In 2001, a new subtype of autoimmune pancreatitis was reported and recognised as IgG4-related disease (IgG4-RD).1 It was characterised by the formation of lesions/masses due to diffuse lymphoplasmacytic infiltration of IgG4-positive cells, tissue sclerosing fibrosis, hypergammaglobulinaemia with a predominant increase in serum IgG4 levels and dysfunction of the compromised organ.2 The list of compromised organs rapidly expanded, with involvement of the salivary glands, bile ducts, orbit, lymph nodes, retroperitoneal tissue, etc.
Moreover, thyroid involvement or IgG4-related thyroid disease (IgG4-RTD) was first described by Li et al.3 in 2009, manifesting as a single entity or as a part of multisystem involvement in IgG4-RD. We report the case of a patient with IgG4-RTD mimicking thyroid lymphoma.
The patient was a 47-year-old Caucasian man, with no history of thyroid disease or cervical radiation, who consulted for a four-month history of non-painful, rapidly growing anterior cervical tumour associated with progressive dysphonia, dysphagia and dyspnoea. Physical examination revealed grade III goitre without palpable nodules. An initial neck ultrasound showed a markedly enlarged thyroid gland with hypoechoic areas and thin hyperechoic septa featuring increased vascularisation on colour Doppler imaging, suggestive of thyroiditis. Laboratory results were consistent with overt primary hypothyroidism of autoimmune origin (thyroid-stimulating hormone [TSH] 100.9μIU/ml [normal range (NR) 0.55–4.78], free thyroxine [T4] 0.38ng/dl [NR 0.89–1.76] and peroxidase antibodies 443,012 IU/ml [NR<60]), so treatment with levothyroxine was started. One month after the onset of signs and symptoms, the patient presented with right thyroid lobe (RTL) enlargement spreading to the ipsilateral submandibular region. Computed tomography (CT) of the neck showed a large goitre affecting the RTL (4cm×4.6cm×12cm [AP×T×L]; left thyroid lobe [LTL] 4.3cm×4cm×4cm), with spread towards the retropharyngeal space compressing the larynx and the ipsilateral pyriform sinus, associated with displacement of the glottal and supraglottal portion, including the vocal cords. Due to the mass’s rapid growth, fine needle aspiration biopsy was performed, yielding results consistent with Hashimoto’s thyroiditis. However, given that thyroid lymphoma was suspected, a decision was made to perform open glandular biopsy, which revealed a pattern of thyroiditis, inflammatory myofibroblastic tumour or IgG4-related sclerosing disease.
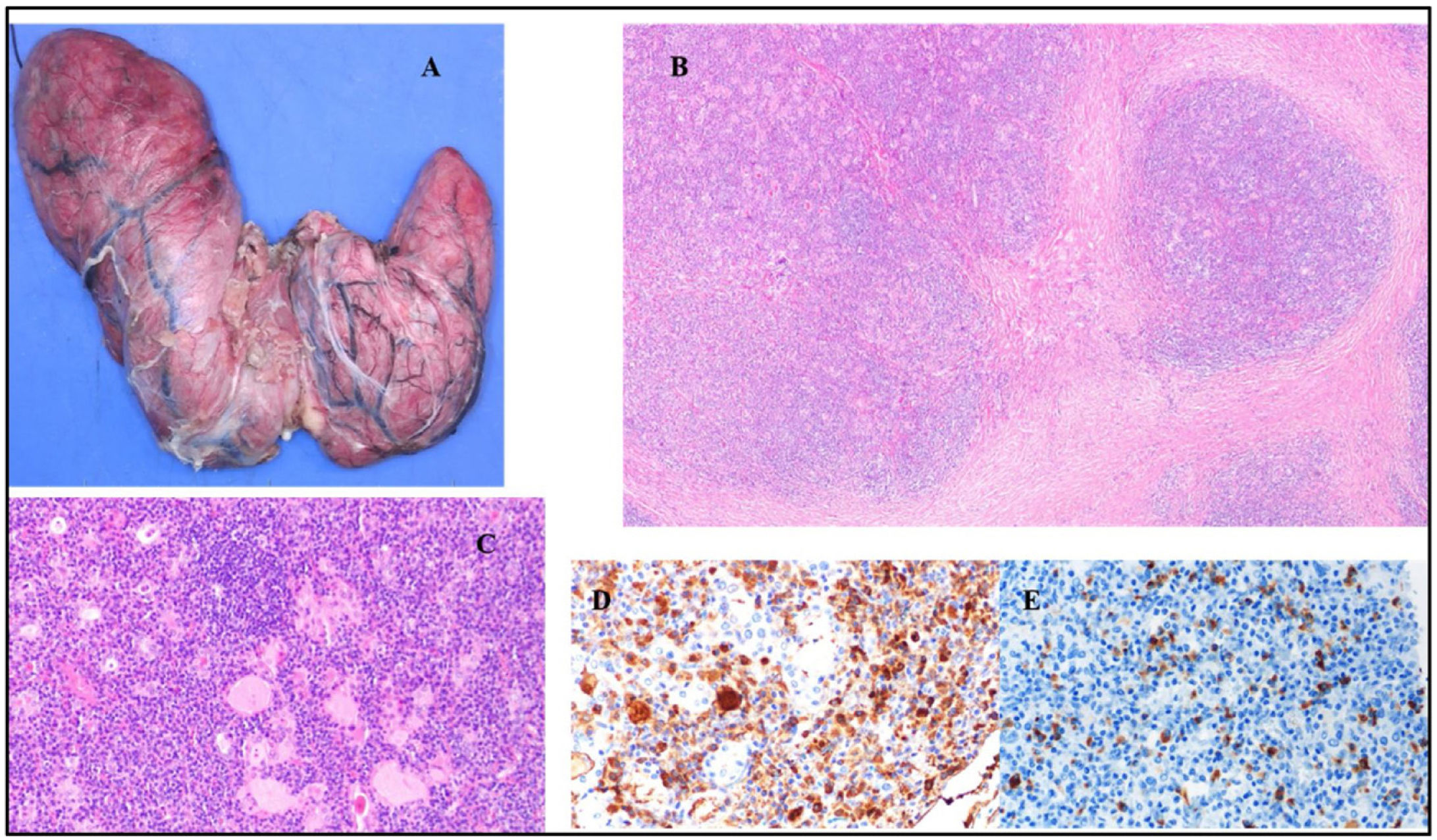
The case was presented to the Endocrine Tumours Committee. It was decided to order IgG4 521mg/dl (NR 3–200), beta-2 microglobulin 2.6mg/l (NR 1.1–2.5) and lactate dehydrogenase (LDH) 247 IU/l (NR 100–190) plus a positron emission tomography/computed tomography (PET/CT) scan with 18F-fluorodeoxyglucose (18F-FDG), which corroborated the presence of a large goitre with diffuse uptake in relation to lymphocytic thyroiditis. In light of the rapid growth and the compressive symptoms reported, it was decided to perform a total thyroidectomy. The only post-operative complication was a seroma that required drainage on two occasions. Pathology showed a thyroid gland weighing 182g (NR 25–30g) with IgG4-related fibrous variant of Hashimoto’s thyroiditis (with IgG4 staining >28 plasma cells per high-power field and IgG4/IgG ratio <30%, without observing areas of diffuse lymphoid proliferation through antigen receptor rearrangement analysis) (Fig. 1). IgG4 values decreased by 55% (290mg/dl) two weeks after the operation and normalised two months later. Two years after surgery, the patient has not presented with compromise of other organs or systems and maintains normal IgG4 serum levels.
