Almeria is a region in southeast Spain with optimal sunlight levels, along with low pluvial and pollution rates. If exposure to sunlight is sufficient to maintain adequate levels of vitamin D (25OHD), this population should display high serum levels.
ObjectivesTo describe 25OHD serum status in women from Almeria and evaluate the impact of long sunlight exposure along the seasons on 25OHD.
MethodsCross-sectional study, performed in women consecutively recruited from an outpatient rheumatology clinic. Serum levels of 25OHD were assessed in all patients and evaluated according to age (<48 yrs, 48–53 yrs, 54–60 yrs and >60 yrs), season, and presence or absence of menopause. Clinical and laboratory variables that could affect status of vitamin D were also considered.
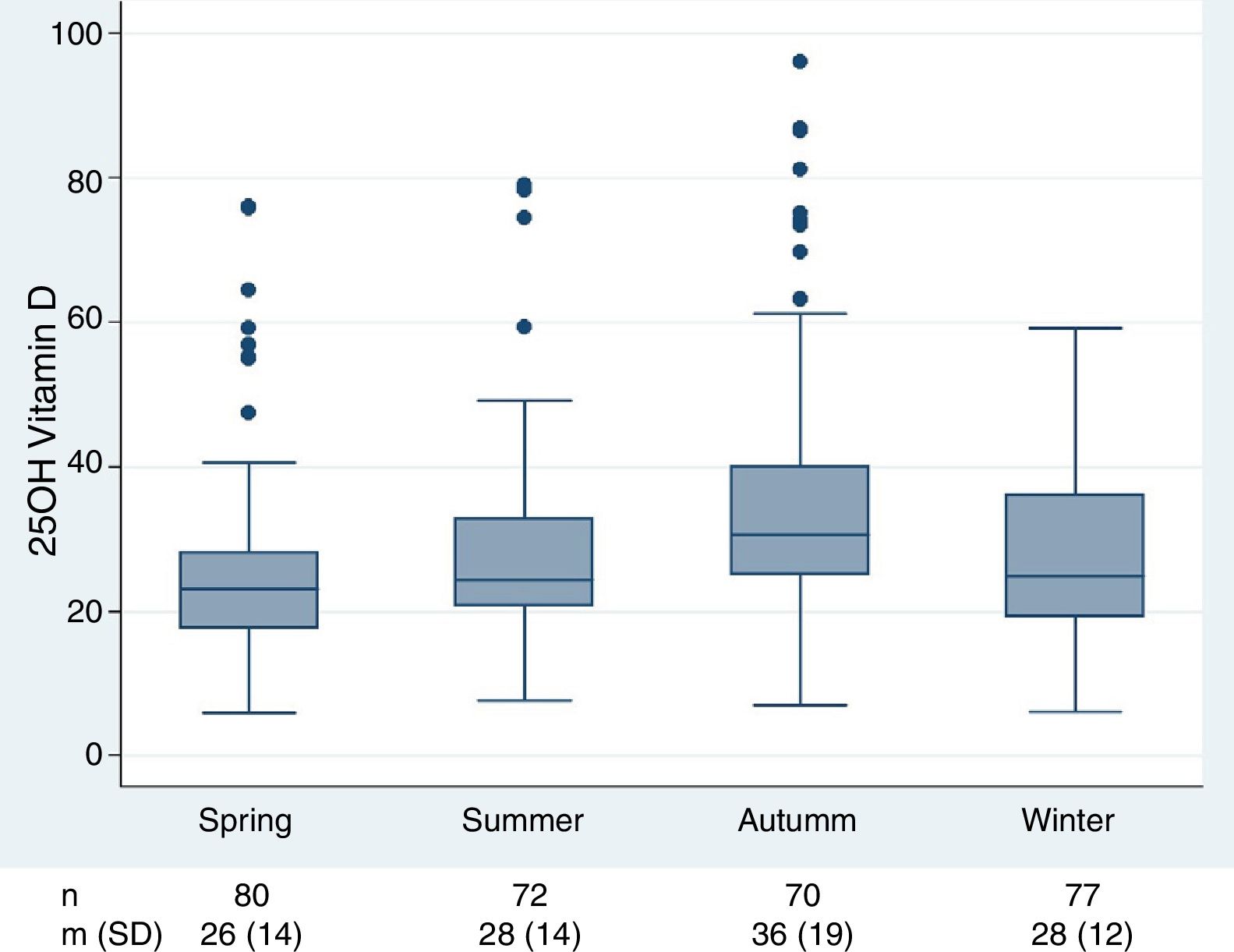
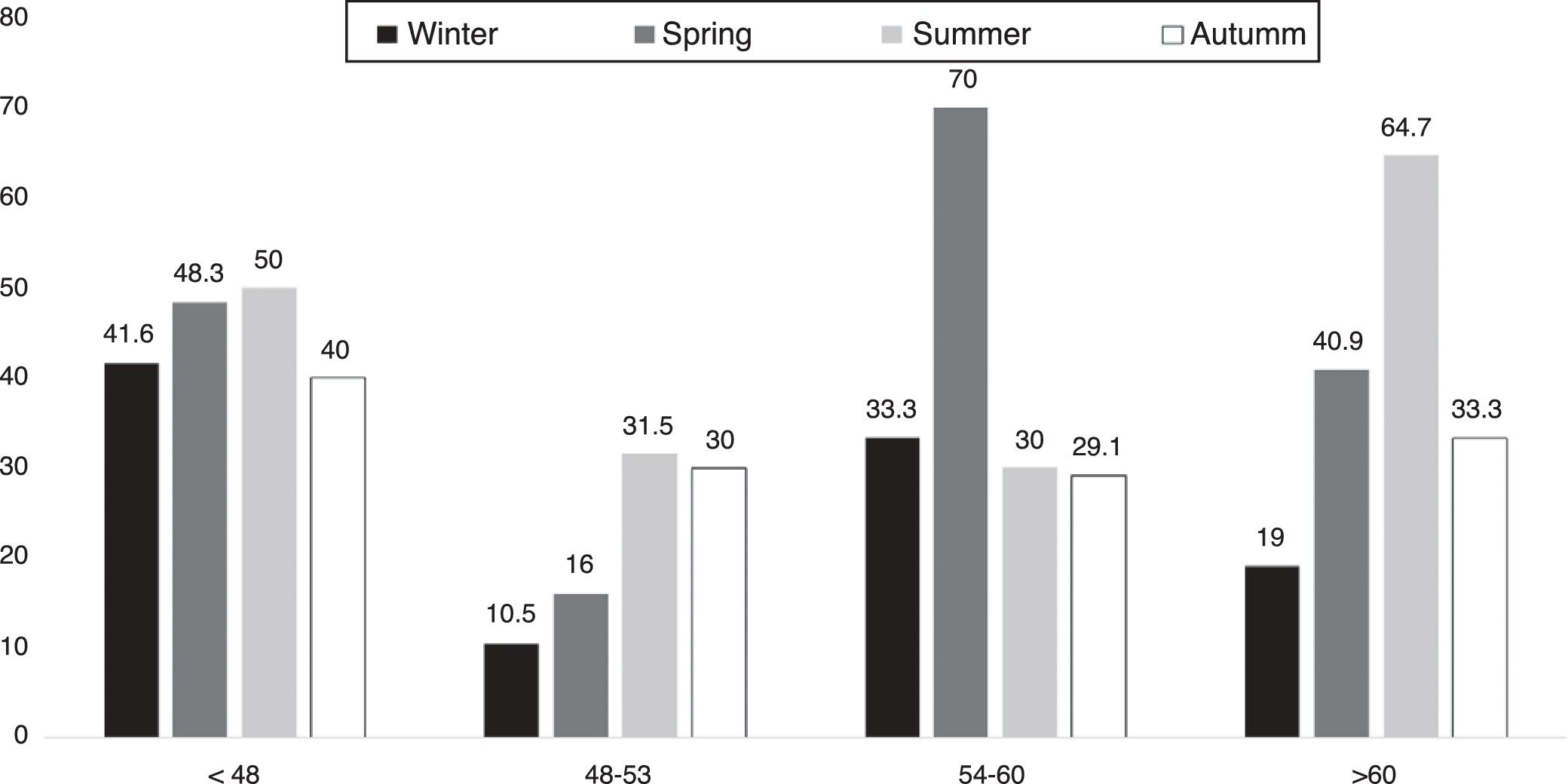
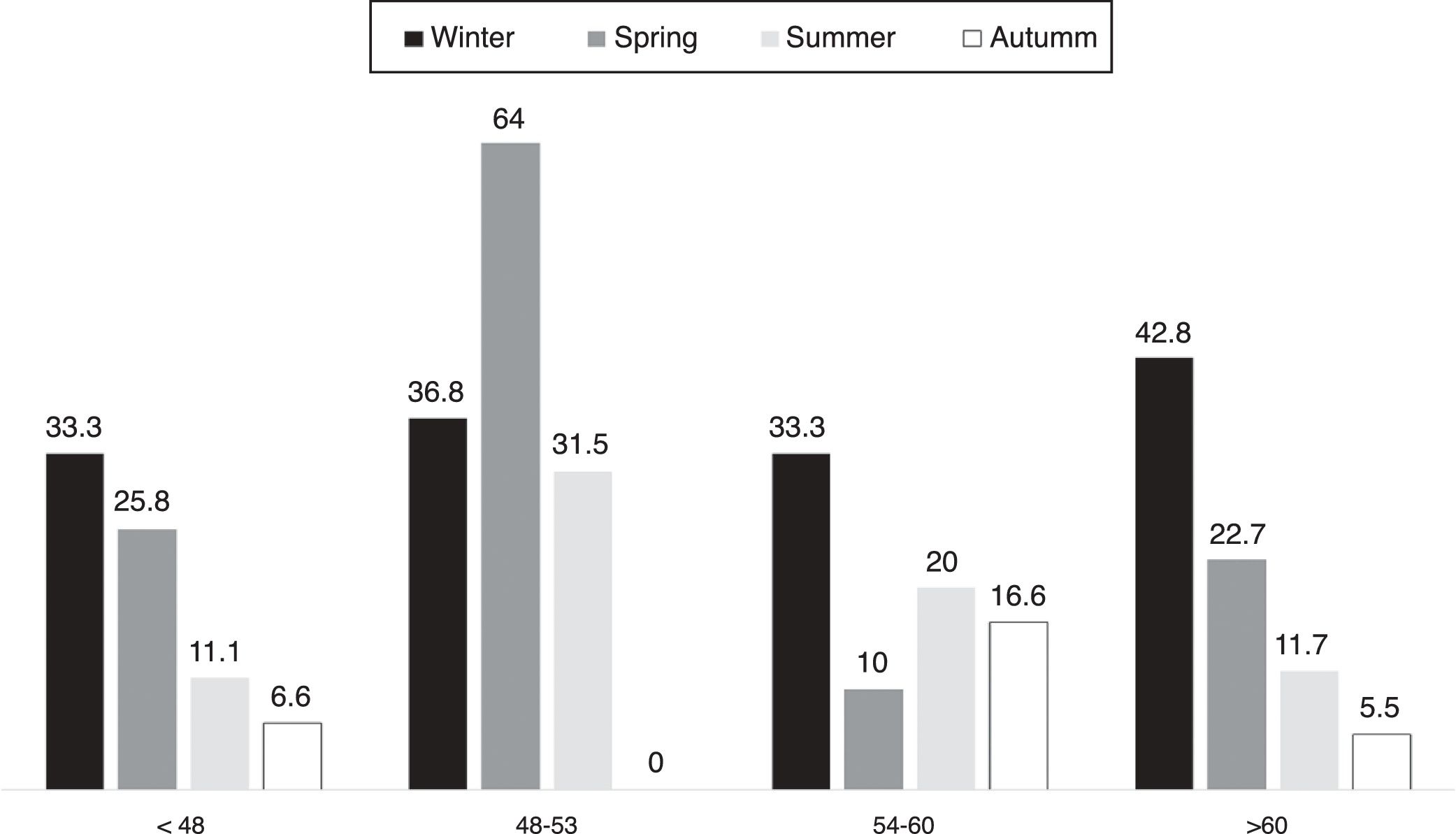
ResultsThe sample included 319 Caucasian female patients. Mean 25OHD were 30.2ng/ml with 195 (61.1%) exhibiting 25OHD inadequate serum levels. Season had a significant effect on 25OHD levels, with autumn being the season in which 25OHD serum levels remained well above 30ng/ml in all age bands, and winter the season with more levels of insufficiency. Menopause did not modify 25OH serum levels. Women whose age was below 48 and over 60 had inadequate levels of 25OHD during summer.
ConclusionsOptimal levels of sunlight could not overcome the problem of inadequate 25OHD serum levels, particularly in elderly and young female population. Vitamin D supplementation may be recommended predominantly in winter and summer in this population.
