Arterial hypertension (HT) is the main risk factor for cardiovascular disease and it affects ∼50% of the Spanish adult population.1 Primary aldosteronism (PA) is a chronic, progressive endocrine disorder that is the main cause of HT; it is found in 10–15% of the hypertensive adult population in general2 and in 30% in cases of severe and/or resistant HT. PA is a major cardiovascular risk factor.3,4 It increases the risk of death, stroke, coronary heart disease, chronic kidney disease, atrial fibrillation, left ventricular hypertrophy and heart failure more than essential HT and regardless of blood pressure levels. Early detection can therefore save lives and improve the quality of life of those affected.5,6
Considering the public health impact of PA, all clinicians should be familiar with its management. However, the reality is that identifying PA can be complex, which partly explains the high rate of underdiagnosis.7 This seems to be no different among endocrinologists in Spain. Studies from the Spanish PA registry report high rates of hypokalaemia, suggesting that PA is diagnosed in advanced stages, even in very obvious cases.8 A recent Spanish national survey on the treatment of PA by Spanish endocrinologists9 showed that there is great variability in this area, and that there is a lack of subtyping studies, findings similar to those reported by other authors.8 Additionally, it was reported that only 35% of departments had a specific specialist in PA and that, although 67% had an HT clinic/unit at their hospital, these came under other specialist areas. It is likely that the establishment of specific referral centres/units/clinics in HT with endocrinologists subspecialising in PA would improve the management of this condition.
Our department boasts a specific endocrine hypertension clinic (C-HT-Endo), which has been running since January 2022. We report here how this clinic has affected the diagnosis of PA and we discuss our experiences so far.
Operational structure of the clinicSuspected cases of endocrine hypertension, mainly PA, have been channelled to two endocrinologists since July 2021, and the C-HT-Endo has been running as a specific service two days a week since January 2022. In parallel with the creation of the clinic and once it was up and running, informative sessions were held with the hospital's Nephrology, Interventional Radiology, Internal Medicine, Cardiology, Urology and Pathology departments to coordinate diagnostic-therapeutic strategies. The patients are referred from the Nephrology HT clinic or from our own department. The reason for referral is suspected endocrine hypertension, which includes PA, pheochromocytoma/paraganglioma, Cushing's syndrome and acromegaly. In the case of PA, in addition to clinical suspicion, an aldosterone-renin ratio value >20 ng/dl/ng/mL/ with blood aldosterone (Aldo) >8 ng/dl was agreed on (measured with or without drugs that interfere with the renin-angiotensin-aldosterone system). For the diagnosis of PA, apart from clinical exceptions, two of the following functional tests are performed using the published protocol and cut-off points,2 in accordance with the latest European consensus:10 captopril challenge test with captopril 25 mg; oral salt loading test; and intravenous saline loading test. For the study of other causes of endocrine HT, the recommendations of the respective clinical guidelines are followed.
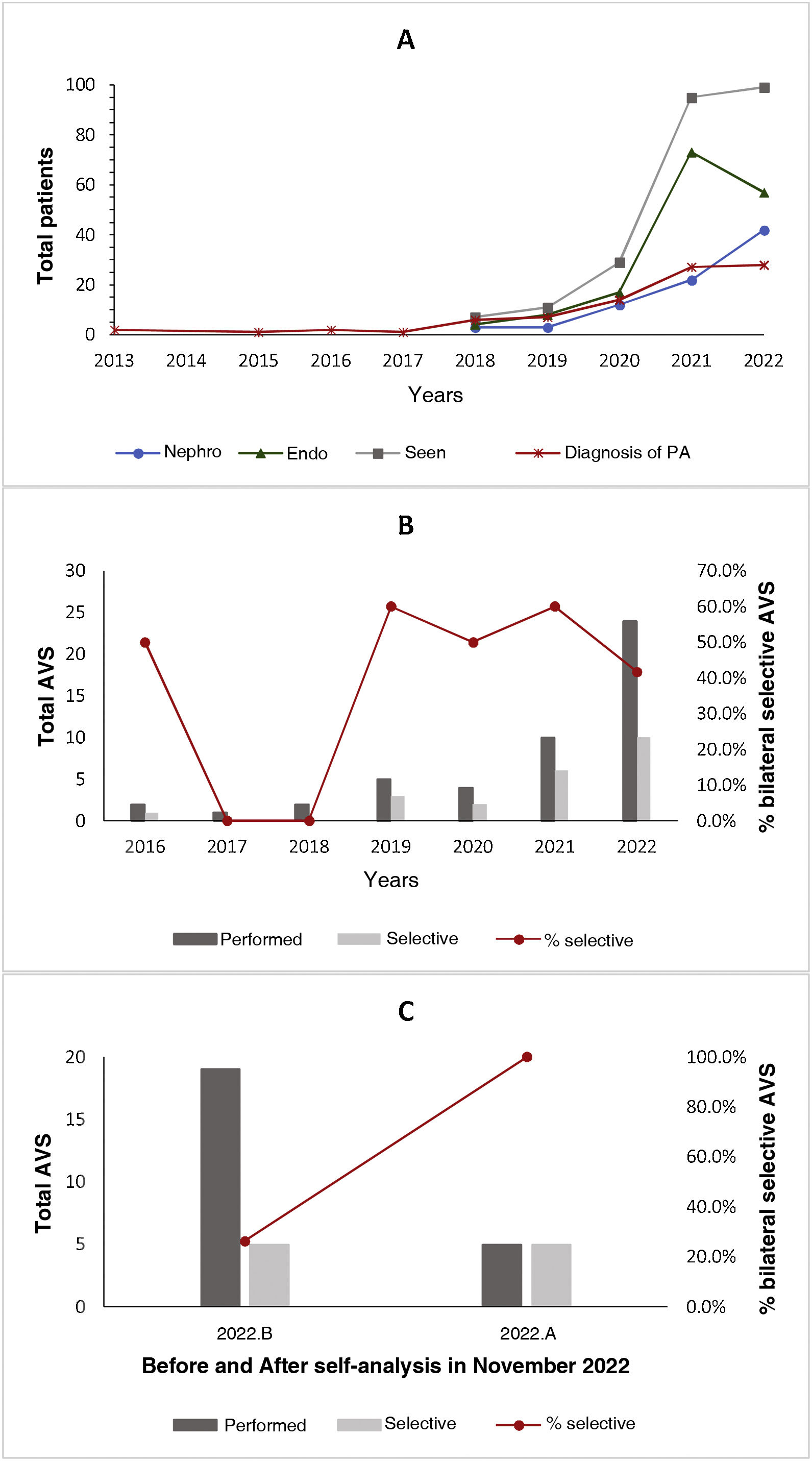
