The prevalence of obesity has increased dramatically in children worldwide. Obesity has been recognized as a risk factor for more serious viral respiratory infections, mainly in adults.
ObjectiveTo study the relationship between overnutrition (obesity and overweight) and clinical severity in children hospitalized with acute respiratory infections of viral origin.
MethodsOne hundred and forty-three clinical records of children between 2 and 18 years old hospitalized for acute respiratory infection at Clínica Dávila (2014–2018) were analyzed, recording the respiratory viruses detected at the time of hospitalization, weight, and height. Nutritional status was estimated using Z score or body mass index, according to age.
ResultsEighty-tree3 children (58%) were positive for more than one respiratory virus. The main virus detected in monoinfection was adenovirus (9.8%), followed by respiratory syncytial virus (7.7%) and parainfluenza virus (7.7%). There were no deaths. Patients with obesity presented more days of hospitalization (P = .04), oxygen therapy (P = .03) and mechanical ventilation (P < .001), as well as a higher probability of requiring mechanical ventilation (P = .001) and of ICU admission (P = .003) compared with children with normal weight. Patients with overweight presented more days of mechanical ventilation (P < .001) than patients with normal weight. No significant differences were found between the presence of viral coinfection and nutritional status.
ConclusionOvernutrition is associated with greater severity of viral respiratory infection in hospitalized children.
La prevalencia de obesidad se ha incrementado dramáticamente en menores de edad a nivel mundial. La obesidad ha sido reconocida como un factor de riesgo para infecciones respiratorias virales más graves, principalmente en adultos.
ObjetivoEstudiar la relación entre exceso de peso (obesidad y sobrepeso) y gravedad clínica en menores de edad hospitalizados con infecciones respiratorias agudas de origen viral.
MétodosSe analizaron 143 historias clínicas electrónicas de menores entre 2 y 18 años hospitalizados por infección respiratoria aguda en Clínica Dávila (2014–2018), registrando los virus respiratorios detectados al momento de la hospitalización, peso y estatura. El estado nutricional se estimó mediante las puntuaciones Z o índice de masa corporal, según edad.
ResultadosOchenta y tres menores (58%) fueron positivos a más de un virus respiratorio. El principal virus detectado en monoinfección fue adenovirus (9,8%), seguido de virus respiratorio sincitial (7,7%) y virus parainfluenza (7,7%). No hubo fallecidos. Los pacientes con obesidad presentaron más días de hospitalización (p = 0,04), de oxigenoterapia (p = 0,03) y de ventilación mecánica (p < 0,001), así como mayor probabilidad de requerimiento de ventilación mecánica (p = 0,001) y de ingreso a UCI (p = 0,003) comparado con los menores con normopeso. Los pacientes con sobrepeso presentaron más días de ventilación mecánica (p < 0,001) que los pacientes con normopeso. No se encontraron diferencias significativas entre presencia de coinfección viral y estado nutricional.
ConclusiónEl exceso de peso se asocia a una mayor gravedad de la enfermedad causada por la infección respiratoria viral en menores de edad hospitalizados.
