Infertility affects millions worldwide and use of assisted reproductive techniques (ART) is in high demand.
AimsTo investigate whether women that underwent ART at our hospital had a higher incidence of GDM than women who conceived spontaneously, if the ART subtype affects the GDM rate and to study obstetrical outcomes in women with GDM in both groups.
MethodsThis was a retrospective analysis of prospectively collected data of singleton pregnancies attended at Hospital Universitari Dexeus between 2008 and 2019. Age<18 years, pregestational diabetes, metformin prior to pregnancy and multiple pregnancies were excluded.
ResultsA total of 29,529 patients were included. Pregnancy was achieved by ART in 2596 (8.8%): in vitro fertilisation (IVF/ICSI) 32.8%, frozen embryo transfer (FET) 37.7%, oocyte donor receptors (ODR) 17.2% and insemination 12.2%. The GDM rate was 8.9% (12.7% in ART vs 8.5% in non-ART, p<0.001). The GDM was 11.2% in IVF/ICSI, 17.7% in ODR, 13% in FET and 9.1% in the insemination group (p=0.001). In a multivariable analysis adjusting for age, parity and BMI, ART was not associated with GDM [OR 1.03 (0.90–1.19)], nor was type of ART. Pregnancy outcomes in GDM patients were similar in both groups except for C-section rates (30.0% in ART vs 15.9% in non-ART (p<0.001).
ConclusionsDespite a higher prevalence of GDM in ART pregnancies, ART was not associated with an increased risk of GDM when adjusting for age, parity and BMI. The prognosis of GDM in ART and non-ART was similar except for C-section rates.
La infertilidad afecta a millones de personas en todo el mundo y existe una gran demanda de técnicas de reproducción asistida (TRA).
ObjetivosInvestigar si las mujeres sometidas a TRA en nuestro hospital presentaron una mayor incidencia de diabetes mellitus gestacional (DMG) que aquellas que concibieron espontáneamente, conocer si el subtipo de TRA afecta a la tasa de DMG y estudiar los resultados obstétricos en mujeres con DMG en ambos grupos.
MétodosSe trató de un análisis retrospectivo de datos recogidos prospectivamente de los embarazos únicos atendidos en el Hospital Universitari Dexeus entre 2008 y 2019. Los criterios de exclusión fueron <18 años, diabetes pregestacional, uso de metformina antes del embarazo o embarazo múltiple.
ResultadosSe incluyó a un total de 29 529 pacientes. El embarazo se logró mediante TRA en 2596 (8,8%): fecundación in vitro (FIV/ICSI) 32,8%, transferencia de embriones congelados (TEC) 37,7%, receptoras de óvulos donados (ROD) 17,2% e inseminación 12,2%. La tasa de DMG fue del 8,9% (un 12,7% en pacientes sometidas a TRA, frente al 8,5% en pacientes no sometidas a TRA, p <0,001). Se observó una tasa de DMG del 11,2% en el grupo con FIV/ICSI, del 17,7% en el grupo con ROD, del 13% en el grupo con TEC y del 9,1% en el grupo con inseminación (p = 0,001). En un análisis multivariable ajustado por edad, número de partos e IMC, la TRA no se asoció a DMG (OR 1,03 [0,90--1,19]), ni tampoco el tipo de TRA. Los desenlaces de los embarazos en las pacientes con DMG fueron similares en ambos grupos, excepto en las tasas de cesáreas (un 30,0% en pacientes sometidas a TRA frente al 15,9% en pacientes no sometidas a TRA) (p < 0,001).
ConclusionesA pesar de una mayor prevalencia de DMG en los embarazos logrados con una TRA, esta no se asoció a un mayor riesgo de DMG cuando se ajustó por edad, número de partos o IMC. El pronóstico de la DMG en pacientes sometidas a una TRA fue similar al de aquellas pacientes no sometidas a una TRA, excepto por las tasas de cesáreas.
