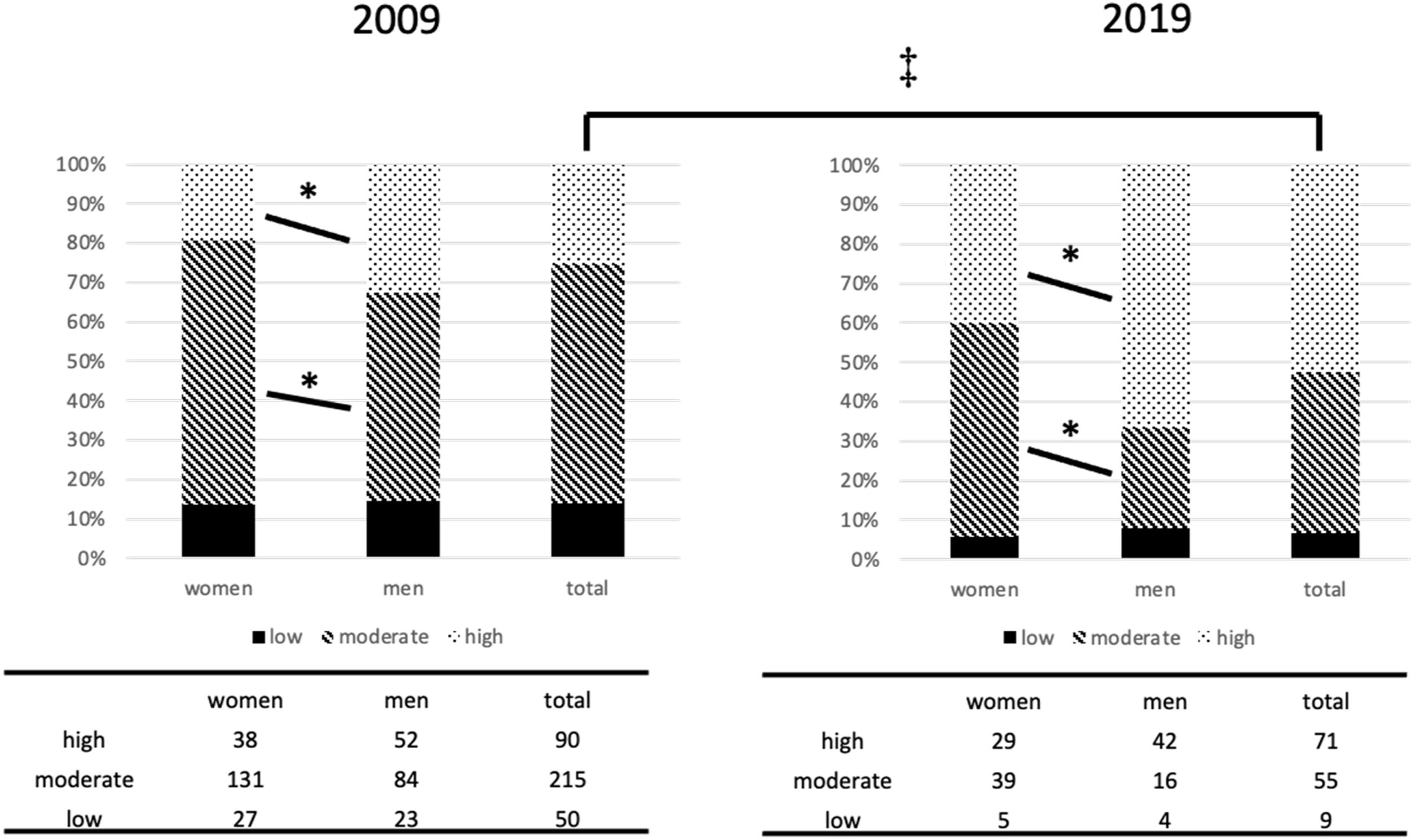
Participants from 2019 were more active (p<0.001) and presented a higher MET (p<0.001) than those from 2009. Regarding sedentary lifestyle, in 2009 14.1% patients were classified as sedentary compared to 6.7% in 2019 (p=0.015) (Table 1, Fig. 1). Similar results were identified when the groups were divided according to sex. Women and men presented a different proportion of moderate or high PA (2009: p=0.005 for moderate PA and p=0.001 for high PA; 2019: p=0.003 for moderate PA and p=0.001 for high PA). Both groups, however, presented a similar number of sitting hours per day.
Physical activity categories in women and men in 2009 and 2019. ‡ Between total 2009 and 2019: p=0.015 for low PA, p<0.001 for moderate PA and p<0.001 for high PA. * 2009: p=0.005 for moderate PA and p=0.001 for high PA, between women and men. * 2019: p=0.003 for moderate PA and p=0.001 for high PA, between women and men.
