Radiofrequency ablation (RFA) plays an increasing role in the management of thyroid nodules. The purpose of this study was to evaluate the safety and efficacy of RFA of benign thyroid nodules in terms of volume reduction and symptom relief.
MethodsWe reviewed the medical records of patients with a solitary thyroid nodule who received RFA at our centre from April 2016 to January 2020. Ultrasound-guided RFA was performed by the moving-shot technique. Patients were followed up with ultrasound examinations and thyroid function tests. We evaluated changes in volume and in compressive (0–10 scale) and cosmetic (4-point scale) symptoms to analyse efficacy and complications, and in thyroid function to evaluate safety.
ResultsA total of 72 patients were included in the study. The mean follow-up was 11.1±0.7 months. There was a statistically significant reduction in size of the nodules at Month 1, 3, 6 and 12 after RFA (expressed as volume reduction rate: 34%±2.1, 50.8%±2.2, 60.3%±2.6, 58.87%±3.5, p<0.0001). We found statistically significant improvement in compressive symptoms (from 7.1±0.26 to 1.76±0.33, p<0.0001) and in cosmetic alteration (from 3.66±0.09 to 2.14±0.14, p<0.0001). No major complications were observed.
DiscussionRFA achieved significant volume reduction and improved compressive symptoms as well as cosmetic complaints, with minimum side effects. Our results are in line with recent available evidence and further support the use of RFA as a safe and effective therapeutic option in the management of benign thyroid nodules.
La ablación por radiofrecuencia (ARF) desempeña un papel cada vez más importante en el tratamiento de los nódulos tiroideos. El objetivo de este estudio fue evaluar la seguridad y la eficacia de la ARF en los nódulos tiroideos benignos en términos de reducción del volumen y alivio de los síntomas.
MétodosRevisamos la historia clínica de pacientes con un nódulo tiroideo único que recibieron ARF en nuestro centro desde abril del 2016 hasta enero del 2020. La ARF guiada por ecografía se realizó mediante la técnica de disparo en movimiento. Se realizó un seguimiento de los pacientes con exploraciones ecográficas y pruebas de la función tiroidea. Evaluamos los cambios en el volumen y en los síntomas compresivos (escala de 0 a 10) y estéticos (escala de 4 puntos) para analizar la eficacia y las complicaciones, y en la función tiroidea para evaluar la seguridad.
ResultadosSe incluyó a un total de 72 pacientes en el estudio. La media de seguimiento fue de 11,1 ± 0,7 meses. Hubo una reducción estadísticamente significativa en el tamaño de los nódulos en los meses 1, 3, 6 y 12 después de la ARF (expresado como tasa de reducción del volumen: 34% ± 2,1; 50,8% ± 2,2; 60,3% ± 2,6; 58,87% ± 3,5; p < 0,0001). Hallamos una mejora estadísticamente significativa en los síntomas de compresión (de 7,1 ± 0,26 a 1,76 ± 0,33; p < 0,0001) y en la alteración estética (de 3,66 ± 0,09 a 2,14 ±0,14; p < 0,0001). No se observaron complicaciones importantes.
DiscusiónLa ARF alcanzó una reducción significativa del volumen y mejoró los síntomas compresivos, así como las molestias estéticas, con efectos secundarios mínimos. Nuestros resultados están en línea con la evidencia disponible reciente y respaldan aún más el uso de ARF como opción terapéutica segura y eficaz en el tratamiento de nódulos tiroideos benignos.
Thyroid nodules are a common clinical finding, and their prevalence is increasing due to better ultrasound techniques and the extended use of radiological tests.1,2 Thyroid nodules can be detected in 19–68% of randomly selected individuals using high-resolution ultrasound (US), with higher frequencies in female and elderly patients.3 The main objective of the evaluation of a patient with a thyroid nodule is to assess its probability of malignancy. International guidelines recommend US to evaluate the characteristics of the nodule. If malignancy cannot be reasonably discarded, fine needle aspiration (FNA) biopsy should be used to confirm the presence or absence of malignancy.3,4 Most thyroid nodules (85–93%) are benign.5
Not all benign thyroid nodules require treatment, but this may be considered for symptoms such as neck pain, dysphagia, foreign body sensation, discomfort, cough, or cosmetic alteration.6 Surgical treatment is effective, but it can lead to mild to severe complications such as laryngeal nerve injury or hypoparathyroidism, in addition to the cosmetic alteration due to the scar.7 Nonsurgical therapy may therefore have a role in the management of benign thyroid nodules,8 and minimally invasive techniques have been tested and are already being used for treating them.9–11 One such technique is radiofrequency ablation (RFA).
