To guide professionals involved in the care of people with diabetes mellitus who practice sport.
ParticipantsMembers of the Diabetes Mellitus Working Group of the Spanish Society of Endocrinology and Nutrition.
MethodsA group of experts in each area covered by the statement carried out a bibliographic review of the available evidence for each topic, based on which recommendations were subsequently agreed upon within the Diabetes Mellitus Working Group.
ConclusionsThe statement provides practical recommendations for the management of diabetes mellitus during sports practice.
Orientar a los profesionales involucrados en la asistencia de personas con diabetes mellitus que realizan deporte.
ParticipantesMiembros del Grupo de Trabajo de Diabetes Mellitus de la Sociedad Española de Endocrinología y Nutrición.
MétodosUn grupo de expertos en cada área del documento realizó una revisión bibliográfica de la evidencia disponible para cada tema, en base a las cuales se establecieron unas recomendaciones posteriormente consensuadas dentro del Grupo de Trabajo de Diabetes Mellitus.
ConclusionesEl documento aporta cuestiones prácticas para el manejo de la diabetes mellitus durante la práctica deportiva.
In 2015, the Grupo de Trabajo de Diabetes Mellitus (GTDM) [Diabetes Mellitus Working Group] of the Sociedad Española de Endocrinología y Nutrición (SEEN) [Spanish Society of Endocrinology and Nutrition] (GTDM-SEEN) prepared its "Clinical recommendations for the practice of sport by people with diabetes mellitus (RECORD Guide)",1 to offer guidance for professionals involved in the care of people with DM who do sport.
With the appearance of new drugs, continuous glucose monitoring (CGM) systems, and new publications in this field, these recommendations have been updated.
The complete document to which this executive summary corresponds can be consulted at:
MethodologyWithin the GTDM-SEEN, a group of experts was selected who carried out a bibliographic review of the available evidence for each topic with an inclusion date until 31 September 2020.
Given the practical absence of clinical studies related to most of the aspects reviewed, it was not possible to establish recommendations based on the level of evidence. Therefore, it was decided to formulate “expert recommendations” based on the available data discussed jointly by the Working Group and have subsequently been endorsed by the SEEN Board of Directors.
Effects on glycaemic control of different types of exerciseExercise increases muscle glucose uptake by improving insulin sensitivity (IS) in an insulin-independent manner. These effects differ according to the type of DM.2
The intensity of aerobic exercise is usually defined by the consumption of O2 by the muscles In practice, the percentage of maximum heart rate (MHR) can be used. The intensity is mild if the %MHR is <40-50%, moderate if it is 50–70% and high if it is >70−80%.
Recommendations 1- •
Diabetes mellitus type 2 (DM2)
- o
Both aerobic and resistance exercise improve IS and HbA1c. These benefits are enhanced by the combination of both, as well as by greater intensity and regularity in the practice of exercise.
- o
A training plan based on high intensity interval training (HIIT) achieves similar benefits with a significant reduction in the time invested.
- o
- •
Diabetes mellitus type 1 (DM1)
- o
The short-term effect on blood glucose depends mainly on insulin levels and the type of exercise.
- o
There is insufficient evidence to conclude that regular exercise consistently improves HbA1c levels in adults with DM1. Despite this, it should be recommended due to its other benefits on the cardiovascular system.
- o
In overweight or obese people, exercise guidelines based on HIIT improve HbA1c levels if adherence is adequate.
- o
People with DM should undergo an assessment before starting an exercise programme3 that will include the following points:
- •
Setting some goals:
- o
Finding out if the patient has any associated disease or complication.
- o
Planning and scheduling exercise.
- o
Preventing injuries.
- o
- •
Reviewing the diabetes care plan (glycaemic control, therapy, education, etc.).
- •
Pre-exercise medical examination.4
- •
Formulation of specific recommendations (Table 1).5
Table 1.Exercise and diabetes complications.