Infertility affects millions of people worldwide with rates increasing in the developed world mainly due to women delaying childbearing, among other factors. Consequently, use of assisted reproductive techniques (ART) is required by many couples. Pregnancies after ART are generally associated with worse prognosis, including more gestational diabetes mellitus (GDM), but it has not been clear whether this should be attributed to confounding factors, including maternal age, maternal BMI or multiple pregnancies.1–6 Factors related to the cause of infertility, drugs used for ovulation induction and luteal phase support as well as the hormonal environment after ovulation and early pregnancy could be associated with the increase in GDM in these patients.4,7 A potential worsening of underlying metabolic and vascular factors exacerbated during ART procedures could also be responsible for the increased rate of GDM. Ashrafi et al. found that type of ART and progesterone use for luteal support1 influenced the risk for GDM, but others did not.8
GDM is a controversial disorder without universal consensus with regards to diagnostic criteria and many different guidelines coexist.9–11 The World Health Organization-International Association for Diabetes in Pregnancy Study Group (WHO-IADPSG) criteria defined after the HAPO study, have been endorsed by different entities (WHO, International Federation of Gynaecology and Obstetrics [FIGO]) but not by others (the American College of Obstetricians and Gynecologists [ACOG], National Institute for Health and Care Excellence [NICE]). WHO criteria diagnose GDM in a single step: a 75g oral glucose tolerance test (OGTT) performed in the second trimester and requires only one glucose value above 92, 182 or 153mg/dl at 0–60 or 120min respectively for the diagnosis. In Spain, the Gestational Diabetes group of the National Diabetes Society recommends the classic two-step diagnostic protocol: first the O'Sullivan test and if ≥140mg/dl, a 100g OGTT interpreted with National Diabetes Data Group (NDDG) criteria (two above: 0h ≥105mg/dl, 1h≥190mg/dl, 2h≥165mg/dl, 3h≥145mg/dl); a change towards IADPSG criteria has not been recommended based on a national study since it would increase the rates of GDM and the pressure on the Public Health System without scientific evidence of clear benefit with intervention.12,13
Among the studies that have found an increased rate of GDM in ART pregnancies, most of them have used IADPSG criteria for the diagnosis or ADIPS (Australasian Diabetes in Pregnancy Society) in Australian studies.1,2,6–8
We aimed to investigate whether women that underwent ART at our Hospital had a higher incidence of GDM than women who conceived spontaneously. Another objective was to analyse if ART was related to the GDM rate and if the type of ART influenced that rate. We also aimed to evaluate the rate of second trimester fasting plasma glucose (FPG)>92mg/dl – as an approximation to WHO diagnostic criteria for GDM – according to ART and the rate of complications and obstetrical outcomes in women who developed GDM in both groups.
Patients and methodsThis was a retrospective analysis of prospectively collected data of all consecutive singleton pregnancies (n=29,529) attended at Hospital Universitari Dexeus between January 2008 and December 2019, who had complete data for all the main variables included in this study. Patients younger than 18 years, with pregestational diabetes, patients treated with metformin prior to pregnancy and multiple pregnancies were excluded. Only patients who were followed-up and delivered at our hospital were included. Informed consent was obtained from all patients and the reported investigations were carried out in accordance with the principles of the Declaration of Helsinki as revised in 2008.
All patients were managed according to standardised clinical protocols, homogeneous in terms of GDM screening and management throughout the study period, following the Spanish Diabetes Society-Diabetes and Pregnancy Group-recommendations.13 Screening for GDM was universal in the second trimester and targeted according to risk factors in the first trimester. Diagnosis was based on the two-step protocol: after an O'Sullivan test ≥140mg/dl, a 100g OGTT was performed. GDM was diagnosed according to NDDG criteria: two or more above: 105, 190, 165 and 145mg/dl at baseline, 1, 2 and 3h respectively after oral glucose.
Ovarian stimulation protocols have been previously described elsewhere. Briefly, ovarian stimulation was performed under gonadotrophins and pituitary suppression with gonadotrophin-releasing hormone analogues (agonists or antagonists) according to established protocols.14 Standard hormonal replacement protocol15 was used for endometrial preparation in frozen embryo transfer (FET) and oocyte donor receptors (ODR).
Data collectionClinical and biochemical data were prospectively collected throughout pregnancy and entered in standard computerised clinical records used in posterior statistical analysis. Demographics, smoking status, history of prior conditions and obstetric outcomes as well as physical examination data were collected at the first antenatal visit. The BMI was calculated as the weight in kg divided by the square height in metres (m2). All patients were managed according to homogenous standardised clinical protocols.
OutcomesMain outcomes were rate of GDM defined by NDDG criteria, rate of second trimester FPG>92mg/dl – as an approximation of GDM by WHO criteria – and rate of maternal and foetal complications in both groups: ART and non-ART patients with GDM.