RFA is a minimally invasive treatment for non-cystic nodules, based on an external radiofrequency generator that is connected to an electrode needle. The latter determines an increase of local temperature (between 60 and 100°C). The result is coagulative necrosis of the area around the needle.9 Effectiveness, safety, and clinical efficacy have been demonstrated in terms of nodule volume reduction, and improvement in symptom and cosmetic results.9,12–21 Low rates of major complications are described, such as injury of the laryngeal or vagus nerve that can lead to voice changes, brachial plexus damage, nodule rupture, or rare thyroid function changes. Minor complications include bleeding and subsequent haematoma, pain, skin burns, infection, cough, or vomiting.22,23
RFA has been included as a therapeutic option in the treatment of non-functioning benign thyroid nodules at the Hospital Universitario Central de Asturias (HUCA) since 2016. HUCA is a third-level hospital, with an assigned population of approximately 330,000. The aim of this retrospective study was to evaluate the efficacy and safety of RFA in the treatment of benign thyroid nodules.
Materials and methodsThis is a descriptive study carried out using the data obtained during the RFA process and the subsequent analytical and ultrasonographic follow-up. Ethical approval for this study was obtained from the ethics committee of the Hospital Universitario Central de Asturias. Verbal informed consent was obtained.
PatientsWe reviewed the medical records of patients with a solitary thyroid nodule who had a single RFA at our centre from April 2016 to January 2020. According to our protocols, patients were eligible for RFA only if they were aged over 18, the ultrasound pattern of the nodule was solid or mixed, and the nodule was benign (Bethesda class II) at two consecutive cytological assessments performed ≥3 months apart.
Prior to treatment, all patients were evaluated by clinical and ultrasound examination and by laboratory blood tests.
ProcedureThe patient was placed in the supine position and with mild neck extension under conscious sedation after a local US-guided lidocaine injection to achieve thyroid capsule anaesthesia. All RFA treatment procedures were performed on an outpatient basis. Blood pressure, electrocardiogram, heart rate and SpO2 were monitored in a non-invasive manner. All procedures were performed under ultrasound guidance, using the trans-isthmic approach and “moving-shot” technique. The RFA system includes a M-3004 generator with a maximum power of 200W at a frequency of 400kHz and an 18-gauge internally cooled electrode with a 1–2cm exposed tip (RF Medical Co., Seoul, Republic of Korea). The primary ablation energy was set at 25W, and it could be increased until 60W. The mean duration time of the treatment was around 12min. At the end of the RFA, an ice pack was applied to the patient's neck. They remained under observation for approximately 2h, and were discharged with a prescription for a mild analgesic, if necessary.
Follow-upPatients underwent periodical ultrasound examinations using an Aplio 500 ultrasound system (Toshiba Medical System, Japan), and thyroid function tests.
The difference in nodule volume vs baseline is called the volume reduction rate (VRR) and it is calculated according to the following formula: (initial volume−final volume)×100/initial volume.
Pain during treatment was evaluated on a 0–4 point scale, and patients were also asked about the presence and reversibility of complications classified as mild, intermediate and severe.
Patients were asked about cosmetic and pressure symptoms prior to and after RFA using two scales:
- -
Cosmetic alterations were evaluated on a 4-point scale as follows: 1, nodule not visible and not palpable; 2, nodule palpable but not visible; 3, nodule palpable and visible from nearby; 4, nodule palpable and visible from a distance.
- -
Pressure symptoms were evaluated on a 0–10 scale, where 0 indicates the absence of compression and 10, an important compression that causes serious symptoms and affects the patient's quality of life.
In the before and after treatment comparison, patients with the lowest score in cosmetic and pressure symptoms were not included as they had no options for improvement.
Prior to RFA, thyroid function was analysed, and categorised as hyperthyroidism (TSH<0.25mU/L), euthyroidism (TSH: 0.25–5mU/L), or hypothyroidism (TSH>5mU/L).