Complication Recommendations Contraindications Precautions Cardiovascular disease Low-impact aerobic activities: walking, cycling, swimming, treadmill. Recent AMI (<6 weeks). Hypertensive activities: lifting heavy weights, high-intensity workouts Increase heart rate gradually Autonomic neuropathy Low-intensity exercises that do not change blood pressure: aquatic activities, stationary cycling and sitting exercises High intensity. Sudden changes in body position. Test to check for coronary disease. Maintain BP to prevent orthostatism. Avoid exercising in very cold or very hot environments and maintain adequate hydration. Monitor blood glucose. Peripheral neuropathy Swimming, cycling, chair exercises, arm exercises and exercises that do not require the use of the feet. Very demanding long walks, running, and any activity that involves jumping. Do not exercise if with ulcers or active Charcot foot. Pre-exercise evaluation of sensitivity. Suitable footwear. Daily hygiene check of the feet. Diabetic retinopathy Low-intensity aerobic exercises: stationary bike, walking, swimming, treadmill Do not perform physical activity in the presence of active PDR (vitreous haemorrhage, vitreomacular traction) and after recent photocoagulation or surgery. Avoid exercises that increase BP abruptly (violent physical activities, Valsalva, weights), those that involve sudden movements or lowering the head (gymnastics, yoga) and contact sports (boxing, martial arts, etc.) Gradual increase in intensity. Avoid allowing systolic BP to reach >170mmHg during exercise. Diabetic nephropathy Low-intensity aerobic activities Avoid exercises that increase BP abruptly: violent physical activities, Valsalva manoeuvre, lifting weights. Pay particular attention to hydration and BP control. AMI: acute myocardial infarction; BP: blood pressure; PDR: proliferative diabetic retinopathy.
- •
Special examinations (stress test, spirometry, ECG).
- •
Assessment of sport habit (SH) and risk of hypoglycaemia.
People with DM who do sport should be classified according to SH in6:
- •
intense SH: >2 weekly exercise sessions lasting ≥45min.
- •
Moderate SH: 1−2 weekly exercise sessions lasting ≥45min.
- •
Low SH: does not exercise regularly.
They should also be classified according to their risk of hypoglycaemia when interstitial glucose monitoring (IGM) is available, according to time below range (TBR) less than 70mg/dl, in:
- •
Low risk of hypoglycaemia: preserved recognition of hypoglycaemia and TBR<4% in the last three months
- •
Moderate risk of hypoglycaemia: conserved recognition of hypoglycaemia and TBR 4–8% in the last three months.
- •
High risk of hypoglycaemia: inadvertent hypoglycaemia or severe hypoglycaemia in the last six months and/or TBR>8% in the last three months.
- •
People with DM with possible cardiovascular (CV) disease or microvascular complications who wish to engage in more vigorous exercise than brisk walking should undergo a medical evaluation that will include medical history, a physical examination (including fundus examination, foot examination and neuropathy test), resting ECG and possibly a stress test.
- •
The stress test should be performed in all patients at high CV risk.
- •
A stress test is useful in multiple ways:
- o
For exercise prescription.
- o
For risk stratification.
- o
For detecting silent coronary disease.
- o
For detecting abnormal hypertensive responses.
- o
- •
It is recommended to classify people according to their SH and risk of hypoglycaemia.
The recommended balance of macronutrients is 45–65% carbohydrates (CH), 20–35% fats and 10–35% proteins2, although it should be personalised. Ensure the intake of B vitamins, iron, calcium and vitamin D. They should only be supplemented if there are deficits in the diet or if they are found to be lacking.7
Before, during and after exercise, adjustments will be made according to Table 2. In prolonged exercise or recovery, slowly absorbed CH (sCH) reduces the risk of hypoglycaemia and avoids hyperglycaemic peaks.
CH supplementation before, during and after practising sport for people with DM1 with glucose monitoring.
| SH type and/or hypoglycaemia risk | Trend arrow | Action | ||||
|---|---|---|---|---|---|---|
| Pre-exercise | Intense SH and/or low risk of hypoglycaemia | Moderate SH and/or moderate risk of hypoglycaemiaa | Low SH and/or high risk of hypoglycaemiab | Direction | Rise in blood glucose expected | Fall in blood glucose expected |
| 126−180mg/dl | 145−198mg/dl | 162−216mg/d | ↗↑ | Start exercise | ||
| → | ||||||
| ↘↓ | Start exercise | Start exercise +15g GL | ||||
| 90−125mg/dl | 90−144mg/dl | 90−161mg/dl | ↗↑ | Start exercise | Start exercise +15g GL | |
| → | Start exercise +10g GL | Start exercise +20g GL | ||||
| ↘ | Delay exercisec +15g GL | Delay exercisec +25g GL | ||||
| ↓ | Delay exercisec +20g GL | Delay exercisec +30g GL | ||||
| 70−89mg/dl | ↑ | Start exercise +10g GL | Delay exercisec +20g GL | |||
| ↗ | Delay exercised +15g GL | Delay exercisec +25g GL | ||||
| → | Delay exercised +20g GL | Delay exercisec +30g GL | ||||
| ↘ | Delay exercised +25g GL | Delay exercisec +35g GL | ||||
| ↓ | Delay exercised + personalised GL | Delay exercisec + personalised GL | ||||
| <70mg/dl | Delay exercisee + personalised GL | |||||
| Exercise | <126mg/dl | <145mg/d | <162mg/dl | ↗↑ | Continue exercise | |
| → | Continue exerciseh +10g GL | Continue exerciseh +15g GL | ||||
| ↘ | Continue exerciseh +15g GL | Continue exerciseh +25g GL | ||||
| ↓ | Continue exerciseh +20g GL | Continue exerciseh +35g GL | ||||
| <70mg/dl | Any trend | Personalised GL replenishment | ||||
| Post exercise | <80mg/dl | <90mg/dl | <100mg/dl | ↗↑ | No | |
| → | +10g GL | |||||
| ↘ | +15g GL | |||||
| ↓ | Individualised intake | |||||
GL: rapidly absorbed glucose/carbohydrates; CH: carbohydrates; SH: sport habit.