Almería es una región del sureste de España con un grado óptimo de luz solar, junto con bajas tasas de contaminación y lluvia. Si la exposición a la luz solar es suficiente para mantener niveles adecuados de vitamina D (25OHD), esta población debería presentar concentraciones séricas altas.
ObjetivosDescribir los valores séricos de 25OHD en mujeres de Almería y evaluar el efecto de la exposición prolongada a la luz solar sobre la 25OHD a lo largo de las distintas estaciones.
MétodosEstudio transversal en mujeres reclutadas consecutivamente en una consulta externa de reumatología. Se determinaron las concentraciones séricas de 25OHD en todas las pacientes y se valoraron en función de la edad (< 48 años, 48-53 años, 54-60 años y > 60 años), la estación y la presencia o ausencia de menopausia. También se tuvieron en cuenta las variables clínicas y analíticas que pudieran afectar al estado de la vitamina D.
ResultadosLa muestra incluyó 319 mujeres de raza blanca. El valor medio de 25OHD fue de 30,2 ng/ml, y 195 (61,1%) mostraron concentraciones séricas inadecuadas de 25OHD. La estación tenía un efecto importante en las concentraciones de 25OHD, y el otoño era la estación en la que los valores séricos de 25OHD se mantenían bastante por encima de 30 ng/ml en todas las franjas de edad, y el invierno la estación con más grado de insuficiencia. La menopausia no modificaba las concentraciones séricas de 25OH. Las mujeres menores de 48 años y mayores de 60 años tenían niveles insuficientes de 25OHD durante el verano.
ConclusiónLa luz solar óptima no podía superar el problema de la insuficiencia de las concentraciones séricas de 25OHD, sobre todo en las poblaciones de mujeres mayores y jóvenes. Pueden recomendarse suplementos de vitamina D predominantemente en invierno y en verano en esta población.
Insufficient exposure to sunlight is a worldwide known cause of vitamin D deficiency.1 Essentially, the chief determinant of circulating vitamin D levels is the total amount of sunlight exposure absorbed by the skin, following solar ultraviolet radiation (UVR).2 Besides, numerous investigations suggest that individual differences together with geographical and seasonal variances exert a critical influence on vitamin D status.3
Evidence of vitamin D beneficial effect on reducing the risk of different adverse health outcomes has been increasingly growing in the past years. Predominantly, there is data on bone health,4,5 cancer,6 autoimmune,7 cardiovascular diseases8 and recently in respiratory tract infections.9 So far, the best marker of vitamin D status is circulating 25OHD concentration; though, there is no formal consensus on the optimal 25OHD serum values10 and besides, what constitutes vitamin D deficiency is still troublesome.11
Almeria is a Spanish province, located in the extreme southeast of the country, receiving a mean well above the 240h of sunlight per month, ranging from 176 to 336h per year.12 The region accumulates the highest amount of hours of daylight both in Spain, and in most European countries. The aim of our study, according to Almeria advantageous location, was to make out 25OHD serum status in a population with distinct rheumatic conditions according to age and season, to identify subgroups at risk of vitamin D deficiency, and evaluate the impact of long sunlight exposure in vitamin D sufficiency.
Patients and methodsStudy design and study populationThis was a cross sectional study conducted between September 2008 and August 2014 in an outpatient rheumatology clinic in Almería province (located 36.5° latitude N, 2° LW).
This geographical location benefits from optimal annual sunshine levels,12 good air quality (particulate matter: 10 and real time quality index (AQI)<5; plus a very low precipitation rate (around 9, 4mm/year).13 Patients eligible for the study were women older than 18 years, able to walk, unaided, and not living in care institutions. Menopausal status was defined as when menstruation has failed to occur over a 12 month period while women whose status was uncertain and who replied that they had an unsettled menopause were classified as premenopausal.
Exclusion criteria comprised inflammatory rheumatic diseases, kidney, hepatic or bowel diseases, corticosteroid (oral or inhaled), and or vitamin D therapy. In order to capture information from several seasons and years, two days per week, patients attending this clinic were invited to take part. These were informed about the study and those who consent were included.
The ethics committee of Hospital Mediterraneo approved the study protocol.