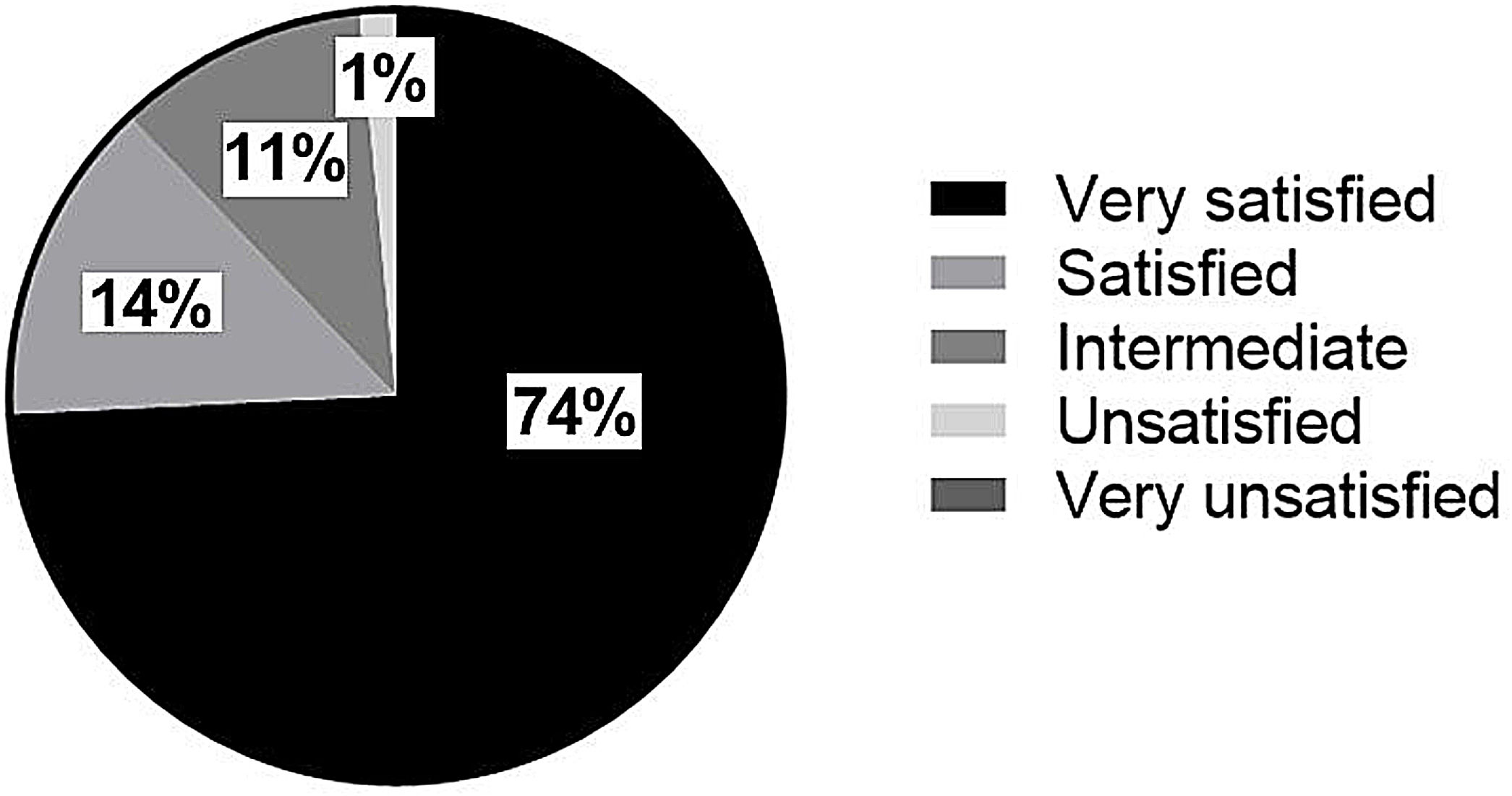
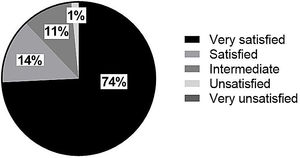
Finally, patients were asked about their global perception of improvement (yes/no), degree of satisfaction (very unsatisfied, unsatisfied, intermediate, satisfied and very satisfied) and willingness to repeat the procedure (yes/no/doubtful) in case of necessity.
Statistical analysisAnalysis was performed using GraphPad Prism, 8.0.1 version (GraphPad Software Inc., San Diego, USA). Data are expressed as mean±SEM. Statistical differences in continuous variables were evaluated by the T student test and the Wilcoxon test according to whether they were parametric, non-parametric or ordinal variables. Significance level was defined as p<0.05.