fIncludes older people with functional status and preserved higher functions.
gIncludes older people with impairment of ≥2 instrumental activities of daily living or mild-moderate cognitive impairment.
iCheck blood glucose at 30min, repeat GL administration if necessary.
Includes older people with impairment of ≥2 instrumental activities of daily living or mild-moderate cognitive impairment.
In exercise longer than one hour, isotonic drinks can prevent hypoglycaemia and contribute to ion replenishment; soft drinks and energy drinks should be avoided. Milk drinks are useful for recovery and prevention of late hypoglycaemia.8
After finishing exercise, if blood glucose is less than 120mg/dl, without IGM data, it is advisable to ingest 15−20g sCH, both in DM1 and DM2 treated with insulin or secretagogues.
Competitive athletes should ensure glycogen replenishment by taking 1–1.5g/kg CH in the first two hours after exercise. Hyperglycaemia associated with explosive exercises should be monitored. If post-exercise CH intake is insufficient, taking them with protein may be beneficial. After strenuous or prolonged exercise, a night-time snack with fat, CG and protein can prevent nocturnal hypoglycaemia.
Recommendations 3- •
There is no ideal recommendation for macronutrients. The recommended macronutrient balance is 45–65% CH, 20–35% fats and 10–35% proteins.
- •
Before exercise, capillary blood glucose should be checked. If it is less than 100mg/dl (without IGM data), a CH supplement should be taken if receiving treatment with insulin or secretagogues.
- •
An adequate state of hydration should be maintained during exercise. If exercise lasts more than one hour, between 30−60g of CH per hour should be ingested.
- •
After exercise, CH replenishment should be ensured, preferably with those with a low glycaemic index.
The EASD-ISPAD-ADA position on the use of CGM and flash glucose monitoring during exercise6 suggests doing the following when taking exercise:
- •
Pre-exercise preparation:
- o
Set the hypoglycaemia alarm at the highest level allowed during peak exercise and the hyperglycaemia alarm above 180 md/dl to avoid alarm fatigue.
- o
- •
During exercise:
- o
Maintain a time in the range of 90−180mg/dl (126−180mg/dl in the case of prolonged aerobic exercise).
- o
- •
After exercise:
- o
Time in range of 80−180mg/dl for the first 90min after performing the exercise.
- o
Perform CGM every 15−30min after doing exercise for the first 90min after finishing.
- o
Modify the hypoglycaemia alarm based on the risk of mild, moderate or severe hypoglycaemia.
- o
- •
CGM and lash glucose monitoring devices constitute therapeutic support when exercising.
- •
It is recommended to analyse sensor data during physical activity and retrospectively to:
- o
Modify the insulin dose.
- o
Adapt the intake of CH.
- o
Minimise late hypoglycaemia.
- o
- •
If hypoglycaemia in interstitial blood is detected during exercise, testing with capillary blood is recommended.
- •
The manufacturer's recommendations for use should be followed.
- •
There are no conclusive data regarding altitude, depth or contact sports, although it seems that they could be useful in types of exercise such as diving and high-altitude sports.
