Thyroid disease in the context of IgG4-related disease (IgG4-RD) may be indistinguishable from malignant thyroid disease if specific findings are not sought. However, differentiating them is of paramount importance, since the treatment of choice for the two conditions is radically different.
IgG4-RD is an immune-mediated fibroinflammatory disease characterised by organomegaly or nodular/hyperplastic lesions in different bodily organs, with tissue infiltration by IgG4-positive plasma cells and elevated serum IgG4 concentrations.1,2 It is rare, with six cases per 100,000 inhabitants in Japan, the country with the most reported cases.3 It primarily affects men between the age of 50 and 69 years.2 IgG4-RD usually responds to treatment with corticosteroids or immunosuppressants.1 However, in some cases it can simulate other inflammatory disorders, infections or even neoplasms,2,4 so it is important to distinguish it from other entities to avoid unnecessary aggressive treatments.1
We present a clinical case in which the differential diagnosis between malignant thyroid disease and IgG4-RD was challenging, even after pathological analysis. The patient was a 59-year-old man with a history of primary hypothyroidism undergoing treatment with levothyroxine 100μg/24h, who was seen at the emergency department for a one-month history of dysphagia and dyspnoea at rest (decubitus) associated with a non-painful anterior cervical mass. The patient had no fever or other systemic symptoms. Physical examination revealed grade 4 goitre with stony-hard consistency and right predominance. A chest X-ray was performed, showing a cervical mass with an endothoracic component that appeared to compromise the airway. For this reason, he was assessed by Otorhinolaryngology, and it was decided to complete the study on a scheduled basis with ultrasound, revealing giant goitre (RTL [right thyroid lobe] 216cc [5.6×6.2×12cm] and LTL [left thyroid lobe] 110cc [4.2×4.6×11cm]). During the same examination, an ultrasound-guided core needle biopsy (CNB) was performed. With the results pending, the patient was referred to Endocrinology, where laboratory testing with thyroid profile was requested, revealing TSH 6.91mIU/l, anti-TPO Abs >1300IU/ml and anti-Tg Abs >3000IU/ml, for which reason levothyroxine was increased to 125mcg/24h.
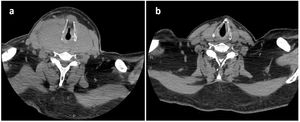
The day after the last consultation, the patient returned to the emergency department due to clinical worsening, with dyspnoea at rest. An urgent neck CT scan revealed compression of the airway at the level of the hypopharynx, due to the large goitre already described by ultrasound, which extended from the hypopharynx to the plane of the sternoclavicular joint (Fig. 1a). The patient required orotracheal intubation (which required exeresis of the thyroid isthmus) and admission to the ICU.
Despite an initially torpid course, the patient improved after intensive empirical corticosteroid therapy. With the patient already on the ward, an attempt was made to advance the diagnosis:
- •
On the one hand, CNB prior to admission was reported as a diffuse lymphoid infiltrate of low cytological grade of the thyroid parenchyma, with the most probable diagnostic possibility being a lymphoproliferative process that affected the thyroid in a diffuse way.
- •
On the other hand, a PET-CT scan performed during admission showed thickening of the thyroid gland with low intensity uptake, without being able to differentiate inflammatory activity from a low-grade neoplastic lesion.
Total thyroidectomy was considered, but postponed because of the patient’s surprising clinical improvement with empirical corticosteroid therapy. Finally, the pathological analysis of the isthmectomy specimen revealed diffuse B and T cell lymphoid infiltrate of the thyroid gland suggestive of lymphocytic thyroiditis.
Given the marked clinical improvement, and despite not having a definitive diagnosis, one and a half months after admission, the patient was discharged from hospital with oral corticosteroid therapy, pending possible thyroidectomy. One month after discharge, the control CT scan found a significant reduction in mass size (RTL 23cc [2.8×2.1×7.5cm] and LTL 21cc [2.9×1.7×6.6cm]) (Fig. 1b), and laboratory tests revealed elevated serum IgG4 (307mg/dl), which accounted for more than 40% of total IgG. For this reason, an immunohistological review of the isthmectomy specimen was requested by pathology, which showed >60 IgG4+ cells/high power field.
This finding confirmed the diagnosis of Riedel’s thyroiditis in the context of IgG4-RD, as the diagnostic criteria for IgG4-RD published in 2011 and reviewed in 2020 were met5:
- 1)
Clinical-radiological characteristics: one or more organs with diffuse or localised swelling or a mass or nodule (involvement of a lymph node, with no other organ affected, is not included as a criterion).
- 2)
Serological diagnosis: IgG4 serum levels >135mg/dl.
- 3)
Pathological diagnosis: positivity for two of the following criteria:
- o
Dense infiltration of lymphocytes and plasma cells with fibrosis.
- o
More than 10 IgG4+ plasma cells/high power field and IgG4+/IgG+ cell ratio >40%.
- o
Typical tissue fibrosis, particularly storiform fibrosis or obliterative phlebitis.
Definitive diagnosis requires that all three criteria be met. If only the first and third criteria are met it will be a ‘probable’ diagnosis, whereas if only the first and second are met it will be ‘possible’.2,5 Subsequently, specific criteria for IgG4-RD have been established for several organs.1 There are still no well-established criteria for IgG4-related thyroid disease, although recently some criteria have been proposed that include the morphological characteristics of the thyroid by ultrasound.3
In any event, immunohistological examination is key to a definitive diagnosis, and should be performed whenever possible.2,4 In our case, malignant thyroid disease was ruled out, so thyroidectomy was dismissed. Given that the biological agent most often used in IgG4-RD is rituximab,4 with a good response in up to 97% of cases,2 this therapy was started in our patient, with subsequent normalisation of serum IgG4 and a good clinical outcome.
In conclusion, we wish to emphasise the importance of always keeping IgG4-RD in mind in the differential diagnosis of a thyroid mass, since early diagnosis prevents unnecessary invasive treatments.
We would like to thank all the professionals who have collaborated to make this study possible.