Unhealthy lifestyle and inadequate diet could influence the development of future cardiometabolic disease. The main aim of this study was to determine the association between aerobic fitness and cardiometabolic risk factors in adults, whether this relation is depends of adherence to Mediterranean diet (MD). A secondary aim was to study the combined effect of aerobic capacity and adherence to MD on global cardiometabolic risk score (CMRS).
MethodA total of 79 adults (38% women) enrolled between 18–40 year from Cádiz. We measured adiposity indicators, blood pressure, triglycerides, glucose and inflammatory profile (interleukin-6 and tumor necrosis factor) and was computed (CMRS). Aerobic fitness was measured by maximal oxygen comsuption through an incremental stress test by cycleergometer. The MD patterns was measured using the questionnaire of adherence to MD. The association between aerobic fitness and cardiometabolic risk factors was examined using a lineal regression and it was adjusted for different confounders. CMRS on the lifestyle was analyzed using the ANOVA test, with statistical significance level of p<0.05 in Bonferroni.
ResultsLinear regression showed inverse association between aerobic fitness and cardiometabolic risk factors (all p≤0.05) in the model without adjustment. Blood pressure and triglycerides lost the association after adjust model for sex, age, and adherence to MD. Participants with high aerobic fitness and high adherence to MD show a lowest CMRS (−1.083±2.325 vs. 2.802±1.759).
ConclusionsAerobic fitness was inversely associated with fatness risk factors, that relationship is independent to adherence to MD. A high adherence to MD could modulate blood pressure. A combination of high aerobic capacity and high adherence to MD could reduce the adverse consecuence of a low adherencie to MD.
Un estilo de vida poco activo y una dieta inadecuada podrían influir en el desarrollo de futuras enfermedades cardiometabólicas. El objetivo principal fue determinar la asociación entre capacidad aeróbica y factores de riesgo cardiometabólicos y si dicha posible asociación es independiente de la dieta mediterránea (DM). A su vez, se plantea como objetivo secundario estudiar el efecto combinado de la capacidad aeróbica y la adherencia a la DM sobre el índice de riesgo cardiometabólico global (IRCM) en adultos.
MétodosSe evaluó a 79 adultos (38% mujeres) entre 18 y 40 años en Cádiz. Se midieron indicadores de adiposidad, presión arterial, triglicéridos, glucosa y perfil inflamatorio (interleucina-6 y factor de necrosis tumoral) y se desarrolló un IRCM. Se midió la capacidad aeróbica mediante el consumo máximo de oxígeno a través de una prueba de esfuerzo incremental en cicloergómetro. La adherencia a la DM se evaluó mediante cuestionario. Se utilizó un modelo de regresión lineal para estudiar la asociación entre capacidad aeróbica y factores de riesgo cardiometabólicos con diferentes modelos de ajuste. Se analizó el efecto combinado de la capacidad aeróbica y la adherencia a la DM sobre el IRCM mediante el test de ANOVA, con nivel de significación de p<0,05 en Bonferroni.
ResultadosSe observó asociación negativa entre la capacidad aeróbica y los factores de riesgo cardiometabólicos (todas p≤0,05) en el modelo sin ajustar. La presión arterial y los triglicéridos perdieron la asociación tras ajustar el modelo por sexo, edad y adherencia a la DM. Los participantes con alta capacidad aeróbica y alta adherencia a la DM mostraron un menor IRCM (−1,083±2,325 vs. 2,802±1,759).
ConclusionesLa capacidad aeróbica se asocia de forma inversa con factores de riesgo cardiometabólicos relacionados con la adiposidad, independientemente de la adherencia a la DM. Una alta adherencia a la DM podría influir en la modulación de la presión arterial. Una alta capacidad aeróbica podría reducir las consecuencias adversas de una baja adherencia a la DM.
Cardiovascular diseases are an epidemic and will be the leading cause of death by 2030.1 The modifiable risk factors include hypertension, hyperlipidemia, overweight, hyperglycemia, smoking and stress.2 Elevated inflammatory marker levels are currently also included among these risk factors.3 An indolent lifestyle and inadequate diet appear to play a key role in the development of these non-transmissible diseases.4
Physically active people have a lower risk of developing disorders such as obesity, diabetes or cancer, among other conditions.5 High physical activity levels could positively influence aerobic capacity or fitness,6 which along with a healthy diet is related to improved health.7 Previous studies have shown high aerobic fitness to be inversely associated with indicators of central and total obesity,8 blood pressure, insulin resistance and lipid profile in both adults9 and young people,10 and it is correlated to a lesser risk of cardiometabolic diseases.11
In addition, the Mediterranean diet (MD)12,13 is regarded as a protective factor against the onset and development of cardiovascular disease.14 The MD has been associated with benefits in terms of the control of diabetes and obesity,15 as well as improvements in blood pressure, lipid profile and inflammatory markers, and contributes to a reduction of the atherogenic process.16 It is characterized by a high consumption of olive oil, fruit, vegetables, legumes, nuts and unrefined grains; a moderate consumption of fish, white meat, fat-free dairy products and wine (mainly with meals); and a low consumption of red meat and processed foods.15
Most studies have analyzed the effect of aerobic fitness or the inclusion of the MD upon cardiovascular or metabolic risk factors considered separately, but not the combined effect of both. Likewise, no studies have been made to determine whether the potential association between aerobic fitness and cardiometabolic risk factors is independent of adherence to the MD or not. It is also of interest to analyze each of these risk factors individually and on a global basis, since they may be influenced differently by aerobic fitness or diet.