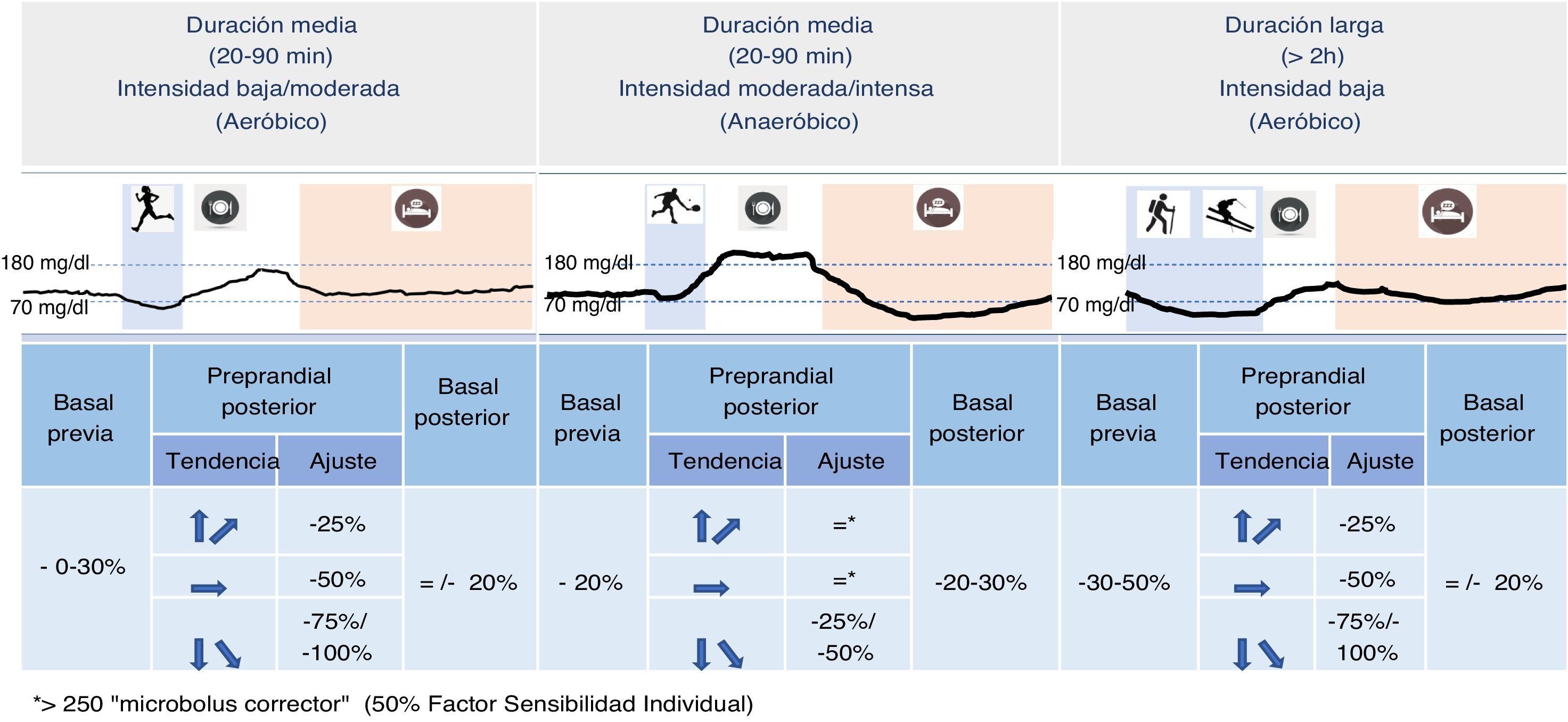
The intensity, duration and type of exercise, and the corresponding individual metabolic response to it, must be predetermined to consider specific adjustments of the insulin dose.2 The increasingly widespread use of CGM makes it possible to take into account the current glucose levels and the prediction of their trend in the following hours when making these decisions (Fig. 1).
- •
Reduce basal (except degludec)/intermediate insulin before that day by at least 20% (glycaemic target: 126−160mg/dl, depending on risk).
- o
If exercise is done on an empty stomach or post-absorptive period (>3h after ingestion), consider making greater reductions.
- o
- •
Adjust rapid-acting insulin.
- o
Preprandial insulin before exercise (1−3h before): reduce by at least 25% for the exercise of short duration (<1/2h), 50% for the medium duration (<1h), and 75% for prolonged exercise (>1h).
- o
Preprandial insulin before exercise (1−3h after): consider a reduction of at least 25% for the exercise of short duration (<1/2h), 50% for the medium duration (<1h) and 75% for prolonged exercise (>1h).
