Turner syndrome (TS) is a result of X chromosome monosomy and affects 25–50 per 100,000 females at birth. Several advances at the treatment level have lead to a reduction in part of the morbidity associated with the syndrome; however, its follow-up must be multidisciplinary.1,2 During childhood, pediatric endocrinologists are responsible for their follow-up and they coordinate all the other medical specialists. In adult life, this coordinating role can be lost; therefore, it is advisable to create specialized units which offer long-term follow-up and allow a correct transition to adult care systems.2–4 We develop a cross-sectional descriptive study, with patients older than 16 years old who suffer from TS in our country, using a questionnaire that contains 5 sections: demographic data, clinical items, employment situation, educational level, current health situation and follow-up in the last year. The questionnaire was sent by email or made by telephone and by means of self-report. All patients gave informed consent either verbal if the questionnaire was made by telephone or written if the questionnaire was sent by e-mail and the study was carried out according to the indications of the ethics committee of the center.
The inclusion of subjects was carried out thanks to the collaboration of five associations of women with TS (Andalucía, Salamanca, Aragón, Galicia, Madrid) and three third level hospitals (Hospital Materno Infantil de Málaga, Hospital Materno Infantil de Badajoz, Hospital Virgen de la Victoria de Málaga).
A total of 70 questionnaires were received. The median age was 29.5 years (interquartile range [IQR] 18) with median age at diagnosis of 7 years (IQR 4). Seventy women (70%) reported having been treated with growth hormone (GH) with median age at starting of 8 years old (IQR 6.5). The median height was 150cm (IQR 10) with median body mass index (BMI) 24.74 kg/m2 (IQR 5.73). There were no significant differences in adult height, weight or BMI between the women treated with GH and those non-treated. However, treated women had lower weight and lower BMI but this difference was not statistically significant.
Regarding the educational level, 80% had a medium-high level of education (secondary school, middle grade or higher studies, university degree) and 41.4% were currently studying. Eighty percent were working and/or studying and 20% reported being unemployed, retired or with permanent disability. Comparing the group of women with TS between 25 and 44 years of age with women the same age from general population (INE 2016 data available at www.ine.es), no statistically significant differences were found with respect to the level of education or in the percentage of employed women. A total of 67.1% of women referred living with their parents with statistically significant difference (p 0.002) comparing with people from the general population and same age in Spain (data from INE 2016).
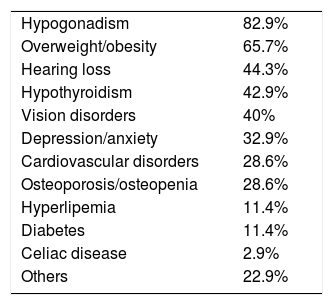
Concerning the current health status (see Table 1), the most common illness was hypogonadism (82.9%), followed by overweight/obesity (65.7%), hearing loss (44.3%), hypothyroidism (42.9%) and vision disorders (40%).
A total of 32.9% women referred suffering from anxiety or depression, although only 25.7% had been evaluated by a psychologist in the last year. There was no association between the level of clinical involvement, evaluated by the number of affected organs, and educational level.
Most women (85.7%) had visited their family doctor in the last year and 91.4% had visited a medical specialist, especially an endocrinologist (73.6%) and/or internal medicine specialist (5.8%). Only one patient referred not having any medical follow-up.
We present the first study conducted in Spain of TS patients of adult age, showing their state of health, health care and various social variables. As has been described before, patients who had been treated with GH achieved similar height to non-treated ones; non-treated patients probably were taller anyway, which is why they were not candidates for GH treatment. Treated women had lower weight and lower BMI, which reinforces the idea of the positive metabolic effect of growth hormone in certain pathologies. Overweight or obesity were present in 65.7% of women; therefore, it is advisable to carry out an intensive follow-up of such patients, focusing on healthy life style and diet to reduce the risk of developing metabolic syndrome and cardiovascular events.3,5,6
In our patients, educational level and employment status were similar to the general female population; similar results were described in studies of Naess EE et al. and Gould HN et al.7,8 We did not find any relation between the number of affected organs and the educational level, so there does not seem to be a direct relationship between the degree of clinical involvement and psychomotor development.7,8
Concerning the follow-up, all guideline insist on a follow-up by a multidisciplinary team lead by an endocrinologist and/or internal medicine specialist. In our series, there is a percentage of women that lacks follow-up by this type of specialist. On the other hand, different behavioral problems and psychological disorders have been described in TS patients. In our series, 32.9% of women referred suffering from depression or anxiety; however, only 25.7% had been evaluated by a psychologist in the last year. Accordingly, it seems advisable to assess and monitor these patients by mental health teams who understand their needs.2,4,9,10
To summarize, although patients with Turner syndrome present health problems that usually involve several systems; these alterations do not seem to affect their level of education or employment. Follow-up in adult life continues to be heterogeneous and it is necessary that multidisciplinary groups take on this responsibility. Finally, most of the patients taking part in our study were included thanks to their participation in associations or during follow-up in outpatient consultations; this may indicate that they have a better level of follow-up than other women with TS in Spain. Likewise, the data collected are those provided by the women themselves, so caution is required when considering their analyses and conclusions.
Conflict of interestThe authors declare no competing financial interest.
We would like to thank the Turner Syndrome associations of Andalucía, Salamanca, Aragón, Galicia and Madrid, whose dissemination of the study has facilitated its development and all the women who have wanted to participate in it.