Thus, the primary objective of this study was to determine the association between aerobic fitness and cardiometabolic risk factors (considered individually and globally), and to establish whether this possible association is independent or not of inclusion of the MD. A secondary objective of the study was to analyze the combined impact of aerobic fitness and adherence to the MD upon global cardiometabolic risk in the adult population.
MethodDesignThis study comprises a subsample forming part of the cross-sectional study of the NUTAF project (Study of nutritional habits and physical activity level in adults), designed to assess the nutritional habits, physical activity level and fitness, as well as health parameters (e.g., body composition, lipid profile, inflammatory markers or blood pressure, among others) in a cohort of adults between 18–40 years of age in the province of Cádiz (Spain). Data collection took place from January 2016 to June 2017. The study was approved by the Research Ethics Committee of Cádiz (Hospital Puerta del Mar), and followed the recommendations of the Declaration of Helsinki for human studies (1964; revision of Fortaleza, Brazil, 2013). All participants were informed about the purpose of the study, the tests and potential risks, and signed an express consent document. Cross-sectional, non-probabilistic study designs pose limitations in terms of representativeness and external validity regarding the population. Nevertheless, many variables and associated factors are collected, and an estimate of health condition and magnitude can be made, because the size and variety of the sample is considerable, thus bringing it close to reflecting the epidemiological characteristics of society in terms of both gender and the presence of overweight/obesity.
ParticipantsThe NUTAF study cohort consisted of 150 volunteers. Of these, we selected 79 participants (31 women) that met the inclusion criteria and had valid data regarding the body mass index (BMI), waist circumference (WC), percentage body fat, blood pressure, plasma triglycerides, plasma glucose, inflammatory profile (interleukin-6 [IL-6] and tumor necrosis factor-alpha [TNF-α]), aerobic capacity or fitness, and adherence to the MD.
The inclusion criteria were as follows: (1) no dieting, with the preservation of a stable body weight over the previous 6 months; (2) no current or past illness or injury capable of affecting the outcomes; (3) no diagnosed arterial hypertension; (4) no smoking; and (5) age 18–40 years.
Anthropometric characteristicsAnthropometric measurements were obtained with the participants wearing no shoes and only light clothing. Body height was measured in the standing position using a stadiometer (SECA 225; range, 60–200cm, precision 1mm). Waist circumference measurements were taken at the midpoint between the lower margin of the last palpable rib and the upper part of the iliac crest, using a non-elastic measuring tape (SEAS 200; range 0–150cm, precision 1mm), based on a standardized protocol.16 The body mass index was calculated by dividing weight (kg) by height squared (m2). Percentage body fat and weight were recorded using a bioimpedance system (Tanita MC-780MA 8-electrode multifrequency model; Tanita Corp., Tokyo, Japan), following the standardized protocol.17,18 The measurements were obtained after a fasting period of at least 8h, the participants having avoided alcohol, caffeine and physical activity during the previous 24h.
Blood pressureBlood pressure was measured three times (early in the morning) on the left arm using an Omron M3 Intellisense digital device (Omron, Kyoto, Japan) previously validated according to the international protocol of the European Society of Hypertension.19 Appropriate cuff sizes were used, and the measurements were made while the participants were sitting and resting, with a pausing interval of several minutes between measurements. We calculated the mean blood pressure (MBP), which reflects the average arterial pressure during a single cardiac cycle, with the incorporation of the systolic (SBP) and diastolic blood pressure (DBP) phases (mmHg). Thereadings were obtained, and the mean value was reported. Mean blood pressure was calculated as: MBP=DBP+(SBP-DBP)/3.20
BiochemistryFasting blood samples (8:00a.m.) were collected by vein puncture. The samples were stored in EDTA-anticoagulated Vacutainer tubes and Vacutainer tubes with gel in the absence of anticoagulant, centrifuged for plasma and serum separation, respectively, and finally stored at −80°C until analysis. At the time of analysis, the samples were thawed in ice and then pipetted in 10μl duplicates onto microplates with 200μ- of specific reagent of each commercial kit. All the plates were spiked with standard curves of known concentrations of each parameter for subsequent absorbance data identification. Analysis was made following the instructions of the manufacturer (Spinreact, S.A., Sant Esteve d’en Bas, Girona, Spain); by adapting the measurements to 96-well microplates, the metabolic parameters analyzed in plasma included blood glucose (Glucose-HK Ref. 1001200) and triglycerides (TAG: Ref. 1001311). The microplates were then placed in a microplate reader (PowerWave™ 340, BIO-TEK), and the absorbance readings were processed with the KC junior™ application from BIO-TEK.