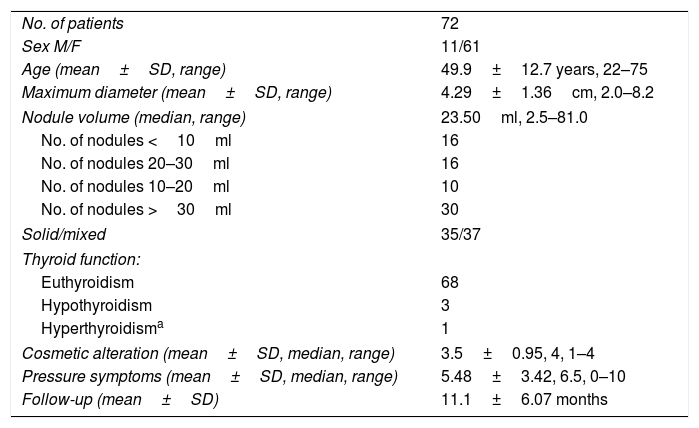
ResultsA total of 72 patients received RFA treatment. General characteristics are shown in Table 1.
Patient characteristics.
| No. of patients | 72 |
| Sex M/F | 11/61 |
| Age (mean±SD, range) | 49.9±12.7 years, 22–75 |
| Maximum diameter (mean±SD, range) | 4.29±1.36cm, 2.0–8.2 |
| Nodule volume (median, range) | 23.50ml, 2.5–81.0 |
| No. of nodules <10ml | 16 |
| No. of nodules 20–30ml | 16 |
| No. of nodules 10–20ml | 10 |
| No. of nodules >30ml | 30 |
| Solid/mixed | 35/37 |
| Thyroid function: | |
| Euthyroidism | 68 |
| Hypothyroidism | 3 |
| Hyperthyroidisma | 1 |
| Cosmetic alteration (mean±SD, median, range) | 3.5±0.95, 4, 1–4 |
| Pressure symptoms (mean±SD, median, range) | 5.48±3.42, 6.5, 0–10 |
| Follow-up (mean±SD) | 11.1±6.07 months |
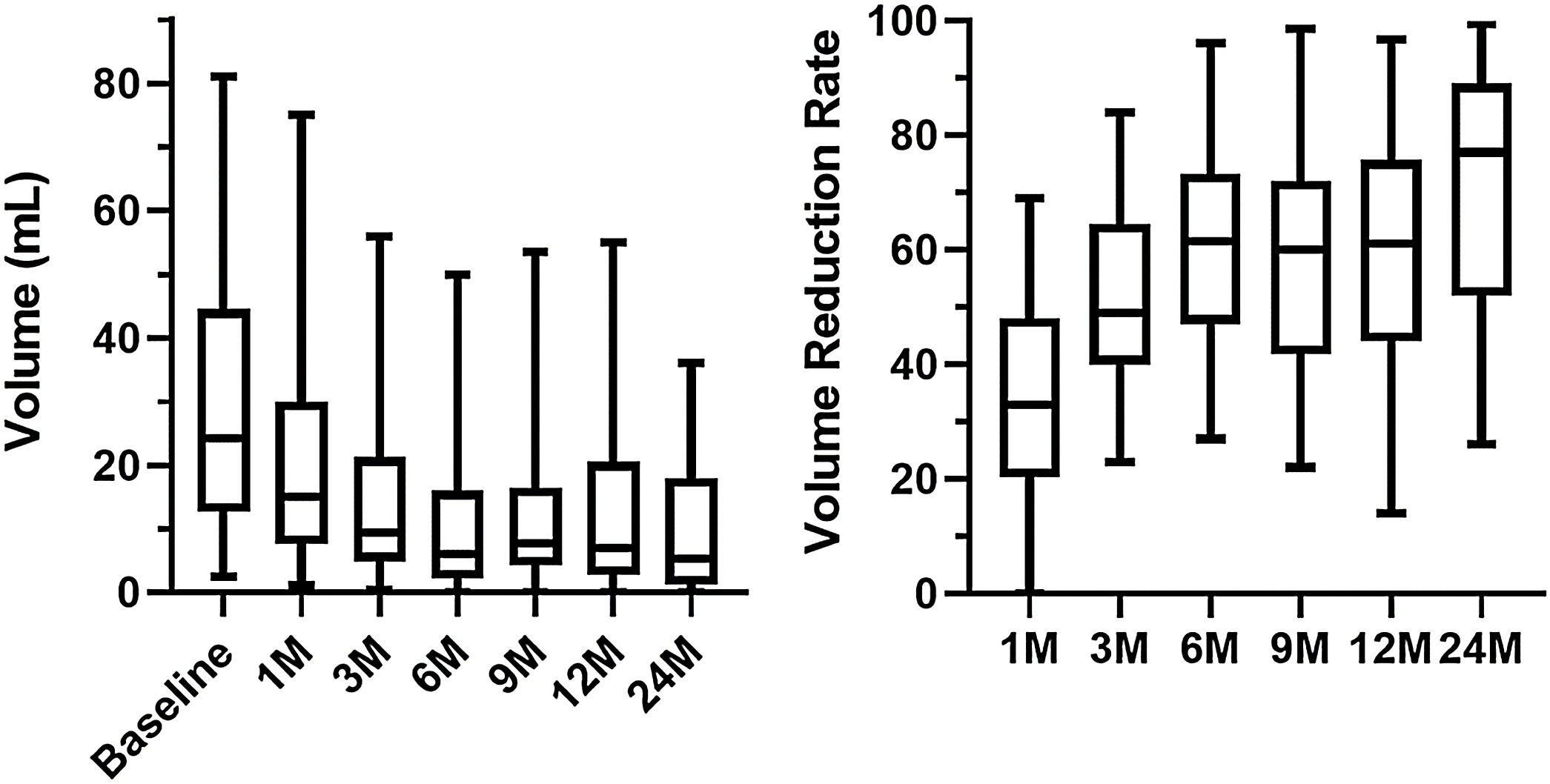
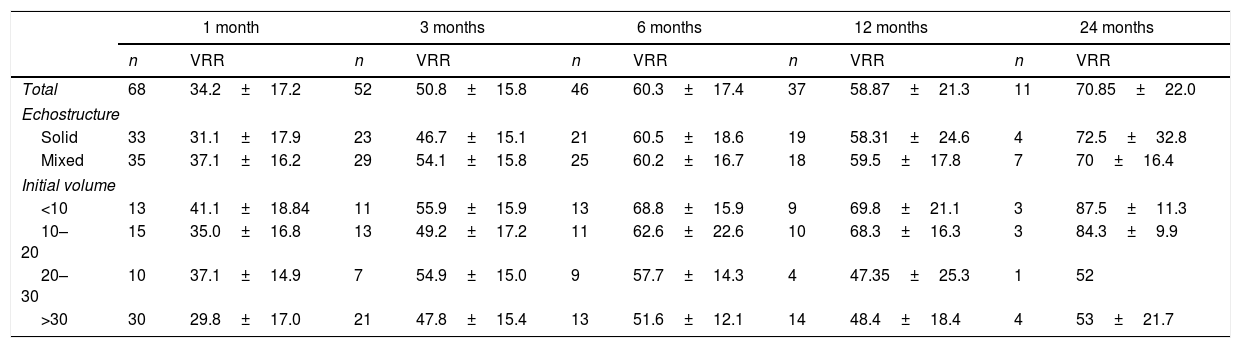
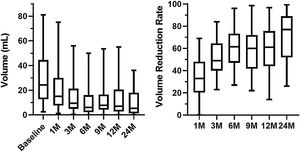
After RFA, nodule volume decreased progressively from 23.5ml, 2.5–81.0 (median, range) at baseline to 15.0ml, 1.2–75.0 one month after treatment, 9.5ml, 0.5–56.0 three months after treatment, 6.0ml, 0.1–50 six months after treatment, 7.0ml, 0.1–55.0 twelve months after treatment and 5.35ml, 0.1–36.0 twenty four months after treatment (p<0.0001 for all times vs. baseline). Expressed as VRR (mean±SD): 34%±17.2 one month after treatment, 50.8±15.8% three months after treatment, 60.3±17.4% six months after treatment, 58.87±21.3% twelve months after treatment and 70.85±22.0% (p<0.0001 for all times vs. baseline). These results are shown in Table 2 and Fig. 1. The percentage of nodules that achieved a volume decrease of at least 50% was 20.6%, 44.2%, 73.9%, 64.8% and 81.8% 1, 3, 6, 12 and 24 months after treatment, respectively. After 12 months, only 1 patient had experienced a subsequent regrowth of the nodule that generated a loss of 50% of the reduction initially achieved. Analysing those nodules with a follow-up of at least 12 months (n=41), initial volume was 17.2ml, 2.6–81.0, the final volume being 6.9ml, 0.1–55.0 (p≤0.001), with a VRR of 60.51%±21.08. Coefficient of variation of VRR in this group was 49.83%, 32.67%, 29.76% and 34.68% 1, 3, 6 and 12 months after treatment, respectively.