MeasurementsBlood samples were taken after an eight-hour fast. Vitamin D measurements were performed with ADVIA Centaur XP Vitamin D Total assay (Siemens Healthcare diagnostics) in external labs, obtaining hydroxylated form, 25OHD values were considered deficient (<20ng/ml), insufficient (>20 and <30ng/ml) and sufficient (≥30ng/ml).14 Calcium, phosphorous, creatinine, albumin, intact parathyroid hormone (PTH) serum levels were also determined. The date of collection was recorded. Seasons were divided according to standards in the northern hemisphere, winter spanning from December 22 to March 20, spring from March 21 to June 20, summer from June 21 to September 22 and fall from September 23 to December 21.
Daylight for the date of the 25OHD sample was obtained from the European weather website (http://www.climatedata.eu),12 and real time air quality index from (http://www.aqicn.org).13
Statistical analysisPatients were described according to the distribution of variables with summary statistics. Student's t test and analysis of variance were used to test hypotheses concerning different distributions by groups. Correlations between continuous variables were tested with the Pearson coefficient. Data were analyzed using Medcalc statistical software version 9.3.8.0 for Windows, with a confident interval of 95% and a significance level lower than 5% (p<0.05).
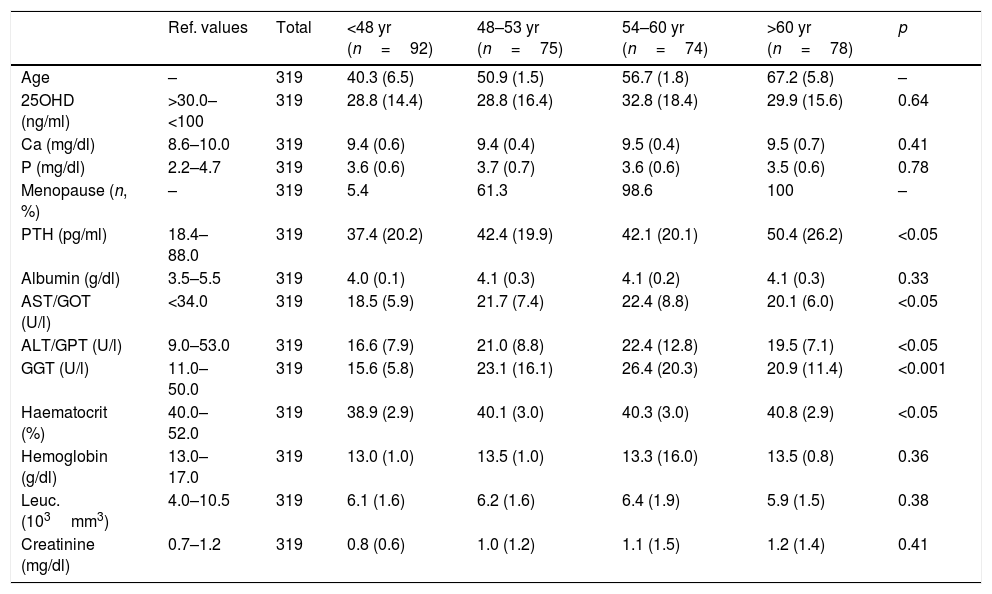
ResultsThe study sample included 319 women, whose mean age was 53.2 (SD 11.1; range 18–81) all Caucasian. Two hundred and sixty women (81, 5%) were postmenopausal. The main diagnosis reported at the time of recruitment were fibromyalgia, osteoarthritis, osteoporosis/osteopenia, back pain, tendinitis, bursitis, shoulder impidgement and polyarthralgia (87%). Yet, major prevalent comorbidities were hypertension, followed by dyslipidaemia and dysthymia (20%, 8% and 12% respectively). Medications most frequently employed were antihypertensives and anxiolytics. Table 1 includes a description of the sample, total and by age groups. The mean 25OHD values were 30.2g/ml (SD 16.2; range 6.0–96.1), with 80 (25.1%) samples considered deficient in vitamin D, 112 (35.1%) insufficient, and 127 (39.8%) sufficient.