The global prevalence of childhood obesity has increased drastically in the last three decades and is a serious global problem.1 In Latin America and the Caribbean, 61% of females are overweight. In Mexico and Chile, more than 75% of the female population is overweight. Similarly, 53% of men in Latin American and Caribbean countries are overweight. Chile tops the list with 74% of its male population being overweight, followed by Mexico (70%) and Argentina (66%).2 Furthermore, childhood obesity has increased significantly in Chile, where 45% of children under 18 years of age suffer from overnutrition (overweight and obesity); considerably higher than the Organisation for Economic Co-operation and Development (OECD) average, which is around 25%.3
Obesity is characterised by an imbalance in hormone levels and plasma glucose and lipid concentrations,4 in addition to being considered a chronic state of inflammation with systemic implications for immunity.5 This disease is recognised as the basis for the development of multiple diseases in both adults and children. Because obesity has increased in recent years, the incidence of type 2 diabetes mellitus has risen to 25%–45% of all young people diagnosed with diabetes.6 In turn, it is estimated that 30% of coronary heart disease and ischaemic stroke and almost 60% of hypertensive disease in developed countries can be attributed to excess body mass index and hypercholesterolaemia7,8 and an association with the severity of the clinical course in viral respiratory infections has recently been identified.9 The current SARS-CoV-2 pandemic, which causes the coronavirus disease (COVID-19), has revealed the impact of obesity on the severity of the viral infection. Patients with obesity are more likely to be hospitalised with COVID-19 and are at greater risk for mechanical ventilation and death.10 According to the latest report from the Chilean Ministry of Health (MINSAL), obesity is one of the main comorbidities in patients with COVID-19, with obesity reported in 5.8% of hospitalised patients and in 1.4% of those not hospitalised.11 Just as for SARS-CoV-2 infection, obese patients with influenza are at greater risk for hospitalisation and death, and longer hospital stay and duration of mechanical ventilation than normal-weight patients.12,13 In Chile, a study conducted in adults hospitalised for influenza A H1N1 in 2009 concluded that obese patients should be closely monitored as they have a high risk of clinical failure.14
Acute respiratory infections represent a major public health problem, with significant morbidity and mortality in children under two years of age.15,16 Some of the main classical viruses that cause acute respiratory infections in children are: respiratory syncytial virus (RSV), human parainfluenza virus (1–4), influenza virus, adenovirus (AdV), human rhinovirus (RV), human metapneumovirus, human coronaviruses (HKU1, NL63, 229E and OC43), human enterovirus (EV) and human bocavirus.16,17 Although there are several studies that relate nutritional status with the severity of COVID-19 in children,18–22 this relationship has been less studied in the case of classical respiratory viruses.16,23,24
All of the above points to a need to study the relationship between nutritional status and severity of the clinical course in patients under 18 years of age. The objective of our study was to investigate the relationship between overnutrition (obesity and overweight) and the severity of infection in minors (2–18 years of age) hospitalised for viral respiratory infection in a hospital setting in Chile, over a period of four consecutive years prior to the COVID-19 pandemic.
Material and methodsStudy populationA retrospective, observational, correlational study was conducted with clinical data from children hospitalised for viral respiratory infection at the Clínica Dávila hospital centre (Metropolitan Region, Chile) between the months of March and August from 2014 to 2018. Thirty patients were randomly selected each month from a Clínica Dávila database, using the Randomizer program. Patients were selected based on the following inclusion criteria: minors between two and 18 years of age admitted for viral respiratory infection. The exclusion criteria were: children at nutritional risk or with malnutrition, with prematurity, and patients with immunodeficiency and/or chronic lung disease. Patients whose age, nutritional status, weight and height were not recorded in their electronic medical record were not considered. The following clinical and epidemiological variables were recorded for each patient: gender, age, weight, height, length of hospital stay in days, number of days on oxygen, days on mechanical ventilation, mechanical ventilation requirement and intensive care unit (ICU) admission.
Nutritional assessmentNutritional status was evaluated with the variables weight, height and age.25 The children were classified into three groups according to their nutritional status using the WHO Anthro 2011 v.3.2.2 and WHO AnthroPlus software: normal weight, overweight and obesity. Nutritional status was determined using the weight-for-height z-score in children aged two to four years and the body mass index for age was used in children aged five years and over. Normal weight was defined as −0.9 to 0.9 SD, overweight as 1.0 to ≤2.0 SD, and obesity as >2 SD. Children at nutritional risk were defined as having a weight-for-height <1 SD, being below the mean, and they were therefore excluded from the study.
Respiratory virusesThe viral panel analysis reported for respiratory viruses was recorded from the electronic medical record, which, according to the regulations of the medical centre, must be performed on all patients hospitalised for respiratory disease. Polymerase chain reaction (PCR) was used to detect multiple respiratory viruses from a respiratory sample obtained from each patient upon hospitalisation. Two PCR detection systems were used: a conventional multiplex PCR, Allplex™ RP1-RP4 (Seegene Inc., Songpa-gu, Seoul, Korea); and the BioFire® FilmArray® system (BioFire Diagnostics, Salt Lake City, UT, USA) using multiplex PCR where several PCR reactions are combined and carried out simultaneously, to establish syndromic diagnoses. The BioFire® system multiplex panel targets a whole group of viruses and bacteria that cause infections of the respiratory system or respiratory panel. Viruses included in both viral panels were: RSV, human metapneumovirus, human parainfluenza virus 1–4, human coronavirus (229E, NL63, HKU1 and OC43), AdV, human bocavirus, influenza A, influenza B and a single detection probe for RV/EV in the case of the BioFire® FilmArray®, and RV and EV in Allplex™ RP1-RP4. Patients were classified as having monoinfection when the report indicated the presence of one virus in the respiratory sample, or coinfection when the report indicated the presence of more than one virus in the respiratory sample.