Volume Reduction Rate (VRR) for all nodules and relative to baseline characteristics. Data are mean±SD.
| 1 month | 3 months | 6 months | 12 months | 24 months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | VRR | n | VRR | n | VRR | n | VRR | n | VRR | |
| Total | 68 | 34.2±17.2 | 52 | 50.8±15.8 | 46 | 60.3±17.4 | 37 | 58.87±21.3 | 11 | 70.85±22.0 |
| Echostructure | ||||||||||
| Solid | 33 | 31.1±17.9 | 23 | 46.7±15.1 | 21 | 60.5±18.6 | 19 | 58.31±24.6 | 4 | 72.5±32.8 |
| Mixed | 35 | 37.1±16.2 | 29 | 54.1±15.8 | 25 | 60.2±16.7 | 18 | 59.5±17.8 | 7 | 70±16.4 |
| Initial volume | ||||||||||
| <10 | 13 | 41.1±18.84 | 11 | 55.9±15.9 | 13 | 68.8±15.9 | 9 | 69.8±21.1 | 3 | 87.5±11.3 |
| 10–20 | 15 | 35.0±16.8 | 13 | 49.2±17.2 | 11 | 62.6±22.6 | 10 | 68.3±16.3 | 3 | 84.3±9.9 |
| 20–30 | 10 | 37.1±14.9 | 7 | 54.9±15.0 | 9 | 57.7±14.3 | 4 | 47.35±25.3 | 1 | 52 |
| >30 | 30 | 29.8±17.0 | 21 | 47.8±15.4 | 13 | 51.6±12.1 | 14 | 48.4±18.4 | 4 | 53±21.7 |
A significant inverse correlation between basal thyroid nodule volume and percentage of volume reduction was found (p=0.0018). After 12 months, 88.8% of the nodules<10ml, 80% of the nodules sized 10–20ml, 50% of those sized 20–30ml and 42.9% of the nodules>30ml reached a decrease of 50% in size, with a coefficient of variation of 30.18%, 23.88%, 53.44% and 37.88%, respectively. No difference was found between mixed and solid nodules (p=0.8707) (see Table 2).
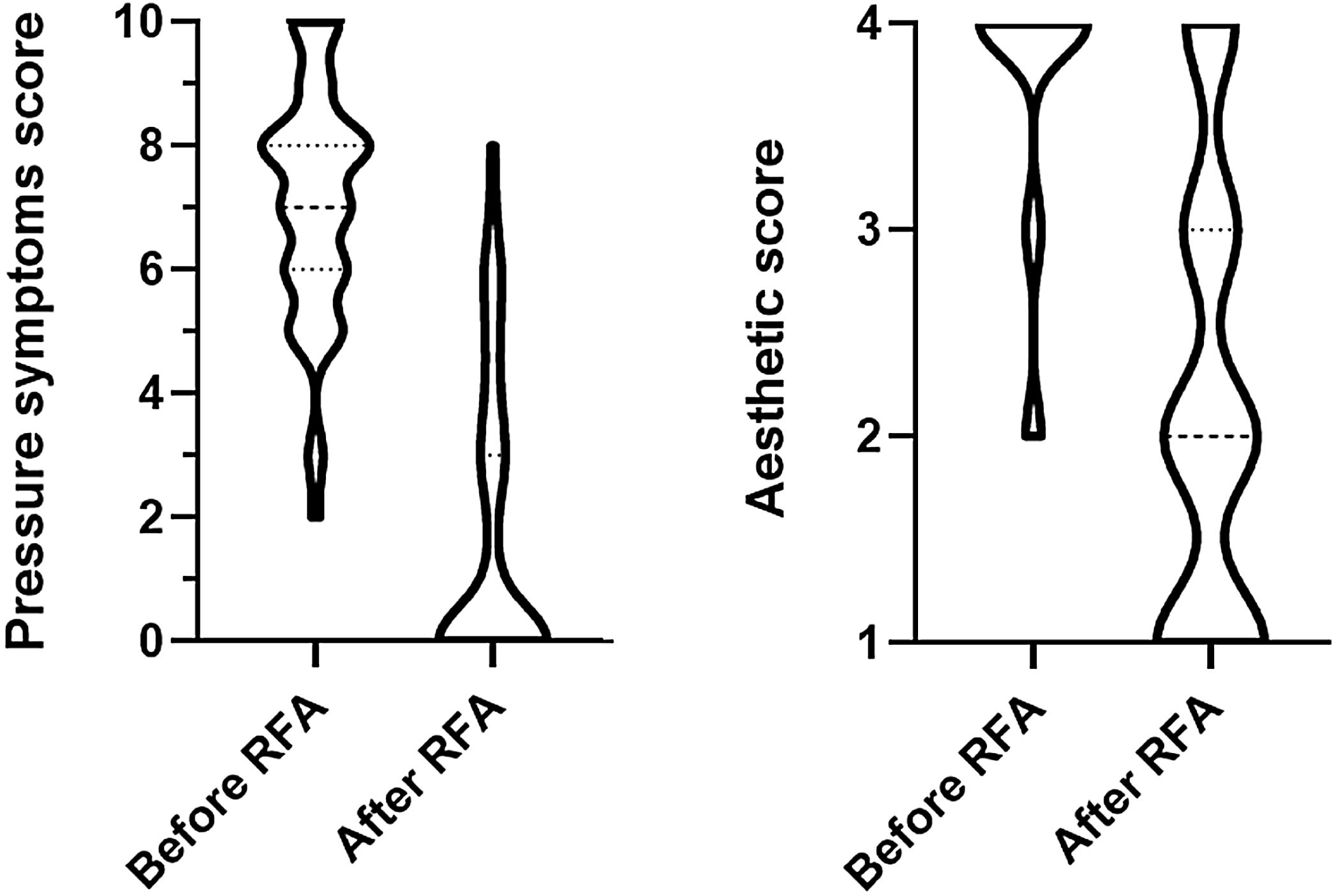
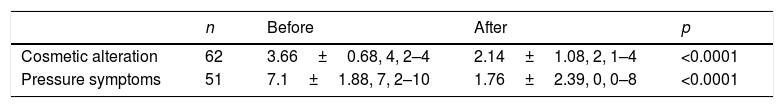
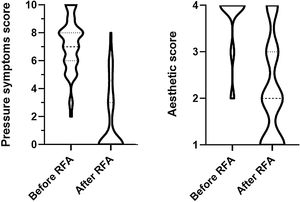