Characteristics of the women included, total and by age bands.
| Ref. values | Total | <48 yr (n=92) | 48–53 yr (n=75) | 54–60 yr (n=74) | >60 yr (n=78) | p | |
|---|---|---|---|---|---|---|---|
| Age | – | 319 | 40.3 (6.5) | 50.9 (1.5) | 56.7 (1.8) | 67.2 (5.8) | – |
| 25OHD (ng/ml) | >30.0–<100 | 319 | 28.8 (14.4) | 28.8 (16.4) | 32.8 (18.4) | 29.9 (15.6) | 0.64 |
| Ca (mg/dl) | 8.6–10.0 | 319 | 9.4 (0.6) | 9.4 (0.4) | 9.5 (0.4) | 9.5 (0.7) | 0.41 |
| P (mg/dl) | 2.2–4.7 | 319 | 3.6 (0.6) | 3.7 (0.7) | 3.6 (0.6) | 3.5 (0.6) | 0.78 |
| Menopause (n, %) | – | 319 | 5.4 | 61.3 | 98.6 | 100 | – |
| PTH (pg/ml) | 18.4–88.0 | 319 | 37.4 (20.2) | 42.4 (19.9) | 42.1 (20.1) | 50.4 (26.2) | <0.05 |
| Albumin (g/dl) | 3.5–5.5 | 319 | 4.0 (0.1) | 4.1 (0.3) | 4.1 (0.2) | 4.1 (0.3) | 0.33 |
| AST/GOT (U/l) | <34.0 | 319 | 18.5 (5.9) | 21.7 (7.4) | 22.4 (8.8) | 20.1 (6.0) | <0.05 |
| ALT/GPT (U/l) | 9.0–53.0 | 319 | 16.6 (7.9) | 21.0 (8.8) | 22.4 (12.8) | 19.5 (7.1) | <0.05 |
| GGT (U/l) | 11.0–50.0 | 319 | 15.6 (5.8) | 23.1 (16.1) | 26.4 (20.3) | 20.9 (11.4) | <0.001 |
| Haematocrit (%) | 40.0–52.0 | 319 | 38.9 (2.9) | 40.1 (3.0) | 40.3 (3.0) | 40.8 (2.9) | <0.05 |
| Hemoglobin (g/dl) | 13.0–17.0 | 319 | 13.0 (1.0) | 13.5 (1.0) | 13.3 (16.0) | 13.5 (0.8) | 0.36 |
| Leuc. (103mm3) | 4.0–10.5 | 319 | 6.1 (1.6) | 6.2 (1.6) | 6.4 (1.9) | 5.9 (1.5) | 0.38 |
| Creatinine (mg/dl) | 0.7–1.2 | 319 | 0.8 (0.6) | 1.0 (1.2) | 1.1 (1.5) | 1.2 (1.4) | 0.41 |
Abbreviations: Ca, calcium; P, phosphorous; PTH, parathyroid hormone; AST/GOT, aspartate aminotransferase; ALT/GPT, alanine aminotransferase; GGT, gamma-glutamyl transpeptidase; Leuc, leucocytes, ng/ml, nanogram per mililitre; mg/dl, milligrams per decilitre; pg/ml, picogram per mililitre; g/dl, grams per decilitre; mm3, cubic milimeter; Ref. values, reference values.
All values are expressed as mean (SD) unless otherwise noted.
The evaluation of laboratory variables that could hamper with 25OHD status revealed no significant difference in hemoglobin, leukocytes, albumin, calcium, and phosphorus between age groups. PTH values were significantly higher in women above 60 years old compared to the other groups and hematocrit significantly lower in the youngest group (see Table 1).
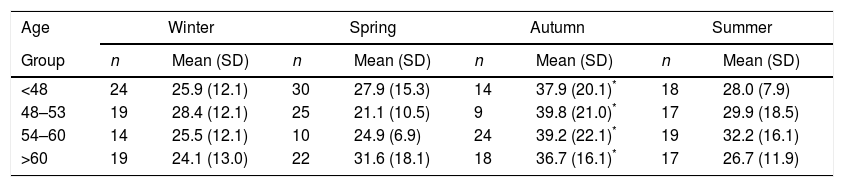
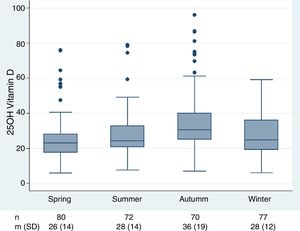
Season was associated to the level of serum 25OHD (p<0.001), with autumn being the only season in which highest levels of 25OHD serum levels were found (mean 36.8ng/ml; SD=19.8) (Fig. 1) with mean levels above 30ng/ml in all bands. Conversely, the lowest mean 25OHD concentrations were found in winter, in all groups (Fig. 1, Table 2). All age groups exhibited mean 25OHD serum levels<30ng/ml in summer, except for cohort between 54 and 60 years, but the difference between groups was not statistically significant. 25OHD serum levels followed normal distribution.