Maternal outcomes included: primary caesarean delivery and gestational hypertensive disease (GHD) (including gestational hypertension and preeclampsia). Preeclampsia was defined as systolic blood pressure ≥140mmHg or diastolic blood pressure ≥90mmHg on ≥2 measures ≥6h apart and proteinuria of ≥1+ on a dipstick test or a 24-h urine protein ≥300mg. Gestational hypertension was diagnosed when the criteria for elevated blood pressure were met without proteinuria.
Perinatal outcomes included small for gestational age (SGA) (defined as birth weight below the 10th percentile for gestational age), macrosomia (defined as neonatal weight at or above 4000g), large for gestational age (defined as birth weight above 95th percentile), prematurity (defined as gestational age at delivery<37.0 weeks), severe prematurity (defined as gestational age at delivery<34.0 weeks) and Apgar score<7 at 1 and 5min.
Gestational age was defined as completed weeks based on last menstrual period or on the earliest ultrasound assessment if discordant.
Subtypes of ART were considered for group analysis: IVF/ICSI, frozen embryo transfer (FET), oocyte donor recipients (ODR) and inseminations.
Statistical analysisMean±standard deviation (SD), were reported for continuous variables, and number and percentage were reported for categorical variables (% (n)).
Categorical variables were compared using the chi-square test or the Fisher exact. Continuous variables were compared using the Student's T test. Finally, to explore if ART was associated with the rate of GDM a multivariable logistic regression (LR) model was also constructed to analyse possible predictors of GDM including maternal age, BMI at the first antenatal visit and parity.
All tests were bilateral with a significant level set to 5%. The statistical analysis was performed using IBM® SPSS® Statistics v22.0 and R (R Development Core Team, 2008) software.
ResultsA total of 29,529 patients were included in the study with a mean age of 34.9±4.3 years and mean BMI of 23.1±3.8kg/m2, 96.6% were Caucasian and 9% smokers. Pregnancy was achieved by means of ART in 2596 women (8.8%): 852 IVF/ICSI (32.8%), 980 FET (37.7%), 446 ODR (17.2%) and 318 inseminations (12.2%). The rest (26,933) were spontaneous pregnancies (91.2%).
Clinical characteristicsCharacteristics of women in the spontaneous pregnancy and ART groups are described in Table 1. As expected, women's age (38.49±4.71 vs 34.61±4, p<0.001) and nulliparity (77.8% vs 56.7%, p<0.001) were higher in the ART group compared with the spontaneous pregnancy group. Significant differences in pregnancy weight gain were found between the ART and spontaneous pregnancy groups (11.41±4.11 vs 12.18±4.04, p<0.001). However, we found no differences in the pre-pregnancy BMI between the two groups. Smoking habit (5.8% vs 9.3%, p<0.001) and previous C-section (4.8% vs 6.8%, p<0.001) were less common in the ART group.
Characteristics of women in the spontaneous group and ART pregnancies.
| Spontaneous pregnancies (N=26,933) | ART pregnancies | P value | |||||
|---|---|---|---|---|---|---|---|
| Global ART (N=2596) | IVF/ICSI (n=852) | FET (n=980) | ODR (n=446) | INS (n=318) | |||
| Mean maternal age (mean±SD) | 34.61±4.1 | 38.49±4.71 | 36.86±3.52 | 39.12±4.70 | 42.47±4.28 | 35.31±3.69 | <0.001*<0.001** |
| BMI (mean±SD) | 23.07±3.76 | 23.20±3.88 | 22.83±3.42 | 23.22±4.13 | 23.86±4.16 | 23.23±3.66 | 0.093*<0.001** |
| Weight gain (mean±SD) | 12.18±4.04 | 11.41±4.11 | 11.74±4.01 | 11.36±4.05 | 10.84±4.43 | 11.55±3.59 | <0.001*0.003** |
| Smoking %(n) | 9.3% (2209) | 5.8% (148) | 7.3% (61) | 4.6% (45) | 5.9% (26) | 5.1% (16) | <0.001*0.107** |
| Parity (Nulliparous) %(n) | 56.7% (15,278) | 77.8% (2020) | 84.6% (721) | 70.6% (692) | 79.1% (353) | 79.9% (254) | <0.001*<0.001** |
| Previous C-section %(n) | 6.8% (1828) | 4.8% (125) | 2.7% (23) | 6.8% (67) | 4.3% (19) | 5.0% (16) | <0.001*0.001** |
ART: assisted reproductive techniques; BMI: body mass index.