Ethical considerationsThe project was approved by the Clínica Dávila Ethics Committee (290621). Authorisation to review the electronic medical records was requested, as well as an informed consent exemption.
Statistical analysesThe normality of continuous and discrete variables was evaluated with the Shapiro-Wilk test. The association between nutritional status (e.g., normal weight, overweight and obesity) as an explanatory variable, and severity, as a response variable, was estimated with multivariate Poisson models for discrete severity variables (e.g., length of hospital stay in days, days on oxygen therapy, days on mechanical ventilation) and with multivariate logistic models for dichotomous severity variables (e.g., requirement for mechanical ventilation and admission to the ICU). The association between nutritional status, as an explanatory variable, and viral coinfection, as a response variable, was estimated with a multivariate logistic model. For Poisson regression models, the coefficients transformed into the incidence rate ratio are reported, while for logistic regression models the odds ratio is reported. In the multivariate models, age (in years), gender (female = 1) and viral coinfection (yes = 1) were used as control variables. A significance level of 5% was applied. The analyses were carried out using the STATA 14.1 program.
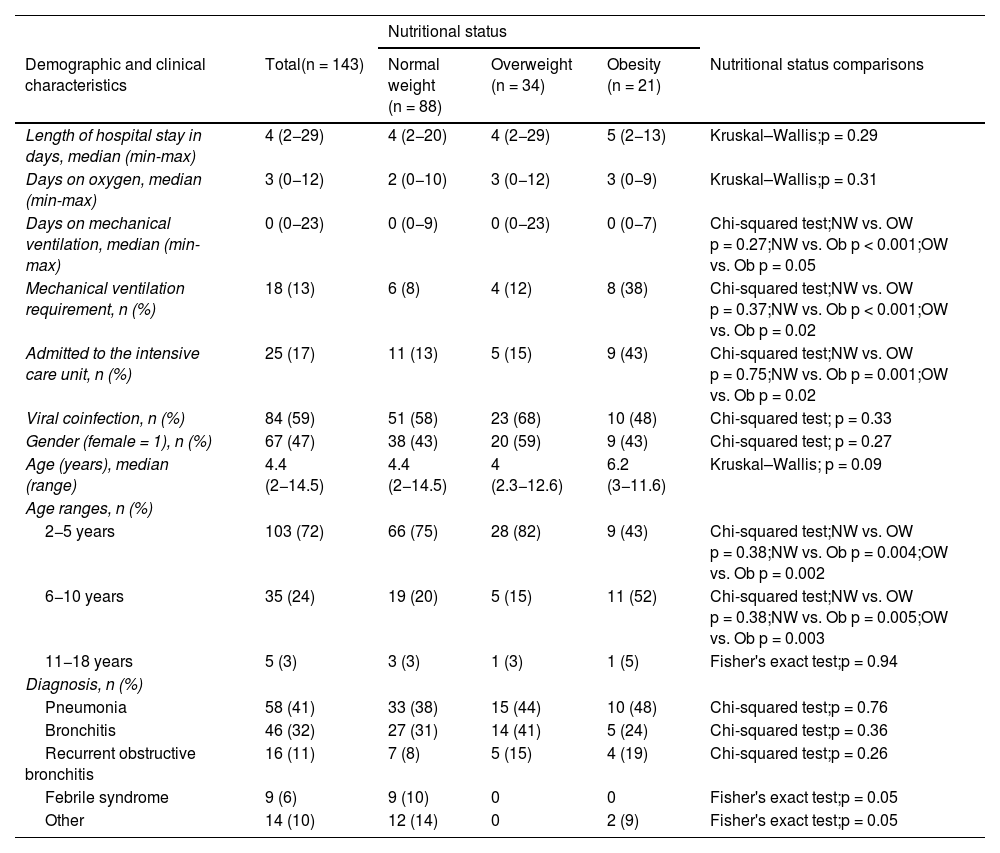
ResultsA total of 192 electronic medical records were examined. After applying the inclusion and exclusion criteria, 143 children were eligible. The clinical and demographic characteristics of the children included in the study according to nutritional status are shown in Table 1. Most of the children included in the study were between two and five years of age (103; 72%). It was found that 55 (38%) of the patients suffered from overnutrition, with the main diagnosis at discharge being pneumonia (58; 41%), followed by bronchitis (46; 32%). The bivariate analysis between clinical and demographic variables according to nutritional status revealed that children with obesity had a shorter range of days on mechanical ventilation (p < 0.001), a higher frequency of requirement for mechanical ventilation (p < 0.001) and a higher frequency of admission to the ICU (p = 0.001) than children with normal weight.