The Bio-plex manager 6.1 application from Bio-Radwas was used to analyze the expressed cytokines.
Aerobic fitnessAerobic fitness was objectively assessed using an incremental exercise test with a cycle ergometer (Lode Excalibur, The Netherlands). The Jaeger MasterScreen CPX® gas analyzer (CareFusion, San Diego, CA, USA) was used. The protocol employed was an adaptation of that validated by Achten et al.21 The test was performed with a load of 30 watts (W), with 30W increments every three minutes until the respiratory ratio reached a stable value of 1 or more.22 After the test, a resting period of 5min was allowed, and the maximum oxygen consumption test (VO2max) was performed again with the cycle ergometer, with 30W increments every minute until exhaustion, at a rate of 80rpm. Heart rate was recorded throughout the test using a Polar Team 2 system (Polar Electro Inc., Lake Success, NY, USA). Lastly, we calculated VO2max relative to body weight (ml/kg/min).
Aerobic fitness was classified into two categories: low and high aerobic fitness, according to percentile 50, based on the previously published reference data for gender and age.23
Adherence to the Mediterranean dietAdherence to the MD was assessed by using the specific and previously validated questionnaire of the PREDIMED study.24 To obtain the overall score, a value of +1 is assigned to each of the items presenting a positive connotation with regard to the MD, while a value of 0 is assigned when the items have a negative connotation. The degree of adherence to the MD was determined from the sum of the values obtained for the 14 items. The resulting score was classified into two categories: low adherence to MD (range 0–7) and high adherence to MD (range 8–14).25
Cardiometabolic risk indexA global cardiometabolic risk index (CMRI) was calculated as an integrated measure of the cardiometabolic risk profile. Each risk factor was standardized making adjustment for gender, using the following formula: Z-score=(value−mean)/standard deviation. The CMRI was calculated by summing the standardized values of the following variables: percentage body fat, waist circumference, MBP, plasma triglycerides, plasma glucose and TNF-α. Blood cholesterol could also have been included in this calculation; the measurement of this parameter was not possible, however.
Combination of groups according to aerobic fitness levels and adherence to the Mediterranean dietFour groups were created with the possible combinations, based on the aerobic fitness categories (high: >percentile 50 and low: ≤percentile 50), according to the abovementioned reference values for gender and age, and adherence to the MD (high: range 8–14 and low: range 0–7). The four groups were defined as follows: “high aerobic fitness and high adherence to MD”; “high aerobic fitness and low adherence to MD”; “low aerobic fitness and high adherence to MD”; and “low aerobic fitness and low adherence to MD”.
Statistical analysisThe statistical analysis of the data was performed using the SPSS version 22 statistical package (SPSS Inc., IBM). A significance level of 95% was established for all statistical analyses (p=0.05). Normal distribution of the samples was assessed using the Kolmogorov–Smirnov test, histograms, standard error of residuals, and Cook distances. Data not exhibiting a normal distribution were subjected to natural log transformation. As descriptive statistics, we calculated the mean (standard deviation [SD]) or median (percentile 25–75) for variables with a non-normal distribution, stratified by body weight status. Differences regarding body status were evaluated using the Student t-test or Mann–Whitney U-test.
Linear regression models were used to explore the association between aerobic fitness as an independent variable and the cardiometabolic risk factors (the BMI, waist circumference, percentage body fat, MBP, triglycerides, blood glucose, IL-6 and TNF-α) and the CMRI as dependent variables. Three linear regression models were analyzed: unadjusted model 1, model 2 adjusted for gender and age, and model 3 adjusted for gender, age and adherence to the MD.
The combined effect of aerobic fitness and adherence to the MD was assessed by the comparison of means (4 groups) based on one-factor analysis of variance (ANOVA), with Bonferroni correction for multiple comparisons.