Impact of the C-HT-Endo on the diagnostic approach to PAFrom July 2021 to December 2022, 144 patients were seen at the C-HT-Endo, 56 (38.8%) referred from Nephrology and the rest from our department. Of the 144 patients, PA was diagnosed in 46 (31.9%), and no other cause in the rest. With the clinic, compared to previous years, we have seen a markedly progressive increase in the cases investigated and diagnosed with PA, as well as in the number and the diagnostic yield of adrenal venous sampling procedures performed (Fig. 1).
A) Changes in cases seen in the clinic over time according to their origin, referred from the Nephrology (Nephro) or Endocrinology (Endo) departments, and diagnosed with primary aldosteronism. B) Changes over time in the total number of adrenal venous samplings (AVS) performed and in AVS with an adequate bilateral selectivity rate. C) Difference in AVS with adequate bilateral selectivity in the last month of 2022, before and after a multidisciplinary meeting in which the consultation data were self-analysed.
First of all, although there are clinical guidelines for the management of HT of endocrine origin, apart from PA, it is still a group of unusual diseases, which are highly heterogeneous from a clinical point of view. The logistical constraints of adapting the approach to the particular situation of each centre and getting a clinic of this type effectively up and running are many. Multidisciplinary coordination with the departments involved is therefore imperative to turn what were initially weaknesses into strengths. Secondly, there is no gold standard for diagnostic or therapeutic action in many of these diseases, especially when "unusual/complicated" cases occur. Moreover, as in the case of PA, the performance of many screening/diagnostic tests can vary depending on pre-analytical factors or cut-off points used, or due to the nature of the disease. In PA, the higher the cut-off point of the aldosterone-renin ratio used for screening, the lower its sensitivity, although the higher its specificity; sitting/standing and some drugs induce different values of aldosterone and renin; and production of aldosterone is not always homogeneous, continuous and completely autonomous. Therefore, doctors who run a C-HT-Endo need to have a thorough knowledge of these situations and be aware that interpreting tests and medical decisions often have to be personalised according to the clinical context. This makes it crucial to have clinical meetings/committees in place for the discussion and study of cases. Lastly, in order to effectively manage endocrine hypertension, it is also necessary to have detailed knowledge of essential hypertension, so training in the field of HT beyond endocrine causes is vitally important.
In conclusion, having a C-HT-Endo has probably led to a more active search for cases of PA by the rest of the physicians, and this would explain the marked increase in the diagnosis of PA in our series. It should also translate into more patients benefiting from better cardiovascular protection after appropriate treatment, which is something we hope to corroborate in the future. We therefore deem the role of an endocrinologist specialising in HT and their participation in HT clinics/units to be vital.
Authors/contributors- 1
Conception and design of the manuscript: JGR-S.
- 2
Data collection: JGR-S and DM.
- 3
Data analysis and interpretation: JGR-S.
- 4
Drafting, review and approval of the submitted manuscript: JGR-S and DM.