Summary of clinical and demographic data of children hospitalised with acute respiratory infections at Clínica Dávila (Metropolitan Region, Chile) between 2014 and 2018 (n = 143) by nutritional status.
| Nutritional status | |||||
|---|---|---|---|---|---|
| Demographic and clinical characteristics | Total(n = 143) | Normal weight (n = 88) | Overweight (n = 34) | Obesity (n = 21) | Nutritional status comparisons |
| Length of hospital stay in days, median (min-max) | 4 (2−29) | 4 (2−20) | 4 (2−29) | 5 (2−13) | Kruskal–Wallis;p = 0.29 |
| Days on oxygen, median (min-max) | 3 (0−12) | 2 (0−10) | 3 (0−12) | 3 (0−9) | Kruskal–Wallis;p = 0.31 |
| Days on mechanical ventilation, median (min-max) | 0 (0−23) | 0 (0−9) | 0 (0−23) | 0 (0−7) | Chi-squared test;NW vs. OW p = 0.27;NW vs. Ob p < 0.001;OW vs. Ob p = 0.05 |
| Mechanical ventilation requirement, n (%) | 18 (13) | 6 (8) | 4 (12) | 8 (38) | Chi-squared test;NW vs. OW p = 0.37;NW vs. Ob p < 0.001;OW vs. Ob p = 0.02 |
| Admitted to the intensive care unit, n (%) | 25 (17) | 11 (13) | 5 (15) | 9 (43) | Chi-squared test;NW vs. OW p = 0.75;NW vs. Ob p = 0.001;OW vs. Ob p = 0.02 |
| Viral coinfection, n (%) | 84 (59) | 51 (58) | 23 (68) | 10 (48) | Chi-squared test; p = 0.33 |
| Gender (female = 1), n (%) | 67 (47) | 38 (43) | 20 (59) | 9 (43) | Chi-squared test; p = 0.27 |
| Age (years), median (range) | 4.4 (2−14.5) | 4.4 (2−14.5) | 4 (2.3−12.6) | 6.2 (3−11.6) | Kruskal–Wallis; p = 0.09 |
| Age ranges, n (%) | |||||
| 2−5 years | 103 (72) | 66 (75) | 28 (82) | 9 (43) | Chi-squared test;NW vs. OW p = 0.38;NW vs. Ob p = 0.004;OW vs. Ob p = 0.002 |
| 6−10 years | 35 (24) | 19 (20) | 5 (15) | 11 (52) | Chi-squared test;NW vs. OW p = 0.38;NW vs. Ob p = 0.005;OW vs. Ob p = 0.003 |
| 11−18 years | 5 (3) | 3 (3) | 1 (3) | 1 (5) | Fisher's exact test;p = 0.94 |
| Diagnosis, n (%) | |||||
| Pneumonia | 58 (41) | 33 (38) | 15 (44) | 10 (48) | Chi-squared test;p = 0.76 |
| Bronchitis | 46 (32) | 27 (31) | 14 (41) | 5 (24) | Chi-squared test;p = 0.36 |
| Recurrent obstructive bronchitis | 16 (11) | 7 (8) | 5 (15) | 4 (19) | Chi-squared test;p = 0.26 |
| Febrile syndrome | 9 (6) | 9 (10) | 0 | 0 | Fisher's exact test;p = 0.05 |
| Other | 14 (10) | 12 (14) | 0 | 2 (9) | Fisher's exact test;p = 0.05 |
N, number; NW, normal weight; Ob, obesity; OW, overweight.
