Extramedullary plasmacytoma is an uncommon manifestation of multiple myeloma that may be present at diagnosis or appear in the course of the disease. The disorder is most commonly located in the upper respiratory tract and oral cavity (80% of all cases), but may also occur in the gastrointestinal tract, bladder, central nervous system, thyroid, breasts, testes, parotid gland, lymph nodes and skin.1
We report the case of a 65-year-old male diagnosed with IgG lambda multiple myeloma (stage iii of the Revised International Staging System [R-ISS]) who had already presented plasmacytoma in the posterior segment of the third rib, and lytic lesions in the dorsal vertebral bodies and right and left ribs. After 5 lines of chemotherapy and autologous hematopoietic stem cell transplantation in the previous 21 months, the patient showed a partial response. He was referred to the endocrinology clinic due to enlargement and increased local temperature of both breasts, associated with pain, and with no fever or history of previous trauma. Examination revealed bilateral gynecomastia with signs of inflammation, more marked in the right breast, where palpation identified a slightly painful breast button of firm consistency measuring approximately 4 cm in diameter, with no galactorrhea or nipple retraction.
The differential diagnosis of palpable breast masses in men includes pseudo-gynecomastia (the accumulation of retroareolar adipose tissue without gland tissue proliferation) and breast cancer. Both of these conditions were ruled out in our patient by the initial examination and subsequent mammography. The differential diagnosis of gynecomastia requires the exclusion of hypogonadism, hyperprolactinemia, hyperthyroidism, kidney disease, chronic liver disease, feminizing testicular or extra-gonadal tumors, and drugs.2
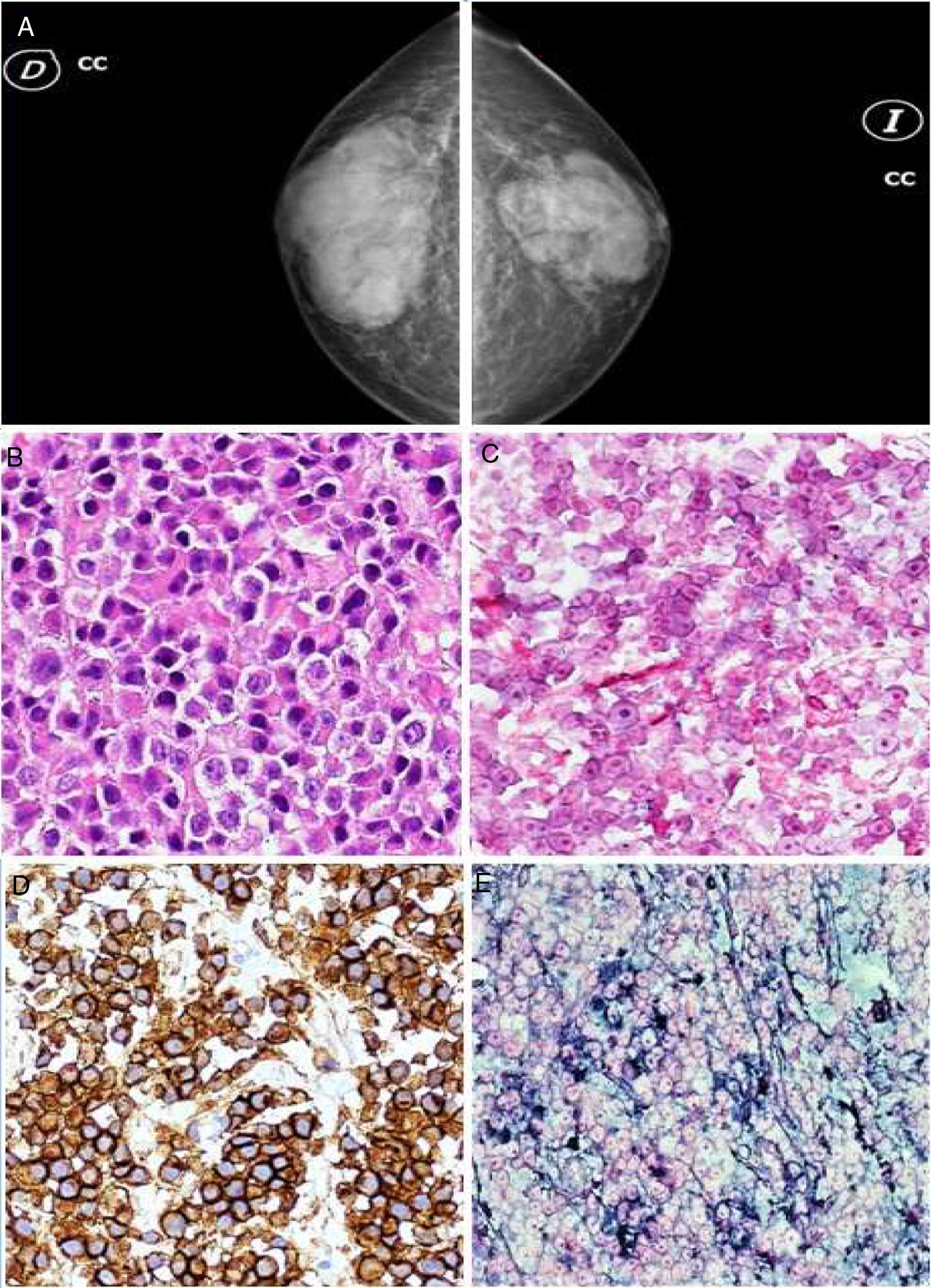
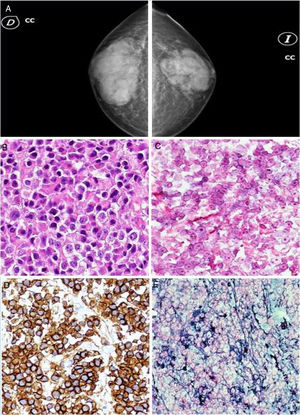
After ruling out possible pharmacological causes, hormone tests revealed FSH 27.4 mIU/mL (reference range 1.5–18), LH 20 mIU/mL (1.4–11.1), prolactin 14.75 ng/mL (4.04–15.2), testosterone 1.76 ng/mL (2.5–11.0), free T4 1.97 ng/dl (0.85–2.00), TSH 3.94 IU/mL (0.27–4.2) and chorionic gonadotropin 0.234 IU/l (0–2). Despite the presence of data consistent with primary hypogonadism, the persistence of bilateral breast pain and induration, with marked inflammatory signs, required the exclusion of other causes. The study was completed by mammography (Fig. 1A) and ultrasound of both breasts, revealing a well-defined glandular breast tissue increase (more marked on the right side), with no nodules, microcalcifications or areas of parenchymal distortion. Since extramedullary plasmacytoma cannot be excluded through imaging tests alone, a core biopsy of both breast lesions was obtained. The histopathological study (Fig. 1B-E) revealed infiltration of both breasts by monoclonal plasma cells (CD138 positive, lambda positive, kappa negative and CD20 negative), consistent with plasmacytoma. Based