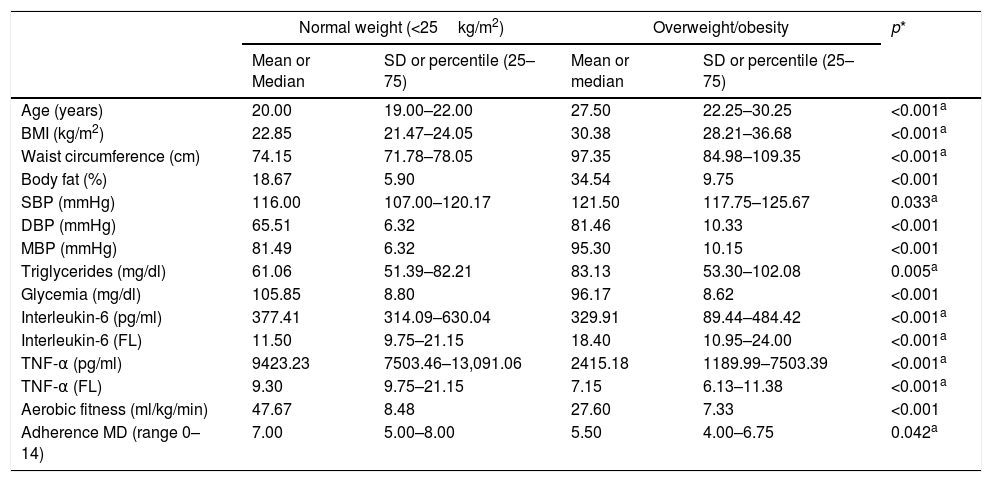
ResultsA total of 79 subjects (38% females) yielded valid data for all measured variables and were included in the study. Table 1 shows the descriptive data of the analyzed sample stratified by body status. Statistically significant differences were observed for all the study variables between participants with normal weight and those with overweight/obesity. The subjects with normal weight had a healthier profile for all variables referring to cardiometabolic risk, except for blood glucose, IL-6 and TNF-α, where the values were higher than in the overweight/obese subjects. Fifty-nine percent of the males showed high physical fitness (p<0.001), and 51% exhibited high adherence to the MD, versus 50% and 50% of the females, respectively. Women had lower diastolic blood pressure, blood glucose and aerobic fitness levels, as well as higher percentage body fat, as compared to men. In contrast, no significant gender differences were found in terms of the BMI, waist circumference, diastolic blood pressure and MBP, triglycerides, IL-6, TNF-α, or adherence to the MD (data not shown).
Descriptive characteristics of the sample of the NUTAF project (n=79).
| Normal weight (<25kg/m2) | Overweight/obesity | p* | |||
|---|---|---|---|---|---|
| Mean or Median | SD or percentile (25–75) | Mean or median | SD or percentile (25–75) | ||
| Age (years) | 20.00 | 19.00–22.00 | 27.50 | 22.25–30.25 | <0.001a |
| BMI (kg/m2) | 22.85 | 21.47–24.05 | 30.38 | 28.21–36.68 | <0.001a |
| Waist circumference (cm) | 74.15 | 71.78–78.05 | 97.35 | 84.98–109.35 | <0.001a |
| Body fat (%) | 18.67 | 5.90 | 34.54 | 9.75 | <0.001 |
| SBP (mmHg) | 116.00 | 107.00–120.17 | 121.50 | 117.75–125.67 | 0.033a |
| DBP (mmHg) | 65.51 | 6.32 | 81.46 | 10.33 | <0.001 |
| MBP (mmHg) | 81.49 | 6.32 | 95.30 | 10.15 | <0.001 |
| Triglycerides (mg/dl) | 61.06 | 51.39–82.21 | 83.13 | 53.30–102.08 | 0.005a |
| Glycemia (mg/dl) | 105.85 | 8.80 | 96.17 | 8.62 | <0.001 |
| Interleukin-6 (pg/ml) | 377.41 | 314.09–630.04 | 329.91 | 89.44–484.42 | <0.001a |
| Interleukin-6 (FL) | 11.50 | 9.75–21.15 | 18.40 | 10.95–24.00 | <0.001a |
| TNF-α (pg/ml) | 9423.23 | 7503.46–13,091.06 | 2415.18 | 1189.99–7503.39 | <0.001a |
| TNF-α (FL) | 9.30 | 9.75–21.15 | 7.15 | 6.13–11.38 | <0.001a |
| Aerobic fitness (ml/kg/min) | 47.67 | 8.48 | 27.60 | 7.33 | <0.001 |
| Adherence MD (range 0–14) | 7.00 | 5.00–8.00 | 5.50 | 4.00–6.75 | 0.042a |
Data are presented as the mean and standard deviation (SD) or median and percentile 25–75 (for those variables that do not exhibit a normal distribution).
MD: Mediterranean diet; FL: fluorescence; BMI: body mass index; DBP: diastolic blood pressure; MBP: mean blood pressure; SBP: systolic blood pressure; TNF-α: tumor necrosis factor-alpha.