Prior to radiofrequency treatment, 62 patients had cosmetic alteration and 51 had pressure symptoms, mainly foreign body perception. Cosmetic alteration improved significantly from (mean±SD, median, range) 3.66±0.68, 4, 2–4 at baseline to 2.14±1.08, 2, 1–4 (p<0.0001). Pressure symptoms also improved significantly from 7.1±1.88, 7, 2–10 at baseline to 1.76±2.39, 0, 0–8 (p<0.0001). These results are shown in Table 3 and Fig. 2. No difference in symptomatic improvement was found in relation to basal nodule characteristics. Finally, 87.9% of patients felt symptom improvement.
Top. Comparison between cosmetic and compressive score (without unaffected patients) before and after treatment. Pressure symptoms were evaluated on a 0–10 scale and cosmetic alterations on a 4-point scale. Data are mean±SD, median, range. 13 of 62 patients with cosmetic alteration had no pressure symptoms. Bottom. Comparison between symptoms before and after treatment. Data are numbers of patients.
| n | Before | After | p | |
|---|---|---|---|---|
| Cosmetic alteration | 62 | 3.66±0.68, 4, 2–4 | 2.14±1.08, 2, 1–4 | <0.0001 |
| Pressure symptoms | 51 | 7.1±1.88, 7, 2–10 | 1.76±2.39, 0, 0–8 | <0.0001 |
| No. of patients | ||
|---|---|---|
| Foreign body | 51 | 20 |
| Dysphagia | 36 | 6 |
| Dyspnoea | 7 | 1 |
| Dysphonia | 9 | 2 |
| Others | 2 | 0 |
At the end of the follow-up period, 4 patients received an additional treatment for the same previously treated nodule: in 2 cases, a second RFA session, and in the other two, surgery was performed. 3 of these 4 nodules had decreased around 60% in size but patients still felt symptoms, and the other had decreased only 13%.