Mean serum levels of vitamin D (ng/ml) by age bands and season.
| Age | Winter | Spring | Autumn | Summer | ||||
|---|---|---|---|---|---|---|---|---|
| Group | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | n | Mean (SD) |
| <48 | 24 | 25.9 (12.1) | 30 | 27.9 (15.3) | 14 | 37.9 (20.1)* | 18 | 28.0 (7.9) |
| 48–53 | 19 | 28.4 (12.1) | 25 | 21.1 (10.5) | 9 | 39.8 (21.0)* | 17 | 29.9 (18.5) |
| 54–60 | 14 | 25.5 (12.1) | 10 | 24.9 (6.9) | 24 | 39.2 (22.1)* | 19 | 32.2 (16.1) |
| >60 | 19 | 24.1 (13.0) | 22 | 31.6 (18.1) | 18 | 36.7 (16.1)* | 17 | 26.7 (11.9) |
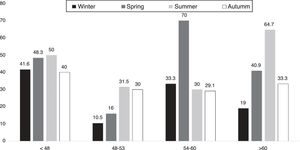
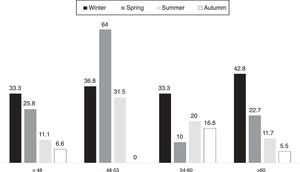
Figs. 2 and 3 display the percentage of patients reaching inadequate levels according to mean serum values of 25OHD, season and age bands. More than 40% of the patients younger than 48 years had vitamin D levels under the level of insufficiency in all seasons.
The presence or absence of menopause did not make difference in 25OHD serum levels. Though significantly older, the menopause group exhibited a clear correlation between age and PTH levels (correlation coefficient r, p=0.036).
DiscussionWe have shown that two thirds of a sample of women in a sunny region are below sufficient levels of vitamin D. In point of fact, the hypothesized proper exposure to sunlight capacity to sustain adequate serum levels of vitamin D in female population appears not to be fully acceptable in view of the present results. Yet, previous research have drawn attention to sunlight exposure (UVR) as a critical step in vitamin D synthesis.3 In addition to the number of sunlight hours, factors like latitude, season and time of the day, exert an important influence on UVR effectivity.15 Yet, regions above 37° latitude N during winter result in very little if any vitamin D3 produced in the skin, while below 37° N more vitamin D3 synthesis occurs throughout the year.1 Despite the fact of Almeria's adequate location and optimum level of sunshine throughout the year (Fig. 1), insufficient 25OHD serum levels prevailed both in winter and spring in middle-aged and elderly women. In this line, studies carried out in similar latitudes16–18 at both sides of the equator achieved comparable seasonal upshots. For example, early studies performed in Buenos Aires, Argentina (latitude 34° S), reported a prevalence of vitamin D deficiency of up to 65% among ambulatory postmenopausal women during wintertime.19 While in Geelong region, Australia (latitude 38° N) vitamin D insufficiency reached 38% in a female population under 60.16 Season is known to be associated with ambient ultraviolet radiation, reaching its peak in summer and minimum in winter. In this respect, Almeria is outstanding, as the annual average hours of sunshine can reach 247.6h, and 196.5h throughout winter.12 Conversely, cities in northern latitudes like Copenhagen (55.6° N) or London (51.5° N) are not exposed to more than 72.3h of sunshine in winter.12 Even so, an optimal level of sunshine throughout the year, does not guarantee acceptable levels of 25OHD as shown in our study. Perhaps, changes in outdoor behavior and increased clothing worn, together with decreased time spent outdoor mainly in both seasons, could explain in part these results.16 On the other hand, autumn is the season in which 25OHD reached optimal serum levels in all ages. This finding is in full agreement with various other works, placing 25OHD annual peak in autumn and nadir in winter-spring.20,21
These percentages of deficiency in our study were even higher than expected. In this regard Rodriguez Sangrador et al., 22 drew attention to the fact that more than 50% of women patients in his trial avoided exposing to sunlight in summer. Similar results were displayed in studies located in Brazil,23 Iran24 and also in an interesting paper by Al-Daghri et al., in Saudi Arabia.25 Regardless of the fact that these regions are well below 37° latitude S and N respectively, summer months present very high temperatures (>40°C at noon) increasing risk of heat strokes. In this line, Almeria, also achieve high temperatures in summer (well >30°C), possibly preventing patients >60 years in particular from exposing to sunlight, and therefore reducing outdoors activities. This is something to take into account, as summer has been traditionally defined as the season were Caucasians and some other skin types can make optimal vitamin D3.26,27 Concerning younger population, unacceptable high insufficient levels, reaching >50%, extended to female patients below 48 and above 60 years old in the present study. Indeed, most trials describe the expected decrease in 25OHD during winter in young population, particularly in northern latitudes.28,29 In this respect, Trangpricha et al. revealed that the prevalence of vitamin D deficiency increased from 3 to 30% between summer and winter in young healthy adults aged 18–29 years.30 However, Gagnon et al., concluded that about a third of women of childbearing age have suboptimal serum 25OHD levels during summer.28 Also, Gonzalez-Padilla et al., revealed that almost 2/3 of young healthy medicine students at University of Las Palmas of Gran Canarias Islands (28 N), had mean levels of 25OHD <30ng/ml. Apart from reasons others than avoiding sunlight exposure and time spent indoors during summer, the use of sunscreen in all ages could exert additional influence in reducing 25OHD serum levels,31 though this is still controversial.32,33