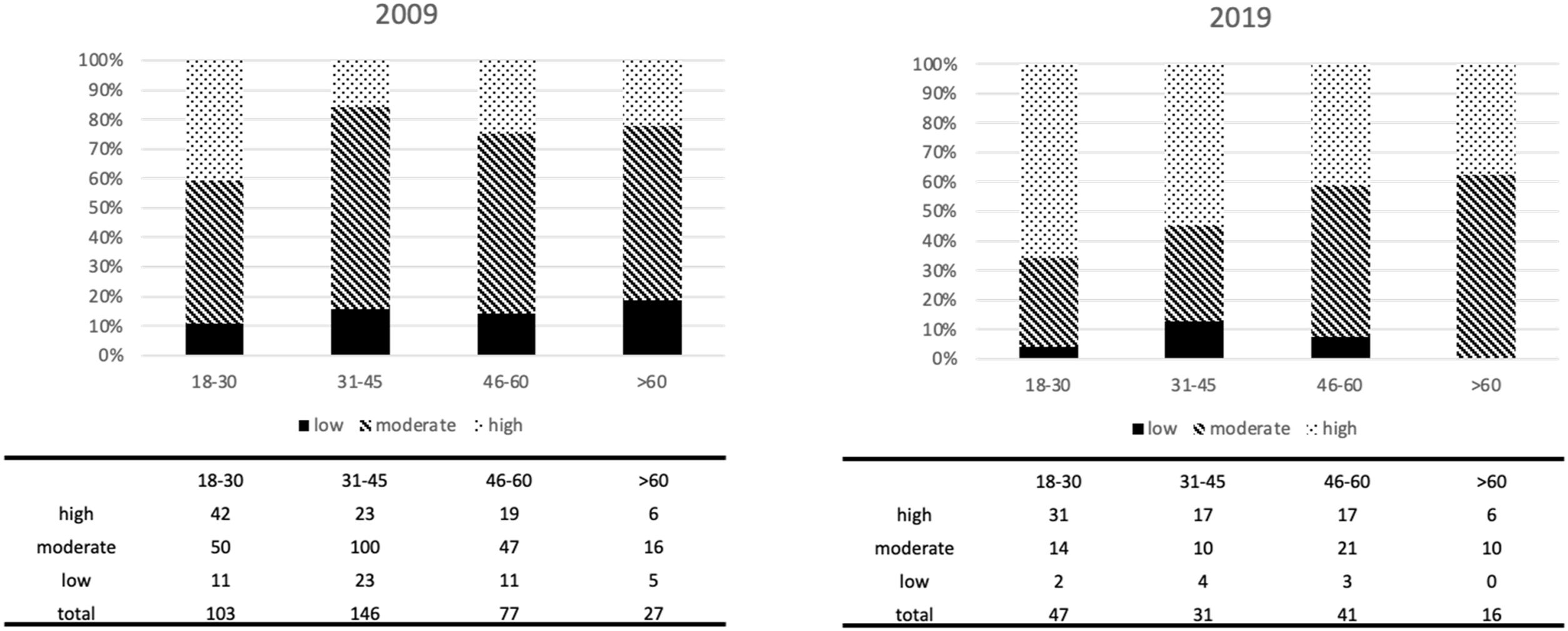
The analysis according to age groups showed that there were no differences in sedentary lifestyle among these groups, both in 2009 and in 2019 (Fig. 2). Groups presented a different proportion of moderate or high PA with the change of age group (2009: p=0.017 for moderate PA and p<0.001 for high PA; 2019: p=0.041 for moderate PA).
An analysis of all the 490 participants, but split by sex, was also performed. The characteristics of the participants, now separated by sex, are presented in Table 2. The main difference between women and men is that men reported more hours of high PA, while both groups presented the same rates of sedentariness and sitting hours per day. In parallel with the differences of PA, women presented lower BMI and used more CSII than men (p<0.05).
Clinical characteristics of all the patients recruited in the study (2009 and 2019 groups together), separated by sex.
| Women | Men | p | |
|---|---|---|---|
| n | 269 | 221 | |
| Age (years) | 40 [29–50] | 37 [27–49] | 0.091 |
| Diabetes duration (years) | 20 [12–29] | 18 [10–27] | 0.185 |
| BMI (kg/m2) | 24.27 [21.45–26.73] | 24.84 [22.49–27.38] | 0.026 |
| CSII (%) | 16 | 7.7 | 0.004 |
| HbA1C(%) | 7.5 [6.7–8.3] | 7.4 [6.8–8.3] | 0.626 |
| Sitting hours (hours/day) | 5 [3–8] | 6 [3–8] | 0.289 |
| Total METs (by IPAQ-SF) | 1470 [864–2772] | 2415 [1215–4464] | <0.001 |
| PA in 3 categories (by IPAQ-SF) | |||
| Sedentariness/low (% in category) | 11.9 | 12.2 | 0.511 |
| Moderate (% in category) | 62.8 | 44.8 | <0.001 |
| High (% in category) | 24.9 | 42.5 | <0.001 |
Bold numbers highlight statistical significant values.
Among all 490 participants, there was an inverse correlation of age with sitting hours (p=0.024, r=−0.102), total MET (p<0.001, r=−0.146) and HbA1c (p=0.038, r=−0.097). Participants with CSII presented more diabetes duration (25 [18–34] vs. 18 [10–27] years, p<0.001) and fewer sitting hours (4.2 [3–6] vs. 6 [4–8] hours, p=0.005) than those receiving MDI. No correlations were found between PA and HbA1c or BMI.
