Obesity is a health problem of epidemic proportions that is increasingly prevalent in patients with advanced liver disease. Indeed, in many cases obesity contributes to or is even the primary cause of such disease. Current data point to non-alcoholic steatohepatitis as the fastest growing indication of orthotopic liver transplantation (OLT) in the United States, with the potential for becoming the leading indication of OLT.1,2 The presence of obesity worsens the prognosis of OLT, with more short and long term complications in patients with a body mass index (BMI) of >35kg/m2.3 On the other hand, weight gain following OLT is common as a consequence of patient intolerance of physical exercise, immobility and immunosuppressor medication, and can give rise to metabolic syndrome and fatty liver disease in the transplanted organ.4 Weight loss is a key element in the management of these patients, and can lessen the risk of decompensation and the degree of liver fibrosis, as well as afford improved control of the metabolic comorbidities, and increase accessibility to OLT.5
At present, bariatric surgery (BS) is the most effective treatment option for securing significant and sustained weight loss in patients with morbid obesity when dietetic measures have proven to be ineffective.6 A recent systematic review has demonstrated that BS in patients with early stage liver cirrhosis offers metabolic benefits. In this regard, sleeve gastrectomy (SG) is the safest technique, though the associated morbidity-mortality is greater than in patients without liver disease.7
Bariatric surgery has also been postulated as an option in patients with advanced liver disease in the context of OLT, though the evidence is still very limited. Nevertheless, these studies have shown that BS may be feasible and of benefit for these individuals–though it is not without complications, due to the great clinical complexity of these patients.3,8
There is still uncertainty as to what type of surgery is best, when it should be carried out (i.e., before, concomitant to, or after transplantation), and what the long term complications might be.9 Although few data are available in the literature, SG is the most widely recommended surgical technique, due to the shorter surgery time involved and the fact that it does not affect immunosuppressive treatment and does not complicate subsequent endoscopic evaluations of the upper gastrointestinal tract and biliary system.8 Performing SG before liver surgery favors access to OLT on the part of certain patients who otherwise would be excluded because of obesity, and allows for the control of comorbidities.10 However, this approach may delay liver surgery, and also involves the inconvenience and cost of two surgical interventions. Bariatric surgery after OLT may reduce the number of metabolic complications and the development of non-alcoholic fatty liver.3 Using this surgical technique concomitant to transplantation avoids the need for two separate surgical interventions and decreases the technical difficulties caused by the presence of bridles and adhesions. Heimbach et al. described the combination of both procedures in a series of 7 patients who achieved effective weight loss with few post-transplantation metabolic complications.8 Recently, Tariciotti et al. reported the first European case, likewise with favorable results regarding weight loss, the withdrawal of diabetic treatment and adequate graft function.11
We report the case of a 54-year-old male with type 2 obesity who had major complications and liver cirrhosis due to genotype 1 hepatitis C virus infection, Child-Pugh stage C, and a MELD (Model for End-stage Liver Disease) score of 30 points. This patient first suffered edematous-ascitic decompensation four years before OLT, and subsequently experienced multiple decompensation episodes in the form of encephalopathy, spontaneous bacterial peritonitis, dilutional hiponatremia, and refractory ascites, which finally caused him to be put on the OLT waiting list in May 2014. The patient had long-evolving obesity, with a maximum body weight of 132kg and a BMI of 39.5kg/m2, that failed to respond to dietetic measures. His comorbidities included high blood pressure treated with three drugs, type 2 diabetes mellitus, and obstructive sleep apnea syndrome (OSAS), treated with continuous positive airway pressure (CPAP). The patient had suffered diabetes for 12 years, with high insulin requirements (2.4IU/kg/day). Continuous subcutaneous insulin infusion had been prescribed in another center, followed by the addition of exenatide twice a day, with a lowering of his body weight to 126kg and of the insulin dose to 1.07IU/kg/day.