- o
For corrective boluses for hyperglycaemia peaks: only in cases of clearly high blood glucose levels (>250mg/dl) consider adding a “corrector micro-bolus” (50% of the individual correction factor).5
- o
- •
Reduce basal (except degludec)/intermediate post-exercise insulin by 20−30%
- •
Rapid-acting insulin.
- o
Preprandial insulin before exercise (between 1 and 3h before) and preprandial insulin after exercise (1–3h after): do not reduce.
- o
For correction boluses for hyperglycaemia peaks (generally of short duration): only in clearly elevated blood glucose levels (>250mg/dl) consider adding a “correction micro-bolus” (50% of the individual correction factor).3
- o
In general, it is not necessary to modify the regimen of non-insulin drugs for sporadic exercise, but secretagogue drugs and SGLT2 inhibitors should be reduced or discontinued when intense and long-lasting exercise is performed.
Recommendations 6- •
Hypoglycaemia is the most common metabolic complication in patients with diabetes who perform physical exercise, although, in the absence of insulin treatment, it appears infrequently.
- •
The non-insulin drugs with the greatest risk of hypoglycaemia are those that increase endogenous insulin secretion (sulfonylureas and glinides), although the overall risk is usually low.
- •
Although SGLT2 inhibitors do not cause hypoglycaemia, they predispose to a higher risk of dehydration, hypotension and ketosis/ketoacidosis.
- •
Before intense and long-lasting exercise (>60min), it is recommended to reduce the usual dose or suspend the administration of both sulfonylureas/glinides and SGLT2 inhibitors.
The following considerations should be taken into account:
- •
Choose the place of insertion of the catheter avoiding areas where it can receive blows or cause rubbing or friction.
- •
In general, it is not recommended to turn off the CSII, but it may be necessary for some sports (aquatic, contact, etc).
- •
In the event of disconnection (try not to exceed 1−2h), previously administer a bolus equivalent to the basal rate (BR) x 1.25, applying a reduction of 20–50%. In disconnections >3−4h, administer the calculated dose by injecting a short- or intermediate-acting insulin (regular, NPH or detemir) 30−60min before disconnection, applying the same reduction percentage. When reconnecting, a correction bolus ≈50% of the calculated dose may be required to avoid subsequent hyperglycaemia.
- •
In high-risk or high-intensity sports, it is recommended to increase the predictive stop threshold of CSII+CGM (80mg/dl) and keep it until 90min after completion of the activity.
- •
For BR and bolus adjustments, see Tables 3 and 4.2
Table 3.Recommended basal rate adjustments and CH supplements in CSII or CSII/CGM users before planned and unplanned exercise.
Planned exercise CBG/IG 60−90min pre-exercise BR reduction (temporary) 60−90min before exercise CBG/IG at start of exercise CH intake at start of exercise <70mg/dl 50% <70mg/dl 10−20g without bolus 70−150mg/dl 30−50% 70−150mg/dl 10−20g and half calculated bolus >150mg/dl 20−30% >150mg/dl Not necessary Unplanned exercise CBG/GI pre-exercise BR reduction (temporary) CBG/IG at start of exercise CH intake at start of exercise <70mg/dl 70−80% <70mg/dl 20g without bolus 70−150mg/dl 50% 70−150mg/dl 10−20g without bolus >150mg/dl 30% >150mg/dl Not necessary CBG: capillary blood glucose; IG: interstitial glucose; CH: carbohydrates; CSII: continuous subcutaneous insulin infusion; CGM: continuous glucose monitoring; BR: basal rate.
Table 4.Recommended prandial bolus settings in CSII or CSII/CGM users before planned exercise within 2–3h.
Type of planned exercise 2−3hours after prandial bolus Low-moderate intensity aerobic exercise Low-moderate intensity anaerobic exercise Intense anaerobic exercise Reduce 25% if low intensity May not require adjustment; evaluate Does not require adjustment −25% to −50% depending on glucose change expected from previous experiences Reduce from 50% to -75% if moderate intensity Consider adding small correction if CBG/IG elevated CBG: capillary blood glucose; IG: interstitial glucose; CSII: continuous subcutaneous insulin infusion; CGM: continuous glucose monitoring.
- •
In planned exercise, use a temporary BR with a reduction percentage before starting the exercise. If the activity is going to be carried out in 2−3h following the administration of a bolus, it is advisable to reduce the bolus.
- •
Use a temporary BR with a reduction percentage in unplanned exercise and take a CH supplement.