We found that menopause did not exert particular influence on 25OHD serum levels along seasons. In contrast, previous reports suggest the prevalence of inadequate vitamin D levels in post-menopausal women, particularly in those with osteoporosis and history of fractures in northern latitudes.34 Also, vitamin D deficiency was corroborated during menopause in studies performed in South America, despite their location at latitudes with abundant sunlight.35
This study identified patients >60 years as being at higher risk of inadequate vitamin D serum levels (both insufficiency and deficiency). However, low 25OHD serum levels were also observed in the other age bands. These inadequacies extended not only to the winter-spring seasons, but also to summer period particularly in the eldest group. The decreased vitamin D status of elderly persons is well known, with numerous factors implicated including lack of dietary consumption, malabsorption, and what is most important, a reduction in 7-dehydrocholesterol (7-DHC) in the skin.36 7-DHC is a chemical precursor required for vitamin D synthesis, which decrease by nearly half from a 21-year-old to an 88-year-old.15 However, the youngest group exhibited almost 60% insufficient 25OHD serum levels in winter, spring and 50% in summer, while deficient levels were not significant in this group.
The main strengths of our study include its large sample size and low frequency of missing data.
However, some limitations are worth noting. To begin with, all women included in the study were Caucasian, corresponding to skin photo type III–IV according to Fitzpatrick classification.37 Therefore caution should be applied when extrapolating these results to the general population. Another limitation was the fact that body mass index was not included in clinical records. As Vitamin D3 is fat-soluble and store in body fat, we could have missed the magnitude of overweight subjects with vitamin D deficiency. Finally, we could not perform a detailed evaluation of vitamin D taken from the diet and obtain accurate data about the quantity of sun exposure.
Another interesting point regards to the variety of assays used to measure 25OHD.38 Chemiluminescence immunoassay employed in this trial show acceptable correlation with the goal standard liquid chromatography-tandem mass spectrometry.39 Still, immunoassays intermethod variability exist,40 thus standardization of vitamin D assays and consideration of assay-specific decision limits should be addressed.
In all cases, patients with either deficiency or insufficiency of vitamin D, were supplemented with oral calcifediol according to 25OHD serum levels and independently of the season.
Several clinical conclusions could be drawn from this study despite the aforementioned limitations. In first place, though the abundant sunlight throughout the year and optimal location of the study, insufficient 25OHD serum levels was commonly observed in winter and spring while autumn exhibited optimal levels in all population groups. Secondly, female elderly patients >60 yrs but also those >48 yrs were at higher risk of inadequate 25OHD serum levels during those seasons and therefore should need surveillance. Thirdly, summer exhibited high percentage of patients with 25OHD insufficient levels in all groups, which should enhance vitamin D measurements and possibly the need of supplementation during this period. In the present study, optimal levels of sunlight did not overcome the problem of inadequate 25OHD serum levels. For all these reasons, we reinforce performing 25OHD serum measurements in elderly rheumatic female population, independently of the season. Vitamin D supplementation may be recommended predominantly in winter but also in summer might be required.
Conflicts of interestNone of the authors declares conflict of interest.
The authors are grateful to Mrs. Mercedes Guerra, manager of documents and archives of the Spanish Rheumatology Society (SER) Research Unit, for her assistance in the reference strategy performance and in obtaining the articles, and to Dr Loreto Carmona for helping with the figures and checking the manuscript. This study has no financial support.