Correlation studies were also performed separately for the groups of the different years. In the group from 2009, it could be confirmed that there was an inverse correlation of age with total METs (p=0.01, r=−0.137), but not with sitting hours or HbA1c. In this group, the use of CSII was not associated with PA, but with worse glycaemic control (HbA1c 8.25% [7.69–8.35] vs. 7.5% [7.41–7.71], p=0.023) and more years with diabetes (19.5 [18.15–27.75] vs. 19 [18.4–21.02] years, p=0.035). The same analysis was made for the 2019 group, and an inverse correlation of age with total MET was identified (p=0.003, r=−0.254) and HbA1c (p=0.018, r=−0.204), but not with sitting hours. Participants with CSII from 2019 presented similar glycaemic control (HbA1c 7.5% [7.28–7.91] vs. 7.3% [7.3–7.72], p=0.371), but more diabetes duration (25 [22.92–30.28] vs. 19 [17.68–23.02] years, p=0.004) than those receiving MDI.
DiscussionPA levels increased in patients with T1D over a 10-year period, with a significant reduction of sedentary lifestyle. In addition, we found characteristics associated with fewer sitting hours, such as increasing age and being on CSII therapy. In a previous populational study carried out in Spain in 2009,11 using the same questionnaire (IPAQ-SF), the rate of self-reporting sedentary lifestyle was around 38% in people without diabetes, far from that obtained in subjects with T1D in our study (14.1% in 2009, and 6.9% in 2019). These results could suggest that visits with endocrinologists and education nurses, and access to educational courses for diet, PA and self-treatment management, promotes healthy behaviours.12
Some previous studies analysed PA in children, adolescents and adults with T1D and compared them with people without diabetes, reporting that subjects with T1D were less physically active.13-15 According to those studies, the differences were attributed to having diabetes, loss of control over diabetes and the risk of hypo- or hyperglycaemia. Notwithstanding, several recent studies are focused on helping patients and healthcare professionals to overcome these and other barriers for this population to perform PA.16,17
In contrast to persons with type 2 diabetes, PA in T1D is not always associated with improvements in glycaemic control, as shown in our study. Carbohydrate intake, the type and amount of exercise, and insulin doses are several factors that can influence glycaemic control.17 Nevertheless, it is known that PA is associated with a reduction of cardiovascular risk factors and mortality.7,8
Both women and men increased PA from 2009 to 2019 in the present study. Men, however, reported more high PA than women. Comparing again with population studies, women usually present higher levels of sedentary lifestyle, such as, for example, 34.9% (30.6–39.2) vs. 27.3% (23.2–31.5) in men in a study with data from 2002,18 or 39% (IC 37.1–40.8) vs. 32.3% (IC 30.3–34.3) in a study with data from 2009.11 These numbers were not confirmed in the present study, where men and women presented similar rates of sedentariness and these rates reduced over 10 years.
The limitations of the study include the lack of evaluation of hypoglycaemic episodes or barriers to PA. Second, we did not evaluate the same patients over time. In this sense, since data from the Biobank registry is anonymous, we cannot ascertain if any of the patients recruited in the first group were also included in the second group. However, considering that the key clinical characteristics of the participants (age and years with diabetes) were similar, this probably reflects that they were two non-related groups. Third, because of the long time period between the two questionnaires (10 years), we cannot rule out that the changes in PA observed were due to causes other than our educational programme and healthcare professionals. Finally, since the recruitment of the participants was not performed on a probabilistic basis, the study group could not be representative of the overall patients followed up in our institution. However, the main characteristics (age, sex and diabetes duration) of our patients were very similar to the adult population included in the SED1 study (a study specially designed to be representative of the Spanish population with T1D,19 which supports the extrapolation of our results. On the other hand, one strength of this study was the use of the same IPAQ-SF in two populations which were very similar in most of the key characteristics (age, sex and BMI) and in the same setting.
In conclusion, the findings of this study indicate that PA has significantly increased in T1D subjects over the last 10 years. Future studies are needed to assess whether these healthier habits translate into better outcomes in this high-risk population.
Authors’ contributionsLB, AH and EE conceptualised and designed the research; AH, AA, DR, MG, NS, IC and EE performed the data collection; LB, and AH performed the statistical analysis; LB, AH and AA drafted the manuscript; all authors interpreted the results and edited, revised and approved the final version.
Ethics approvalPart of the clinical data was facilitated by HCB-IDIBAPS Biobank, which provides de-identified clinical data. The HCB-IDIBAPS Biobank protocols are in accordance with the ethical standards of our institution and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The complete study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics and Research Committee of Hospital Clínic de Barcelona. Approval number: HCB/2019/0715. Date of approval: 17 December 2019; addendum 29 April 2021.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Conflict of interestsThe authors declare that they have no conflict of interest.
We are indebted to the HCB-IDIBAPS Biobank for human data procurement. We are also grateful to the subjects who participated in the study.