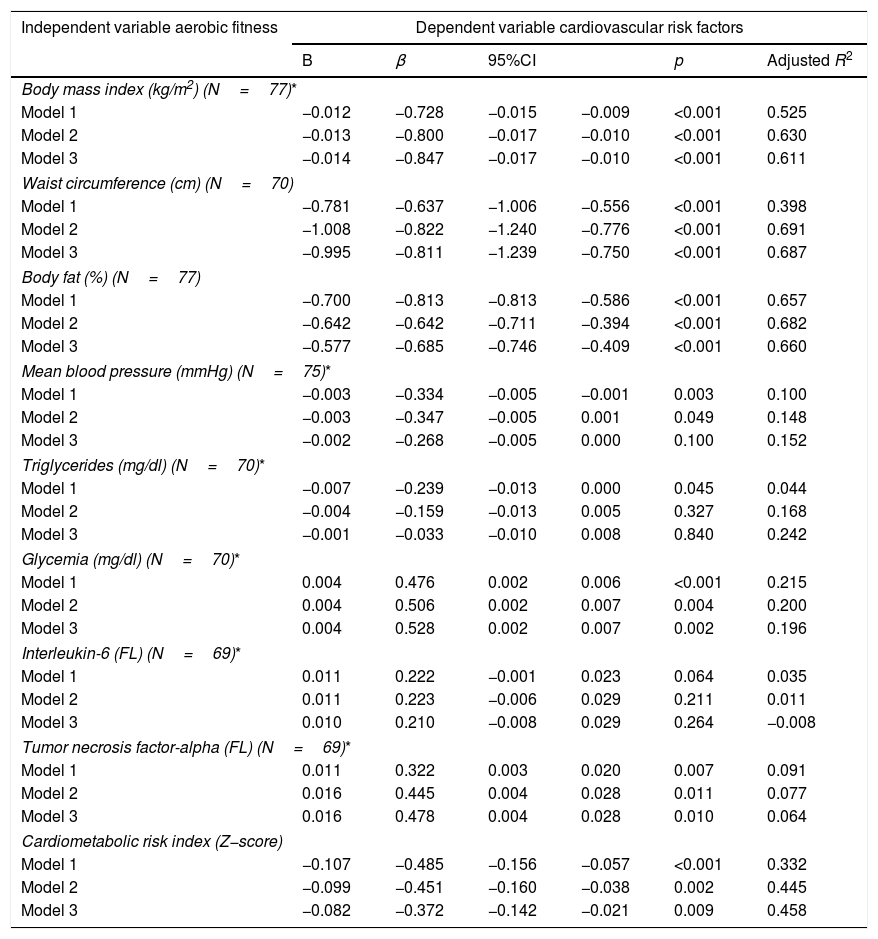
Table 2 shows the linear regression model analyzing the association between aerobic fitness and cardiometabolic risk factors, individually and grouped for the CMRI. No gender interaction was observed; the analyses were therefore made without differentiating between men and women. Model 1 (unadjusted) revealed a negative association between aerobic fitness and the BMI (β=−0.728; p=0.001), waist circumference (β=−0.637; p=0.001), percentage body fat (β=−0.813; p=0.001), MBP (β=−0.334; p=0.100), triglycerides (β=−0.239; p=0.045) and the CMRI (β=−0.485; p=0.001); and a positive correlation to blood glucose (β=0.476; p=0.001) and TNF-α (β=0.322; p=0.007). In general, the association remained statistically significant after adjusting for gender and age (Model 2) or adherence to the MD (Model 3). The association was lost in the case of triglycerides (models 2 and 3) and MBP (model 3). Only IL-6 showed no association in any of the models.
Linear regression model examining the association between aerobic fitness and cardiometabolic risk factors.