Macroscopic and histological imaging of total thyroidectomy specimen. (A) Macroscopic image of thyroid gland, anterior face, weighing 182g. (B) Histological image of pseudonodular areas due to fibrosis (haematoxylin and eosin, 40×). (C) Immunohistochemistry image with IgG (400×). (D) Immunohistochemistry image with IgG4 (400×).
Our case represents a clear example of IgG4-RTD, a recently recognised benign thyroid disease that may mimic a neoplastic condition. The link between thyroid compromise and IgG4-RD was initially suggested based on the observation that hypothyroidism was highly prevalent in patients with autoimmune pancreatitis.1 Taking these observations as a starting point, Li et al.3 found that patients with Hashimoto’s thyroiditis could be subcategorised as patients with IgG4 (+) or IgG4 (–) infiltrates, with the former characterised by fibrosis and lymphoplasmacytic infiltration and the apparent absence of systemic extrathyroid involvement. Typically, patients with IgG4-RTD had higher rates of hypothyroidism, had high levels of thyroid peroxidase (TPO) antibodies, were younger, were mostly male and had disease with a surprisingly progressive course compared to patients with IgG4 (–) disease.4,5 Thus, the case reported had the typical characteristics of this condition.
At present, it is known that IgG4-RTD can encompass cases of (a) chronic autoimmune thyroiditis, (b) a fibrotic variant of this disease, (c) Riedel’s thyroiditis and (d) some uncommon cases of Graves’ disease.6
Regarding diagnosis of IgG4-RTD, although there are mixed criteria, the most commonly accepted criteria are those of the Japan Thyroid Association and the Japan Endocrine Society, which include: (1) gland enlargement, (2) hypoechoic lesions on ultrasound, (3) elevated serum IgG4 levels (≥135mg/dl), (4) thyroid histopathology findings such as infiltration of >20 IgG4+ plasma cells per high-power field and a proportion of IgG4+/IgG+ plasma cells >30%) and (5) involvement of other organs.7 As such, a patient is considered to have definitive IgG4-RTD when criteria 1–4 are met, probable IgG4-RTD when criteria 1+2+4 or 1+2+5 are met and possible IgG4-RTD when criteria 1+2+3 are met.
On the one hand, it should be stressed that histopathological findings are the most important elements for demonstrating IgG4+ plasma cell infiltration and for ruling out malignancy or other entities. On the other hand, it is important to note that elevated serum IgG4 levels are not sufficient by themselves to diagnose this entity, since elevated IgG4 is also characteristic of other diseases.8 Although histology in the case reported revealed a proportion of IgG4+/IgG+ plasma cells <30%, based on meeting all the other criteria, the clinical presentation, the epidemiological data and the fact that lymphoid clonality had been ruled out, the patient was considered to have definitive IgG4-RTD.
Concerning treatment, glucocorticoids and immunomodulators such as azathioprine, mycophenolate mofetil and methotrexate are treatments of choice in IgG4-RD.6 However, thyroid gland enlargement with significant compression of adjacent organs, constrictive symptoms or suspected malignancy lend themselves to a surgical strategy.9
In conclusion, knowledge of this condition is indispensable given that it will help physicians to decide the best strategy for diagnosis and treatment, since many of these lesions involve a mass raising clinical suspicion of malignancy, and in some cases unnecessary surgery may be avoided.
FundingThis research has not received specific funding from public sector agencies, the commercial sector or non-profit organisations.
Conflicts of interestThe authors declare that they have no conflicts of interest in relation to the publication of this scientific article.