- •
After finishing the exercise, the temporary BR can be cancelled when the value of capillary blood glucose (CBG) or interstitial glucose (IG) is >100−120mg/dl. In some sports, it may be necessary to disconnect from the CSII.
- •
In high-intensity exercise, a correction bolus may be required when reconnecting.
- •
If a CGM system is used, frequently check the IG value and trend.
- •
With the CSII+CGM integrated system with predictive stop, it is recommended to raise the stop threshold when doing high-intensity exercise. With the hybrid closed-loop system, it is recommended to use the safe BR.
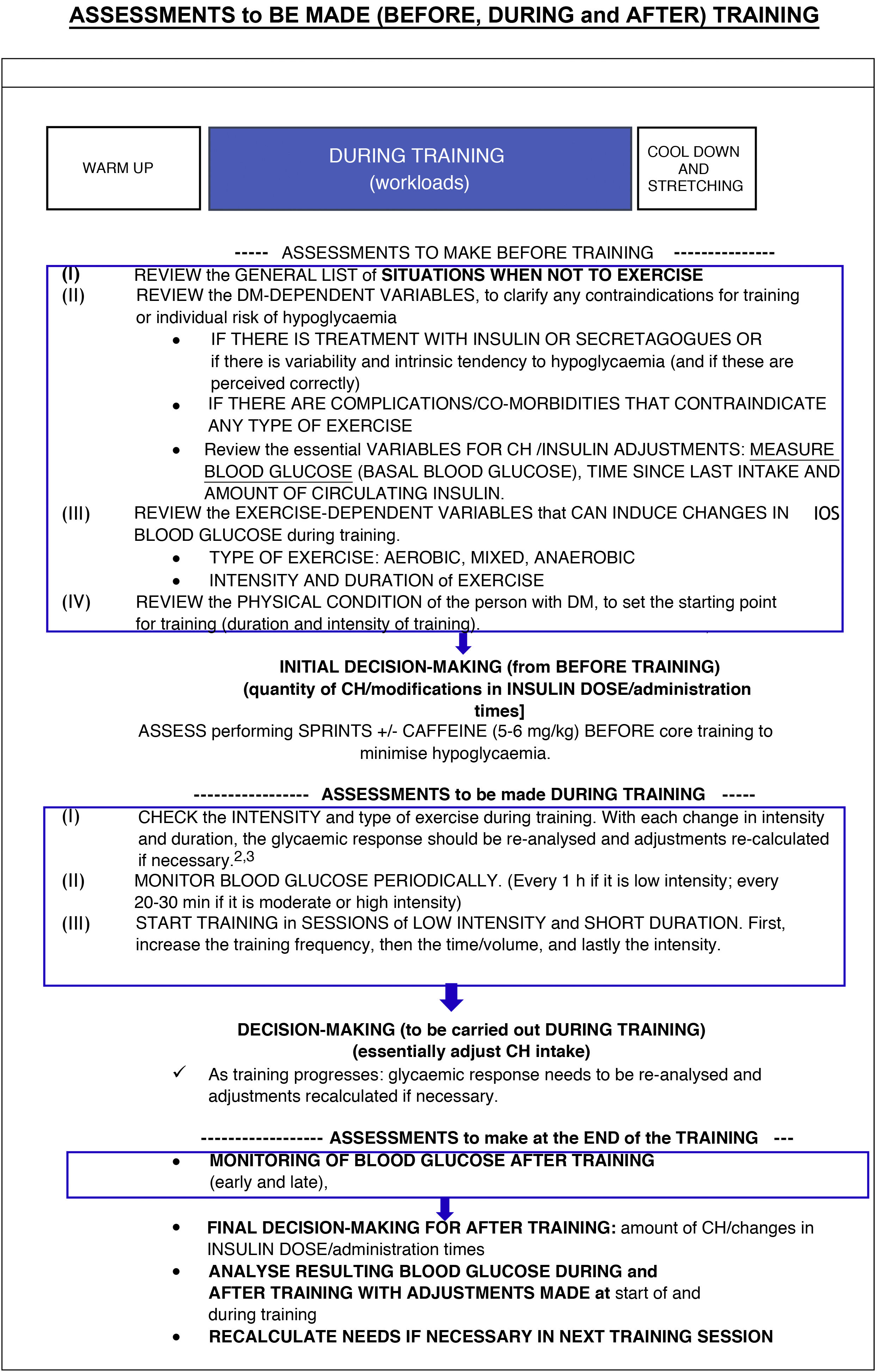
Training for people with DM has dual aspects which must go in parallel: on the one hand, the physical training incorporates and increases physical fitness, and on the other, the training is supported by structured diabetes education to minimise the risk of dysglycaemia.