The GDM global rate was 8.9% (2632). If we compare the different study groups, the GDM rate was 12.7% (330) in pregnancies by ART compared to 8.5% (2302) in non-ART pregnancies (p<0.001). According to the ART subtypes, GDM was 11.2% (95) in the subgroup of IVF/ICSI, 17.7% (79) in ODR, 13% (127) FET and 9.1% (29) in the insemination group (p=0.001).
Rates of second trimester FPG>92mg/dlOverall, 8.8% (815) of patients had FPG>92mg/dl, 11.9% (104) in the ART group and 8.5% (711) in the spontaneous pregnancy group (p=0.001). In the DMG group 20.7% of the ART pregnancies had FPG>92mg/dl and 15.5% of spontaneous pregnancies (Table 2).
Pregnancy outcomes in GDM patients in ART vs non-ART.
| Spontaneous pregnancies %(n)8.5 (2302) | Total ART pregnancies%(n)12.7 (330) | P value | |
|---|---|---|---|
| Glu>92mg/dl | 15.5 (137/885) | 20.7 (30/145) | 0.075 |
| Elective C-section | 15.9 (367) | 30.0 (99) | <0.001 |
| GHD | 3.2 (74) | 5.2 (17) | 0.072 |
| SGA ( | 7.5 (172) | 8.5 (28/) | 0.289 |
| IUGR ( | 1.3 (30) | 0.3 (1) | 0.084 |
| Preterm delivery<34 | 0.7 (15) | 1.5 (5) | 0.095 |
| Preterm delivery<37 | 4.6 (106) | 6.7 (22) | 0.103 |
| Apgar 5<7 | 0.2 (4/2273) | 0.3 (1/326) | 0.459 |
| Apgar 1<7 | 1.6 (36/2275) | 2.1 (7/327) | 0.489 |
| Macrosomia | 4.7 (108) | 4.5 (15) | 0.906 |
| LGA | 11.8 (272) | 10 (33) | 0.335 |
Glu: glucose; LGA: large for gestational age; SGA: small for gestational age; IUGR: intrauterine growth restriction; ART: assisted reproductive techniques; FET: frozen-thawed embryo transfer; IVF: in vitro fertilisation; ins: insemination.
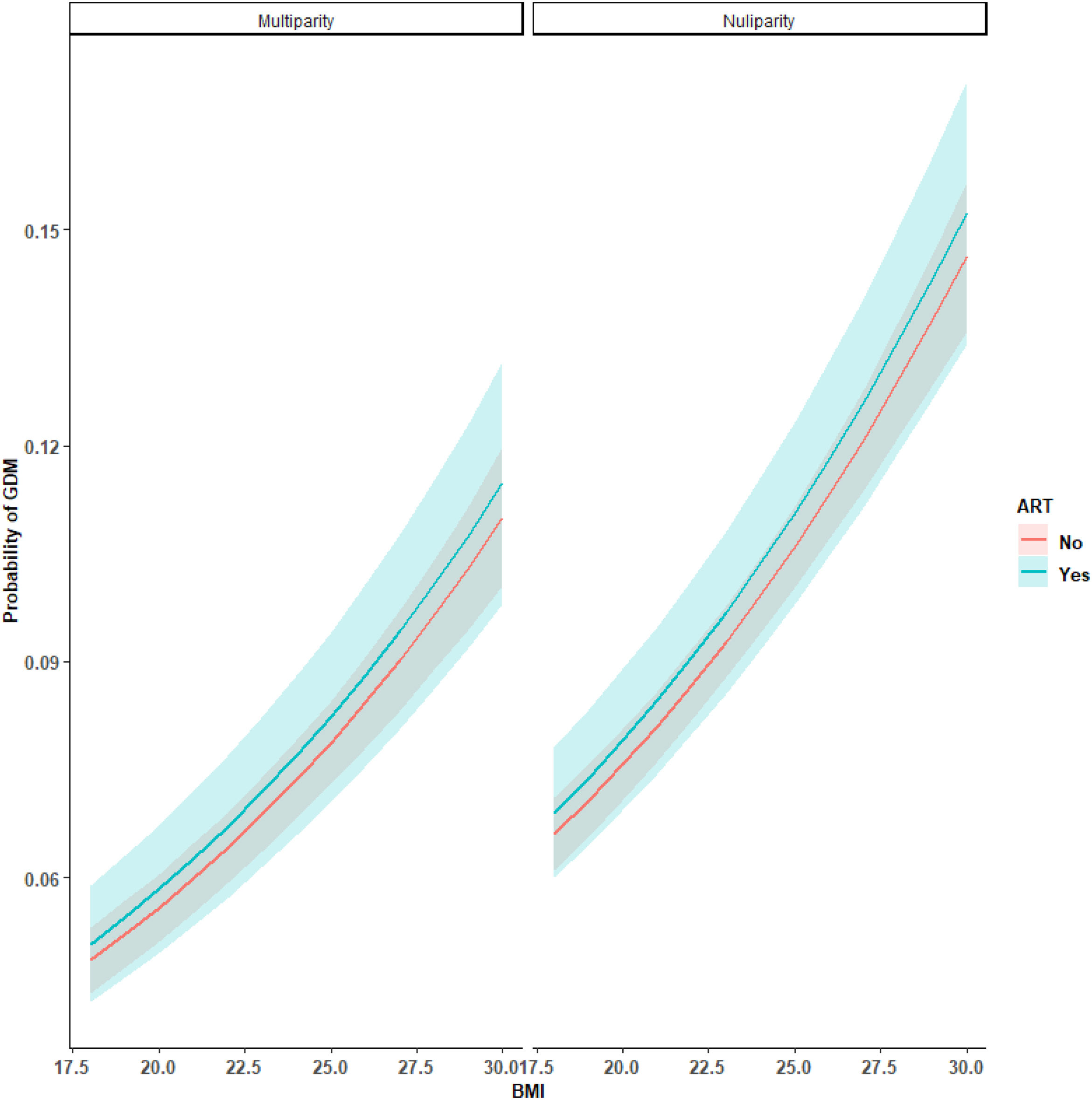
In a multivariable analysis adjusted by confounding factors (maternal age, BMI and parity), we observed that ART was not an associated factor for GDM [OR 1.03 (0.90–1.19)] (Table 3).
GDM multivariant logistic regression adjusted by maternal age, BMI, parity and assisted reproductive techniques.
| OR | 95% CI | |
|---|---|---|
| Maternal age | 1.09 | [1.07; 1.10] |
| BMI | 1.08 | [1.07; 1.09] |
| Parity (nulliparity) | 1.33 | [1.21; 1.45] |
| ART | 1.03 | [0.90; 1.19] |