| Independent variable aerobic fitness | Dependent variable cardiovascular risk factors | |||||
|---|---|---|---|---|---|---|
| B | β | 95%CI | p | Adjusted R2 | ||
| Body mass index (kg/m2) (N=77)* | ||||||
| Model 1 | −0.012 | −0.728 | −0.015 | −0.009 | <0.001 | 0.525 |
| Model 2 | −0.013 | −0.800 | −0.017 | −0.010 | <0.001 | 0.630 |
| Model 3 | −0.014 | −0.847 | −0.017 | −0.010 | <0.001 | 0.611 |
| Waist circumference (cm) (N=70) | ||||||
| Model 1 | −0.781 | −0.637 | −1.006 | −0.556 | <0.001 | 0.398 |
| Model 2 | −1.008 | −0.822 | −1.240 | −0.776 | <0.001 | 0.691 |
| Model 3 | −0.995 | −0.811 | −1.239 | −0.750 | <0.001 | 0.687 |
| Body fat (%) (N=77) | ||||||
| Model 1 | −0.700 | −0.813 | −0.813 | −0.586 | <0.001 | 0.657 |
| Model 2 | −0.642 | −0.642 | −0.711 | −0.394 | <0.001 | 0.682 |
| Model 3 | −0.577 | −0.685 | −0.746 | −0.409 | <0.001 | 0.660 |
| Mean blood pressure (mmHg) (N=75)* | ||||||
| Model 1 | −0.003 | −0.334 | −0.005 | −0.001 | 0.003 | 0.100 |
| Model 2 | −0.003 | −0.347 | −0.005 | 0.001 | 0.049 | 0.148 |
| Model 3 | −0.002 | −0.268 | −0.005 | 0.000 | 0.100 | 0.152 |
| Triglycerides (mg/dl) (N=70)* | ||||||
| Model 1 | −0.007 | −0.239 | −0.013 | 0.000 | 0.045 | 0.044 |
| Model 2 | −0.004 | −0.159 | −0.013 | 0.005 | 0.327 | 0.168 |
| Model 3 | −0.001 | −0.033 | −0.010 | 0.008 | 0.840 | 0.242 |
| Glycemia (mg/dl) (N=70)* | ||||||
| Model 1 | 0.004 | 0.476 | 0.002 | 0.006 | <0.001 | 0.215 |
| Model 2 | 0.004 | 0.506 | 0.002 | 0.007 | 0.004 | 0.200 |
| Model 3 | 0.004 | 0.528 | 0.002 | 0.007 | 0.002 | 0.196 |
| Interleukin-6 (FL) (N=69)* | ||||||
| Model 1 | 0.011 | 0.222 | −0.001 | 0.023 | 0.064 | 0.035 |
| Model 2 | 0.011 | 0.223 | −0.006 | 0.029 | 0.211 | 0.011 |
| Model 3 | 0.010 | 0.210 | −0.008 | 0.029 | 0.264 | −0.008 |
| Tumor necrosis factor-alpha (FL) (N=69)* | ||||||
| Model 1 | 0.011 | 0.322 | 0.003 | 0.020 | 0.007 | 0.091 |
| Model 2 | 0.016 | 0.445 | 0.004 | 0.028 | 0.011 | 0.077 |
| Model 3 | 0.016 | 0.478 | 0.004 | 0.028 | 0.010 | 0.064 |
| Cardiometabolic risk index (Z−score) | ||||||
| Model 1 | −0.107 | −0.485 | −0.156 | −0.057 | <0.001 | 0.332 |
| Model 2 | −0.099 | −0.451 | −0.160 | −0.038 | 0.002 | 0.445 |
| Model 3 | −0.082 | −0.372 | −0.142 | −0.021 | 0.009 | 0.458 |
β: estimated value; CI: confidence interval; global cardiometabolic risk index: generated from the sum of the following standardized risk factors (Z-score) according to gender: percentage body fat, waist circumference, mean blood pressure, triglycerides, blood glucose and TNF-α; FL: fluorescence; Model 1: unadjusted linear regression; Model 2: linear regression adjusted for gender and age; Model 3: linear regression adjusted for gender, age and adherence to MD; p: significance; R2: coefficient of determination.
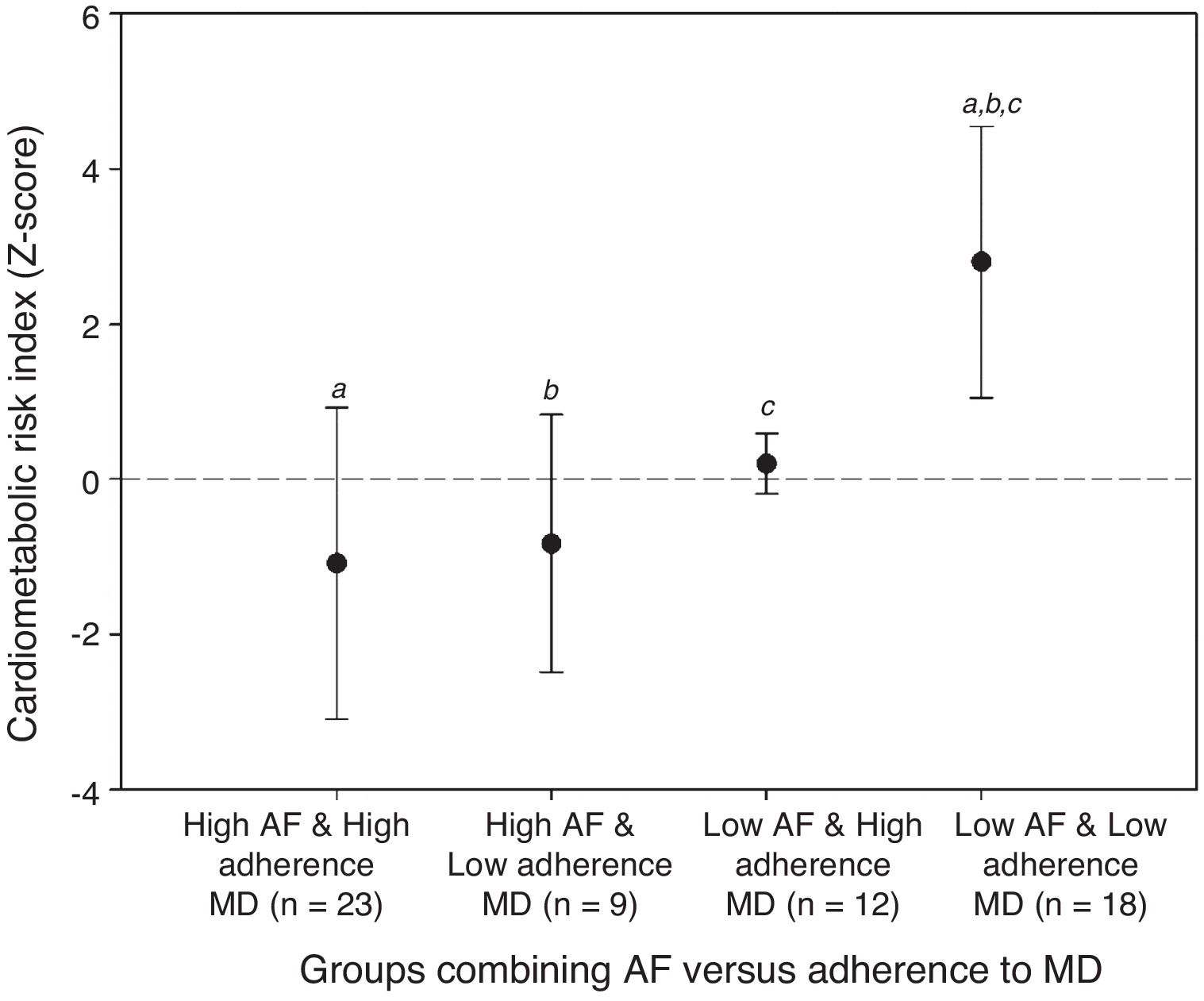
Fig. 1 shows the combined effect of aerobic fitness and adherence to the MD upon the CMRI. There were significant differences among the groups (p<0.001): the “low aerobic fitness and low adherence to MD” group presented greater cardiometabolic risk than the other groups. The analyses were repeated, this time adjusted for gender (analysis of covariance [ANCOVA]), and the results were not seen to change (data not shown).
Combined effect of aerobic fitness and adherence to the Mediterranean diet upon the global cardiometabolic risk index.
AF: aerobic fitness; MD: Mediterranean diet; CMRI: global cardiometabolic risk index, obtained after summing the standardized risk factors (Z-score) according to gender (% fat, waist circumference, mean blood pressure, triglycerides, blood glucose and TNF-α).