It is a planned and complex process that organises progressive and increasing workloads that stimulate the development of different physical capacities. The glycaemic response to exercise depends on variables related to DM and factors related to exercise and has a marked individual response.2,8 The recommended adjustment ranges are also very wide.
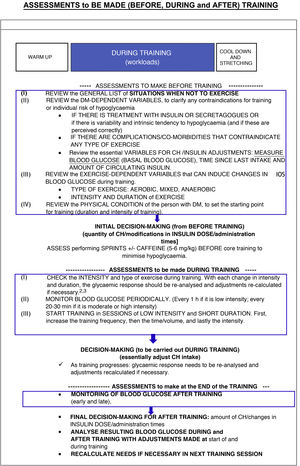
Table 5 shows the recommendations to be followed before, during and after training.
Recommendations 8- •
Before, during and after training, a series of assessments should be made to make adjustments (Table 5).
- •
Training should be started in low-intensity and short-duration sessions and then progress gradually.
- •
Training that combines aerobic and strength exercises should be carried out every other day.
- •
Whenever possible, they should be accompanied (but not replaced) by flexibility exercises. In older adults with DM, combine flexibility and balance training 2−3 times a week.
- •
Whenever possible, increase unstructured physical activity between workouts, as it provides extra benefits in terms of health.5
The special characteristics of each sport can influence the practical management of people with DM.
Diving can be practised safely by patients with DM as long as a series of conditions are followed, and various guides deal with this aspect.9 Cases have been published on the effective use of IGM during repetitive dives. To prevent decompression sickness, good hydration is very important, and it would be advisable for subjects with DM to readjust their dive computers to more conservative safety limits.
There are no data that contraindicate mountaineering for people with well-controlled DM. Some aspects should be taken into account:
- •
Glycaemic control: insulin needs and blood glucose levels increase (possibly due to the effect of counterregulatory hormones), so reducing the dose of insulin or oral drugs is not recommended.
- •
Retinopathy: can worsen at altitude.
- •
Thyroid function: there is a greater demand for thyroid activity at altitude, so prior thyroid dysfunction must be ruled out and treated if present (even subclinical).
- •
IGM: can be reliable up to an altitude of 3600m.
- •
Practical aspects. Insulin should be prevented from freezing by storing it in bags attached to the body. Use nasal glucagon (it does not freeze and is properly stored at temperatures up to 30°).
- •
Divers: start with a blood glucose level >180mg/dl. With any suspicious sign of hypoglycaemia: alert your diving partner and abort the dive. Dive only within the recommended safety margins for patients with DM. Dive with a partner who is informed and trained in managing hypoglycaemia.
- •
Mountaineers: do not reduce the dose of drugs; keep well hydrated; protect against the cold, especially the feet; and check blood glucose frequently. Keep insulin and glucagon from freezing. No increased risk of altitude sickness. Acetazolamide not recommended in DM1.
- •
Long-distance runners: preventive reduction of hypoglycaemic doses. Adequate hydration. Supplements and self-monitoring (or IGM) schedules. Prevent heat stroke.
- •
Navigators: do not go sailing alone. Supplements and self-monitoring (or MIG) every hour.
- •
Swimmers: start with a blood glucose level >180mg/dl. If hypoglycaemia is suspected, stop exercising, take supplements (carry gels in your swimsuit) and get out of the water.
Tables 6 and 7 provide recommendations for treatment with insulin and CH before and during exercise in children and adolescents with DM1 adapted to the ESAD, ISADP and ADA recommendations.6
Recommendations for treatment with insulin and carbohydrates for exercise in children and adolescents with DM1.
| Treatment | Type/intensity of exercise | Type/intensity of exercise |
|---|---|---|
| Duration up to 30−45min | Duration >45min | |
| MDI/CSII: | −25% light exercise | −50% light exercise |
| Preprandial bolus | −50% moderate exercise | −75% moderate exercise |
| −50% intense aerobic exercise | −75% intense aerobic exercise | |
| −25% mixed aerobic/anaerobic exercise | −50% mixed aerobic/anaerobic exercise | |
| Up to −50% post-exercise | Up to −50% post-exercise | |
| MDI | −20% in afternoon/evening exercise | −20% in afternoon/evening exercise |
| Basal insulina | −30−50% unusual activitya | |
| CSII | Up to −50% 90min pre-exercise | Up to −80% 90min pre-exercise |
| Pump suspension (<60min) | Pump suspension (<60min) | |
| −20% overnight post-exerciseb | −20% overnight post-exerciseb | |
| CH intakec | −10−15g CH | |
| −1.5g CH/kg weight/hour in intense exercise | ||
| −0.4g CH/kg weight before bed if evening exercise |
CH: carbohydrates; CSII: continuous subcutaneous insulin infusion; MDI: multiple doses of insulin.