ART: assisted reproductive techniques; BMI: body mass index; CI: confidence interval; OR: odds ratio; GDM: gestational diabetes.
We built a model (Fig. 1) to report the probability of GDM in mean age, adjusted by BMI and ART, in nulliparous and multiparous women.
Pregnancy outcomes in GDM patients in ART vs non-ARTPregnancy outcomes were similar in both groups except for C-section rates. There were no differences in GHD, SGA, LGA, preterm<34 GW or <37 GW, Apgar score or macrosomia rates in both groups. C section rates were 30.0% in ART patients versus 15.9% in non-ART (p<0.001) (Table 2).
DiscussionThe present study provides epidemiological data and pregnancy outcomes in a large population of pregnant patients by means of ART (n=2596) compared to spontaneous pregnancies (n=26,933). Rates of GDM were much higher in ART patients (12.7% vs 8.5%) but in multivariable analysis, ART was not associated with this outcome. We also found significant differences in GDM rates between different ART subtypes: IVF/ICSI, FET, ODR and inseminations but these groups were not comparable in variables known to affect GDM rates.
Pregnancy outcomes were similar between GDM in spontaneous and ART pregnancies except for C-section, suggesting that ART does not confer an additional risk for the other complications of GDM studied.
Pregnancies after assisted reproduction are thought to be associated with worse prognosis than spontaneous pregnancies, including more GDM,6–8 but it has not been clear to date whether this is due to confounding factors, including age or twin pregnancies; studies have also used different diagnostic criteria for GDM. The present study is based on a very large cohort of pregnant women from a single University Hospital followed by a homogeneous protocol, criteria for GDM diagnosis was based on the two-step protocol, the 100g OGTT and the NGGD cut-offs. We found an increased rate of GDM in ART but the multivariable analysis does not support any influence, and other factors including age, BMI and parity seem to explain the differences among ART versus the non-ART groups.