on these findings, the sixth line of chemotherapy (carfilzomib-lenalidomide-dexamethasone) was suspended at the end of the third cycle, and local radiotherapy was started with 30 Gy, revealing an absence of radiological progression of the breast lesions once treatment had been completed. A new line of chemotherapy was therefore started with dexamethasone-cyclophosphamide-etoposide-cisplatin (DCEP). The patient immediately experienced rapid and severe disease progression, developing plasmacytomas in the right frontal bone, maxillary bone and right testicle, together with severe pancytopenia, bacteremia due to Escherichia coli, and severe worsening of his general condition, requiring hospital admission 15 days after starting DCEP. Following a poor course, with respiratory failure, hematuria and retroperitoneal bleeding, the patient died within a few days.
Monoclonal gammopathies are a group of diseases characterized by the clonal proliferation of plasma cells, ranging from monoclonal gammopathies of uncertain significance to malignant monoclonal gammopathy1. The latter include multiple myeloma and plasmacytomas, in addition to other disorders.
Plasmacytomas can be found in both bone marrow - the most common locations being the spine and peripheral long bones - and in soft tissues (extramedullary plasmacytoma).1,3 Extramedullary plasmacytomas are present in 7-19% of all patients at the time of the diagnosis of multiple myeloma, and occur in another 6-20% during the course of the disease. The mean patient age at diagnosis is 55–60 years, and two-thirds of all cases correspond to males.4–7
Breast plasmacytomas are an extremely rare condition, occurring mainly in women diagnosed with multiple myeloma who have secondary breast involvement, often of a unilateral nature (in over two-thirds of all cases).3,5–8 Imaging tests such as mammography, ultrasound and magnetic resonance imaging are useful.4 The mammographic findings were consistent with those reported in the literature, where they are described as well-defined masses with little or no microcalcifications.5,7 Consensus is lacking regarding the ultrasound findings, since hyperechogenic, hypoechogenic or anechoic lesions may be observed.5,8,9
The final diagnosis is based on the confirmation of monoclonal plasma cell histopathological features shown by immunohistochemistry, in our case involving a core needle biopsy. High-dose radiotherapy with healing intent is the treatment of choice.4,7
It is therefore necessary to maintain a high degree of suspicion in patients diagnosed with multiple myeloma who present either unilateral or bilateral gynecomastia, even if the patient has hypogonadism, and to perform a core needle biopsy of the lesion to confirm cases of extramedullary plasmacytoma.
Please cite this article as: Galán González J, Amaya García MJ, Gordillo Chaves J, Quirón Cebrián JL, Enciso Izquierdo FJ. Ginecomastia bilateral secundaria a plasmocitoma extramedular. Endocrinol Diabetes Nutr. 2020;67:420–422.