Adapted from Moser et al.6.
Actions to adopt according to IGM data in different groups of children and adolescents with DM1.
| SH type and/or risk of hypoglycaemia | Trend arrow | Action | ||||
|---|---|---|---|---|---|---|
| Pre-exercise | Intense SH and/or low-risk hypoglycaemia | Moderate SH and/or moderate risk of hypoglycaemia | Low SH and/or high risk of hypoglycaemia | Direction | Rise in blood glucose expected | Fall in blood glucose expected |
| >270mg/dl and ketonemia >1.5mmol/l | Any | No exerciseCorrection with insulina | ||||
| >270mg/dl and ketonemia <1.5mmol/l | Any | Consider correction insulinaCan do mild/mod activity | Consider correction insulinaCan do any PA | |||
| 180−270mg/dl | 199−270mg/dl | 217−270mg/dl | ↗↑ | Mild/mod activity | Any PA | |
| →↘↓ | Any PA | |||||
| 126−180mg/dl | 145−198mg/dl | 162−216mg/d | →↗↑ | Any PA | ||
| ↘↓ | 5g CHAny PA | 10g CHAny PA | ||||
| ↑↗ | Any PA | 5g CHAny PA | ||||
| 90−125mg/dl | 90−144mg/dl | 90−161mg/dl | → | 5g CHAny PA | 10g CHAny PA | |
| ↘ | 10g CHDelay PAb | 15g CHDelay PAb | ||||
| ↓ | Individual CH amountDelay PAb | |||||
| <90mg/dl | Individual CH amountDelay PAb | |||||
| During exercise | >270mg/dl and ketonemia >1.5mmol/l | Any | Stop exerciseConsider correction insulinaDo not restart exercise | |||
| ↗↑ | Consider correction insulincContinue PA | Continue any PAConsider mild/mod activity | ||||
| >270mg/dl and ketonemia <1.5mmol/l | → | Consider correction insulincContinue PA | Continue any PA | |||
| ↘↓ | Continue any PA | |||||
| 181−270mg/dl | 199−270mg/dl | 217−270mg/dl | ↗↑→ | Continue any PAConsider correction insulinc | Continue any PA | |
| ↘↓ | Continue any PA | |||||
| 126−180mg/dl | 145−198mg/dl | 162−216mg/d | Any | Continue any PA | ||
| <126mg/dl | <145mg/dl | <162mg/dl | ↗↑ | Continue any PA | ||
| → | 5g CHContinue any PAd | 10g CHContinue any PAd | ||||
| ↘ | 10g CHContinue PAd | 15g CHContinue PAd | ||||
| ↓ | 15g CHContinue PAd | 20g CHContinue PAd | ||||
| <70mg/dl | Stop any PAConsider confirming capillary blood glucosecIndividualised intake of CHRestart any possible PAe,f | |||||
| <54mg/dl | Stop any PAConfirm capillary blood glucoseIndividualised intake of CHDo not restart exercise | |||||
PA: physical activity; CH: carbohydrates; SH: sport habit.
Adapted from Moser et al.6.
After finishing exercise (90min post-exercise), the recommended glucose range is 80−180mg/dl or higher, depending on the risk of hypoglycaemia. If sensor glucose levels rise rapidly, a correction bolus of insulin (50% of the usual correction dose) may be considered, except around bedtime, to avoid post-exercise nocturnal hypoglycaemia. In the case of glucose <80mg/dl in children and adolescents at high risk of hypoglycaemia, CH will be ingested and consumption will be repeated until glucose levels are restored.
Recommendations 10- •
The insulin dose should be adapted to the intensity and duration of the exercise.
- •
It is preferable to adapt the intake of carbohydrates to the weight of the adolescent/child.
- •
It is recommended to set hypo/hyperglycaemia alerts in ranges of 100−180mg/dl or to do it individually and favour remote monitoring (for example, mobile applications that allow remote monitoring of the blood glucose sensor in real-time).