A total of 59 children (41%) tested positive for a single respiratory virus, while 84 (59%) tested positive for more than one respiratory virus. Of the viruses that manifested in monoinfection, AdV was the most common (9.8%), followed by parainfluenza virus (7.7%) and RSV (7.0%) (Table 2). Of the samples that showed coinfection, 50 (35%) were positive for two viruses, 31 (20.9%) for three viruses and three (2.1%) for four viruses. RV/EV was the most frequently detected virus in 59 cases (41.3%), followed by AdV in 53 (37%) and RSV in 38 (26.6%), while AdV-RV/EV was the most frequently detected combination (10; 6.9%).
Frequency of virus detection in nasopharyngeal samples in children hospitalised for respiratory infection.
| Virus | n | % |
|---|---|---|
| AdV | 14 | 9.8 |
| PIV | 11 | 7.7 |
| RSV | 10 | 7.0 |
| RV/EV | 9 | 6.3 |
| FluA | 5 | 3.5 |
| HMPV | 4 | 2.8 |
| COV | 2 | 1.4 |
| HBoV | 2 | 1.4 |
| FluB | 2 | 1.4 |
| RV | 0 | 0 |
| EV | 0 | 0 |
| RSV codetected with other viruses | 27 | 18.9 |
| >1 virus other than RSV | 57 | 39.8 |
| Total | 143 | 100 |
AdV, adenovirus; COV, coronavirus; EV, enterovirus; FluA, influenza A; FluB, influenza B; HBoV, human bocavirus; HMPV, human metapneumovirus; PIV, parainfluenza; RSV, respiratory syncytial virus; RV, rhinovirus; RV/EV, rhinovirus/enterovirus.
Severity was found to be associated with nutritional status, adjusted for control variables such as coinfection, age and gender. Specifically, keeping the adjustment variables constant, children with obesity showed a 1.2-fold increase in length of hospital stay (p = 0.04; 95% CI 1.0−1.5), a 1.4-fold increase in days of oxygen therapy (p = 0.03; 95% CI 1.0−1.8) and a 4.4-fold increase in days of mechanical ventilation (p < 0.001; 95% CI 2.7−7.1) than children with normal weight (Table 3). Similarly, the probability of requiring mechanical ventilation and of being admitted to the ICU, expressed in risk ratios (e.g., odds ratio), was 7.7 times (p = 0.001; 95% CI 2.2−26.3) and 5.1 times (p = 0.003; 95% CI 1.7−15.2) higher in children with obesity compared to children with normal weight, respectively. Moreover, while there was no difference between overweight and normal-weight children regarding mechanical ventilation requirement (p = 0.36; 95% CI 0.5−7.3), overweight children who required mechanical ventilation had 3.3 times more days of mechanical ventilation (p < 0.001; 95% CI 2.1−5.2) than normal-weight children. There were no differences in length of hospital stay in days, days of oxygen therapy or admission to the ICU between overweight and normal-weight children (Table 3).
Association between variables of severity and nutritional status among children hospitalised with acute respiratory infections at Clínica Dávila (Metropolitan Region, Chile) between 2014 and 2018.