Different authors have assessed GDM rates in patients undergoing ART. Different studies have used different GDM diagnostic criteria and reported rates of GDM are different, probably accordingly to that. Some authors have found ART to be independently related to GDM but many studies are cross-sectional and retrospective1,6 and many did not exclude multiple pregnancies or patients with prior metformin use as we did. These variables may have influenced our findings. Other large studies lack clinically relevant information and/or did not control for clinically relevant confounding factors.16,17 Silberstein et al.,18 in a large cohort including pregnancies conceived by IVF (n=1296) and ovulation induction (n=1988) as compared to singletons conceived spontaneously (n=172,288), found a significant linear association among the three groups for GDM (17.3% in IVF, 14.2% in ovulation induction and 6.6% in the control group), severe preeclampsia (2.7% in IVF, 1.8% in ovulation induction, 1.1% in the control group) and overall perinatal mortality (3.3% in IVF, 2.1% in ovulation induction and 1.3% in the control group). In the multivariable analysis, both IVF and ovulation induction treatments were found to be independent risk factors for GDM. In this particular study GDM rates were similar to ours, though GDM diagnostic criteria were not specified.
Carbillon et al.19 found a greater rate of GDM after ART than after spontaneous pregnancies (17.6% vs 14.2%, p<0.05). They also found a higher prevalence of GDM after ovulation induction followed by assisted-reproduction procedures (18.3%) than after ovulation induction only (15.5%). Upon multivariable analysis, women who had ART compared with those who had spontaneous pregnancies or pregnancies after ovulation induction only, had a higher risk of gestational diabetes with an odds ratio of 1.32 (p<0.05).
The present study also aimed to understand the prognosis of assisted-reproduction pregnancies with gestational diabetes. We found a similar prognosis of GDM independent of ART, except for C-Section. Carbillon et al.19 found higher rates of GDM (by WHO criteria) and more obstetric complications in ART, but this was mainly driven by polycystic ovarian syndrome (PCOS), a population that in the present study was less represented since metformin use prior to pregnancy was an exclusion criterion, and PCOS patients in our hospital are usually on metformin prior to conception. Koukhan et al.,6 in a nested case-control study with a more limited number of patients, found higher complications of GDM (by WHO criteria) in women who had ART versus spontaneous pregnancies. It is also possible that NDDG criteria and WHO criteria identify different subtypes of GDM (more baseline hyperglycaemia in those by WHO criteria) and this may be another factor related to the different results.
Other authors have also found worse obstetric results in ART pregnancies.1,17,20 Shevell et al.20 reported pregnancy outcomes in a cohort of 36,062 pregnancies, 1776 (4.9%) by means of ART, separating those who had IVF vs. ovulation induction in the ART group. Ovulation induction was associated with a statistically significant increase in placental abruption, foetal loss after 24 weeks, and although gestational diabetes was increased, it did not meet criteria for achieving statistical significance after adjustment. Use of IVF was associated with a statistically significant increase in preeclampsia, gestational hypertension, placental abruption, placenta previa, and risk of caesarean delivery but they did not report complications in the GDM groups only.
Limitations of the present study include the retrospective nature of data analysis, the lack of some clinical information like family history of diabetes and as our hospital is a private institution it may be a bias in the population included in the study, but its strengths are the large sample and the homogeneity of care of the population included.
In conclusion: Despite a higher prevalence of GDM in ART pregnancies, ART was not associated with an increased risk of GDM when adjusting for age, parity and BMI. The prognosis of GDM in patients undergoing ART is similar to those with spontaneous pregnancies except for C-section rates.
Authors’ contributionsGS, PP and MA: substantially contributed to the design, review and interpretation of the results. SG and IR: carried out a lot of work by performing all the statistical analysis. IR and MG: significantly contributed by collecting data and writing some parts of the main document. BS and ARM: as a senior consultant, substantially contributed to the final review of the study. GA and PP: main authors, both first authors of the article. Developed the idea of the study, collected data, wrote a major part of the manuscript and reviewed all the documents for submission. All authors have read and approved the manuscript.
Availability of data and materialsAll data generated or analysed during this study are included in this published article. Supplementary information files are also available on request.
Consent for publicationNot applicable.
FundingNo funding was received for this study.
Conflict of interestsThe authors declare that they have no competing interest.
This study has been carried out under the auspices of the Càtedra d’Investigació en Obstetrícia i Ginecologia of the Autonomous University of Barcelona, Spain