a,b,c repetitions mean statistically significant differences, respectively, between groups.
The present study analyzed the association between aerobic fitness and cardiometabolic risk factors in adults, and whether this relationship is independent of adherence to the MD or not. In addition, an analysis was made of the combined effect of aerobic fitness and adherence to the MD upon global cardiometabolic risk in adults.
The results obtained indicate the existence of an inverse relationship between aerobic fitness and the BMI, waist circumference, percentage body fat, MBP and the CMRI after adjusting for age and gender (model 2). In general, these results are consistent with those of previous studies which indicate that higher aerobic fitness is inversely associated with body parameters such as the BMI, waist circumference and percentage body fat.8,26 Also, improved aerobic fitness is inversely correlated to metabolic markers such as high blood pressure and high global cardiometabolic risk.27 In addition, high aerobic fitness may contribute to attenuating certain cardiovascular risk factors, such as obesity, arterial hypertension or hyperlipidemia.28
Likewise, a positive association was seen between aerobic fitness and blood glucose and TNF-α levels after adjusting for age and gender. The results are not in line with previous studies indicating that exercise is beneficial for glycemic control29; however, the mean plasma glucose values observed in our population fall within the acceptable range for healthy individuals (70–100mg/dl). This may be due to the absence of disorders related to diabetes in the subjects studied. On the other hand, the findings referring to cytokine TNF-α reinforce those of studies evidencing a lack of association between physical performance and inflammatory parameters.30 TNF-α is an indicator of proinflammatory disease processes released by the immune system with the purpose of activating the phagocytosis of toxic compounds, and could be mediated by IL-6 production.31 The proinflammatory role of IL-6 has often been considered; however, in vivo studies have shown that physical exercise has a strong antiinflammatory and immunosuppressive effect: it stimulates several mediators in the inflammatory cascade, such as IL-4 and IL-10, and acts as a TNF- α inhibitor.31,32
In our study, statistically significant differences in IL-6 and TNF-α values were observed between subjects with normal weight and with overweight/obesity; however, there were no clinically significant differences, since none of the subjects had inflammatory disease. Aerobic fitness is related to TNF-α and not to IL-6; previous studies have found IL-6 to be associated with central adiposity, whereby high aerobic fitness could keep IL-6 levels low, especially in the presence of adiposity.33
The literature shows that increased adherence to the MD is also associated with a decrease in inflammatory markers.34 In this respect, a recent study analyzing the effects of the MD upon 24 inflammatory biomarkers found the MD and its antioxidant compounds to modulate the expression of these biomarkers both in the first stage of cardiovascular disease and over the long term, by lowering the levels of cytokines IL-6 and TNF-α.35 However, the IL-6 and TNF-α levels in our sample were not indicative of inflammatory disease; no conclusions therefore can be drawn.