During radiofrequency treatment, 95.5% of patients felt no pain. Two patients felt mild pain, one moderate but no-one severe pain. All patients left hospital a few hours after the treatment. In the days following the procedure, 59% were completely asymptomatic. In the other group, 77% described their inconvenience as mild, 23% moderate and none as severe. Most of these patients described slight cervical pain, which was reported by almost all as transitory. Only one patient reported a persistent symptom: a slight decrease of his voice potency. No alterations of vocal cord mobility were found in the studies performed. During follow-up, 4 patients started taking medication due to thyroid function alteration (3 levothyroxine and 1 thiamazole). After excluding those patients that started taking medication, TSH was 2.31±1.55mU/L (mean±SD), exceeding the upper limit of normality in two cases after a mean follow-up of 9.4±6.8 months. TSH evaluation was performed at 8.63±5.14 months (minimum: 1, maximum: 20) after treatment.
In the satisfaction survey, 87.9% of patients reported being satisfied or very satisfied with the procedure (shown in Fig. 3) and 89.4% answered that they would choose the same treatment option again after the experience.
DiscussionMany reports have shown the efficacy of RFA in reducing the volume of benign thyroid nodules and in improving its cosmetic and/or compressive symptoms. The present study confirms and extends previous data.
Earlier studies reported 47.7–96.9% VRR after RFA.9,12–21 Our results (58%) are in line with these although far from those with higher VRR.17–19 We have seen that nodule reduction is statistically significant from the first month after treatment. Other studies with longer follow-up have shown reductions over long periods of time.16,17
Our results show that initial volume influences the efficacy of RFA; nodule volume reduction was greater on smaller nodules. Furthermore, the coefficient of variation is lower in smaller nodules. This difference in nodule volume reduction has been noted in other studies that reported similar results.16,17,24 The influence of echostructure is not statistically significant in our study; however, other studies have reported higher reductions in mixed nodules.16,17 Differences in volume reduction in relation to the characteristics of the nodules hardly imply changes in the use of RFA. In any case, reductions achieved in nodule size and symptomatic scores are beneficial.
Most of our patients reported a perception of improvement of their symptoms. Cosmetic and compressive scores both improved ameliorated after RFA in a statistically significant manner. This is an important benefit of RFA as its main reason to be used as treatment of benign nodules is to reduce their symptoms. RFA has shown efficacy to do this both in our study and in others.15,17,19
After RFA, a few patients received a second RFA or surgical intervention, which means that, for the great majority of patients, a single RFA would be enough to treat their thyroid nodules. As has been mentioned, this allows us to avoid all the possible surgical complications and reduces the cost of the treatment.
Intervention was painless for most of the patients, probably due to the use of conscious sedation, and those who felt some kind of discomfort in the days after the treatment described it as mild and transitory. Thyroid function was not affected in most of the cases. RFA has proved its safety as has been noted in the literature.15,18,22,23
We note a complication suffered by a 48 year-old female patient of our study after a second RFA on the same nodule (this complication is not included in the results as we have considered efficacy and safety of a solitary RFA). After the first RFA, the volume of the nodule, which was on the left side, was reduced only 13%, so a second RFA was performed. Two days after the second treatment, the patient reported left eye ptosis and miosis. She was diagnosed with Horner syndrome in relation to RFA treatment. This is a most extraordinary complication that could be explained by a lesion of the middle cervical sympathetic ganglion.23 The patient has improved slightly after 18 months, but the syndrome persists.
It should be noted that most patients expressed satisfaction with the procedure, and we understand that as a valuable marker of the efficacy of the technique.
A limitation of this study could be its retrospective nature. While it was being carried out, new patients were progressively included, which explains the fact that we present a smaller sample size for a longer follow-up period, which does not allow us to obtain conclusions of the evolution in the medium-long term. Furthermore, follow-up was heterogeneous due to the loss of some of the scheduled ultrasound examinations. Even though our sample size may be considered limited, we consider it is adequate for evaluating the efficacy and safety of the technique. Our results are also in line with those described in recent literature, making them more reliable. Another possible limitation is that the maximum power level applied during the procedure has not been considered. The strong points of our study would be that it collects data on both efficacy in volume and symptom reduction, considering our patients’ opinion about the procedure and their satisfaction with the results.
In conclusion, RFA is effective and safe in shrinking benign thyroid nodules as well as in reducing nodule-related symptoms. RFA can be an alternative to surgery in symptomatic benign mixed or solid thyroid nodules. What is more, as more evidence on its advantages and long-term results becomes available, this minimally invasive technique and/or others may be more readily considered also as a first line treatment option for the management of benign thyroid nodules in future guidelines.
Conflict of interestsThe authors declare that they have no conflict of interest.