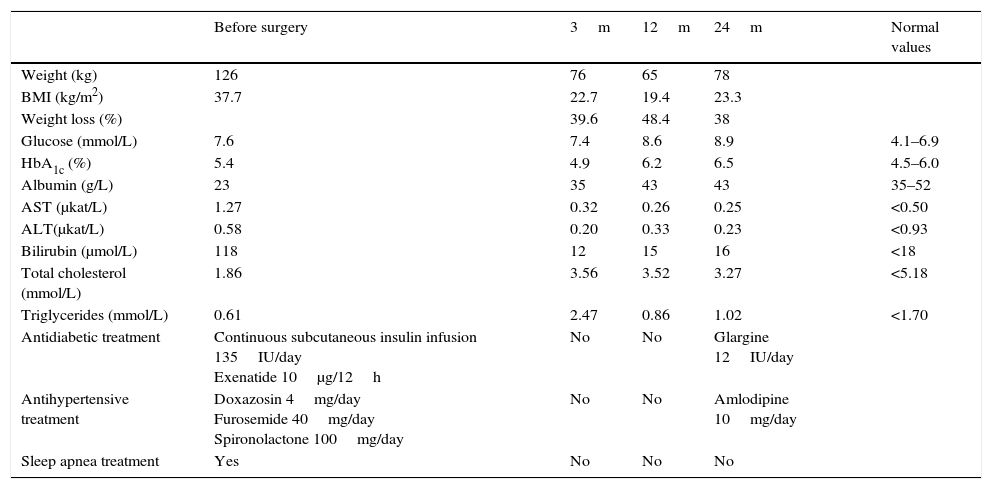
The patient was referred to our hospital, where OLT and BS in the same surgical procedure were decided upon. Orthotopic liver transplantation was performed on 15 October 2014 by the usual procedure, followed by SG, without intraoperative complications. Following the operation the patient presented Klebsiella pneumoniae bacteremia, acute respiratory distress syndrome, colitis due to Clostridium difficile and Cytomegalovirus infection. The insulin dose was gradually tapered during admission. The patient did not require antihypertensive treatment or CPAP at hospital discharge. The usual vitamin supplements and a standard immunosuppressant treatment consisting of mycophenolate 500mg/12h and tacrolimus 7mg/24h were prescribed. Changes over time in weight, comorbidities, and the most relevant laboratory parameters are shown in Table 1. Three and 12 months after surgery, his weight loss was 39% and 48% respectively (BMI 19.4kg/m2). The patient therefore required oral energy and protein supplementation until his weight stabilized one year after surgery. After two years of follow-up, there have been no changes in the nutritional parameters, vitamin deficiencies, or plasma immunosuppressant levels.
Changes over time in weight, comorbidities and the most relevant laboratory parameters.
| Before surgery | 3m | 12m | 24m | Normal values | |
|---|---|---|---|---|---|
| Weight (kg) | 126 | 76 | 65 | 78 | |
| BMI (kg/m2) | 37.7 | 22.7 | 19.4 | 23.3 | |
| Weight loss (%) | 39.6 | 48.4 | 38 | ||
| Glucose (mmol/L) | 7.6 | 7.4 | 8.6 | 8.9 | 4.1–6.9 |
| HbA1c (%) | 5.4 | 4.9 | 6.2 | 6.5 | 4.5–6.0 |
| Albumin (g/L) | 23 | 35 | 43 | 43 | 35–52 |
| AST (μkat/L) | 1.27 | 0.32 | 0.26 | 0.25 | <0.50 |
| ALT(μkat/L) | 0.58 | 0.20 | 0.33 | 0.23 | <0.93 |
| Bilirubin (μmol/L) | 118 | 12 | 15 | 16 | <18 |
| Total cholesterol (mmol/L) | 1.86 | 3.56 | 3.52 | 3.27 | <5.18 |
| Triglycerides (mmol/L) | 0.61 | 2.47 | 0.86 | 1.02 | <1.70 |
| Antidiabetic treatment | Continuous subcutaneous insulin infusion 135IU/day Exenatide 10μg/12h | No | No | Glargine 12IU/day | |
| Antihypertensive treatment | Doxazosin 4mg/day Furosemide 40mg/day Spironolactone 100mg/day | No | No | Amlodipine 10mg/day | |
| Sleep apnea treatment | Yes | No | No | No |
A liver biopsy performed 10 months after transplant showed a preserved parenchymal architecture with signs of predominantly lobular hepatitis and no evidence of rejection. One and a half years after OLT, the patient was administered HCV eradication therapy with ledipasvir/sofosbuvir, which resulted in the negativization of viral RNA.
The reported case shows that BS combined with OLT may be a treatment option in selected patients with end-stage liver disease. SG was selected because it is less complicated, has no malabsorptive component, and involves less risk of malnutrition. Combined surgery was decided upon because it implied a single procedure and patient recovery, thus avoiding the need for repeat surgery in a potentially more complicated surgical field because of the presence of bridles. It also avoided a delay in BS due to complications associated with transplantation, such as rejection, infection, intercurrent diseases, or surgical complications such as biliary stenoses.
SG achieved a sustained weight loss at two years, and an improvement in the associated metabolic comorbidities. However, during the first months the patient experienced excess weight loss that required close nutritional monitoring. Such weight loss was influenced not only by the restrictive component of the surgery, but also by multiple post-transplant complications, including bacteremia, respiratory infection, Clostridium colitis and Cytomegalovirus infection. In turn, antiviral treatments with valganciclovir and foscarnet caused multiple gastrointestinal side effects. These complications were to be expected following OLT, since postoperative respiratory complications are frequent in patients with very advanced liver disease. On the other hand, although serological tests for Cytomegalovirus were negative in our patient before OLT, the organ donor was positive, and in this situation Cytomegalovirus infection is practically inevitable.
Further studies are needed to broaden the existing evidence on the role of BS in patients with end-stage liver disease and to improve candidate selection, establish the most adequate surgery and the best time to perform it, and assess the long term benefits and complications.
Please cite this article as: Guerrero Pérez F, Pia Marengo A, Fabregat J, Xiol X, Vilarrasa N. Gastrectomía vertical y trasplante hepático ortotópico combinado en paciente con obesidad de tipo 2 y enfermedad hepática avanzada. Endocrinol Diabetes Nutr. 2017;64:282–284.