| Response variables | |||||
|---|---|---|---|---|---|
| Explanatory variables | Days in hospital | Days on oxygen | Days on MV | Requirement for MV | ICU admission |
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Nutritional status | |||||
| OW vs. NW | 1.1(0.9−1.3) | 1.1(0.9−1.4) | 3.3(2.1−5.2)*** | 1.9(0.5−7.3) | 1.2(0.4−3.7) |
| Ob vs. NW | 1.2(1.0−1.5)* | 1.4(1.0−1.8)* | 4.4(2.7−7.1)*** | 7.7(2.2−26.3)** | 5.1(1.7−15.2)** |
| Viral coinfection | 0.9(0.7−1.0)* | 0.9(0.7−1.1) | 0.7(0.5−1.1) | 0.8(0.3−2.6) | 1.4(0.3−2.7) |
| Female | 1.3(1.1−1.5)** | 1.4(1.1−1.7)** | 1.4(0.9−2.0) | 1.2(0.4−3.5) | 1.4(0.5−3.4) |
| Age | 0.9(0.9−1.0) | 0.9(0.9−1.0) | 0.9(0.9−1.1) | 1.1(0.9−1.3) | 1.0(0.9−1.2) |
| Regression | Poisson | Poisson | Poisson | Logistic | Logistic |
95% CI, 95% confidence interval; ICU, intensive care unit; IRR, incidence rate ratio; MV, mechanical ventilation; NW, normal weight; Ob, obesity; OR, odds ratio; OW, overweight.
For Poisson regression models, the cells show the IRR-transformed coefficients and, in parentheses, the 95% CI. In the logistic regression models, the OR and, in parentheses, the 95% CI are reported. The explanatory variable of nutritional status corresponds to a categorical variable (dummy), comparing NW vs. OW and NW vs. Ob. Control variables include viral coinfection (yes = 1), female (yes = 1) and age (in years).
The significance level is indicated as:
Viral coinfection (≥2 viruses) was associated with a shorter hospital stay (incidence rate ratio = 0.9; p = 0.04; 95% CI 0.7−1.0), but was not significantly associated with the other severity variables (Table 3). Comparing the gender of the patients, it was found that girls had 1.3 times more days of hospitalisation (p = 0.001; 95% CI 1.1−1.5) and 1.4 times more days of oxygen therapy (p = 0.003; 95% CI 1.1−1.7) than boys. Age was not associated with any severity variable (Table 3). Lastly, the presence of viral coinfection was not significantly associated with nutritional status (overweight vs. normal weight [odds ratio = 1.1; p = 0.8], obesity vs. normal weight [odds ratio = 0.8, p = 0.7, 95% CI 0.3–2.2]).
DiscussionObesity is a serious global problem. The recent SARS-CoV-2 pandemic has highlighted the importance of obesity in the severity of the clinical course of COVID-19 caused by this virus in both children and adults. Obesity in childhood and adolescence can be considered a risk factor for greater susceptibility to and severity of COVID-19 and is associated with nutritional, cardiac, respiratory, renal and immunological abnormalities, which can exacerbate the complications of SARS-CoV-2 infection.22,26,27
As has been reported, SARS-CoV-2 affected the circulation of other respiratory viruses, which occurred with very low frequency compared to previous years, so few studies have analysed the relationship between overnutrition and infection by other respiratory viruses, especially in the paediatric population.28 A study that included six hospitals in the USA conducted in July and August 2021 with 915 paediatric patients concluded that a higher proportion of patients with COVID-19 in viral coinfection with other viruses required oxygen support compared to those without viral coinfection, with RSV being the main virus detected in coinfection.27
Our study, conducted in hospitalised patients prior to the COVID-19 pandemic, found that obesity and overweight are risk factors for a worse clinical course of respiratory infection due to classical viruses in children hospitalised for acute respiratory infection. In patients with obesity, severity was higher in all the severity variables analysed: greater length of hospital stay, days of oxygen requirement, requirement for and days on mechanical ventilation, and admission to the ICU. These results are consistent with the few previous studies that linked nutritional status with severity of viral respiratory infection in children prior to the current pandemic. Rivera Claros et al.29 studied children under two years of age without chronic disorders who required hospital admission due to RSV infection, concluding that being overweight or obese is associated with requiring more days on oxygen therapy. In turn, Akiyama et al.24 studied a group of minors who required hospitalisation for RSV, including children up to seven years of age, and found that the duration of the RSV infection disease can be prolonged not only in underweight minors but also in minors with obesity. Arias-Bravo et al.16 found that children under six months of age with overnutrition and hospitalised due to viral respiratory infection, not just due to RSV, had a longer hospital stay and required more days of oxygen therapy than infants with normal weight. Furthermore, overnutrition has been linked not only to viruses, but also to bacteria. Arias-Bravo et al. found that children with overnutrition presented with a nasopharyngeal profile characterised by an overrepresentation of pathogenic bacteria and pro-inflammatory cytokines.30 The available data in both humans and mice indicate that a state of excess adiposity greatly increases susceptibility to infection.4 However, the direct and indirect mechanisms responsible for the differences in immune activity and host defence between healthy and obese individuals remain unclear.