The analyses in our study showed the association between aerobic fitness and cardiometabolic risk factors to be independent of adherence to the MD, with the exception of MBP. In agreement with these results, previous studies on the association between the MD and independent risk factors have found an inverse relationship between the MD and DBP and SBP.36 No association was found between aerobic fitness and plasma triglyceride levels, unlike in other studies suggesting that aerobic fitness exerts a modulating effect upon dyslipidemia,37 and that diets rich in monounsaturated foods, such as the MD, have a beneficial impact upon the lipid profile.38 Despite the results obtained, it must be noted that longitudinal studies such as the PREDIMED survey indicate that high adherence to the MD exerts a cardioprotective effect and reduces the risk of developing type 2 diabetes and obesity.14
On examining the combined effect of aerobic fitness and adherence to the MD, the “low aerobic fitness and low adherence to MD” group exhibited greater cardiometabolic risk than all the other groups, the risk being found to decrease in the groups characterized by high aerobic fitness, regardless of adherence to the MD. Other similar studies analyzing the global cardiometabolic index in adolescents have found that high aerobic fitness reduces the prevalence of cardiometabolic risk, and that aerobic fitness plays a key role in this relationship.39
Another study in European adolescents analyzed the combined effect of a healthy diet and an active lifestyle upon cardiovascular risk factors. The data obtained showed active adolescents (with at least 60min of physical activity daily) to have a healthier cardiovascular profile. Furthermore, the fact of being physically active was seen to reduce the harmful effects of an unhealthy diet.7
Although our study shows aerobic fitness to play a key role in preventing cardiometabolic risk independently of the MD, we cannot overlook the importance of adequate nutrition for good cardiometabolic health. In the present study, the CMRI was calculated based on the variables obtained. It is therefore not possible to follow patterns of previously developed global cardiometabolic risk indices, which makes it difficult to compare our results with those of other studies. In addition, other variables such as total cholesterol, high density lipoprotein-cholesterol (HDLc), low density lipoprotein-cholesterol (LDLc) and insulin resistance have been shown to largely contribute to cardiometabolic risk and to be related to aerobic fitness or diet.39–41
Our study has a number of limitations. As an example, parameters such as total cholesterol, HDLc, LDLc or insulin resistance may be useful for analyzing the association between aerobic fitness and multiple risk factors, as commented above. On the other hand, because of the cross-sectional nature of the data, no cause-effect conclusions can be drawn. Lastly, the sample size and variables not analyzed, such as sociodemographic characteristics or economic status, could have had some influence upon the results.38
With regard to the strengths of our study, mention should be made of the objective measurement of aerobic fitness based on the laboratory test considered to be the gold standard. Associations between aerobic fitness and cardiometabolic risk factors have been established both individually and jointly, and mention must be made of the novel contribution represented by the combined effect of aerobic fitness and adherence to the MD on global cardiometabolic risk in adults.
ConclusionsBased on the results of our study, it can be concluded that aerobic fitness is inversely related to cardiometabolic risk factors associated with adiposity, independently of adherence to the MD. However, high adherence to the MD may influence MBP regulation. The combination of low aerobic fitness and low adherence to the MD is associated with increased overall cardiometabolic risk; furthermore, high aerobic fitness may reduce the adverse consequences of low adherence to the MD.
The findings obtained suggest that in addition to promoting a healthy diet, such as the MD, it is important to achieve and maintain adequate aerobic fitness adjusted to gender and age. Programs integrating physical exercise in the healthcare setting as the primary prevention of cardiovascular and metabolic risk therefore should be encouraged.
FundingThis study was made possible in part by funding obtained in the form of grants corresponding to the UCA Research Projects, Young Research Modality 2016 (Reference: PR2016-041 and PR2016-051).
Conflicts of interestThe authors declare that they have no conflicts of interest.
Thanks are due to the research team that developed the “NUTAF” project for their collaboration, and to the participants who made this study possible.
Please cite this article as: Rebollo-Ramos M, Velázquez-Díaz D, Corral-Pérez J, Barany-Ruiz A, Pérez-Bey A, Fernández-Ponce C, et al. Capacidad aeróbica, dieta mediterránea y factores de riesgo cardiometabólicos en adultos. Endocrinol Diabetes Nutr. 2020;67:113–121.