On the other hand, our study found no relationship between viral coinfection and respiratory infection severity. Conflicting data have been reported regarding the severity of symptoms in patients infected with a single virus versus coinfected patients. Certain viral combinations appear to present greater disease severity.31,32 A meta-analysis of viral respiratory coinfections in children found that coinfections with RSV or human metapneumovirus are associated with increased risk of ICU admission.33 However, a meta-analysis that included 21 studies of respiratory infections involving 4,280 patients found that viral co-infections did not correlate with worse clinical disease outcomes compared with individual infections.34
It is also interesting to observe that the clinical course is more severe in girls, with longer hospital stay and more days of oxygen therapy. Boys exhibit significant pulmonary differences compared to girls, which predispose them to a higher frequency of respiratory diseases. These differences are primarily based on the fact that female sex hormones are beneficial in promoting lung development and maturation early in life,35 which is related to a greater predisposition to lung diseases in boys. However, in our cohort, girls more frequently suffered from overnutrition than boys (43% vs. 34%), which could explain the greater severity of the disease associated with the female sex in our study.
Although our results are relevant, we recognise that this type of analysis is not exempt from limitations. For example, being a retrospective study, it does not allow us to demonstrate causality or include variables that allow us to control endogeneity in the data set. Similarly, there are omitted variables that could conceal more relevant explanatory factors, such as vaccination against influenza viruses, which, unfortunately, was not reported in more than 38% of the electronic medical records reviewed. Limitations due to omitted variables are common in correlational and retrospective studies, which, for the most part, constitute actual learning only when the study has concluded. Furthermore, we also recognise that the data set may include some measurement errors, for example due to a data set being composed of different winter campaigns, molecular techniques and personnel taking the sample; external factors that are very difficult to control. In addition, different combinations of respiratory viruses can occur because the viral circulation is different every year. These limitations could be addressed by future studies on acute respiratory infections.
Regarding its strengths, we would argue that our study is one of very few to address the relationship between overnutrition in children, viral coinfections and severity of the clinical course. The data present a comparable proportion between girls and boys, as well as reliable and standardised anthropometric records. Highly sensitive and specific molecular techniques were used for the analysis of respiratory samples,36 so the results reflect a true approximation of the types of virus that we can find in these patients. Despite these possible limitations, we would emphasise that there is consistency in that nutritional status is a significant factor in the different indicators of severity, suggesting robust and conclusive associations.
Future research should focus on the study of overnutrition and its role in the severity of viral respiratory infections in children. In order to address the problem more fully, these studies should be jointly conducted by the different medical specialties. In addition, children with overnutrition should be considered a risk group, their priority status should be emphasised, and therefore they should be prioritised with regard to vaccination campaigns.
ConclusionObese and overweight children suffer a more severe clinical course than normal-weight children when they contract respiratory viral infections. Because of this, encouraging the use of available vaccines against respiratory viruses in children suffering from overnutrition is recommended. On the other hand, no relationship was found between overnutrition and the presence of respiratory viral coinfection. Considering the high rates of childhood obesity worldwide and the significant possibility of future new pandemics, it is essential to study the relationship between nutritional status, viral coinfection and severity of infection in children.
FundingWe appreciate the support of the Vice-Rector for Research and Postgraduate Studies, Universidad Autónoma de Chile, funding number DIUA 168-2019, Sociedad Chilena de Nutrición [Chilean Society of Nutrition] SOCHINUT-Tetra Pak 2020 and DICYT 032075ZR, Vice-Rector for Research, Development and Innovation, Universidad de Santiago de Chile.
Conflicts of interestThe authors declare that they have no conflicts of interest.