The efficacy and safety of inpatient hyperglycemia management protocols using basal-bolus regimens have been widely demonstrated, but their implementation is insufficient. The aim of the study was to assess implementation and to establish the efficacy and safety of inpatient hyperglycemia management protocol based on a basal-bolus regimen and the incorporation of a nurse consultant.
Material and methodsEvaluation was performed at 10 hospital units. Data were retrospectively reviewed during hospital stay and 90 days after discharge in 400 patients after protocol implementation and 200 patients before implementation.
The degree of satisfaction of professionals was assessed using a questionnaire 12 months after implementation.
ResultsThe proportion of patients with basal-bolus regimens upon admission was higher in the postimplementation group (58% vs. 9%, P < 0.001). Mean pre-prandial and bedtime blood glucose levels during admission were lower in the postimplementation group (164 ± 41 mg/L vs. 196 ± 50 mg/dL, P < 0.001). After implementation, there were less patients with blood glucose levels > 300 mg/dL (36.3% vs. 50.5%, P < 0.001) and more patients with values < 70 mg/dL (15% vs. 9%, P = 0.040). Insulin addition and intensification was the main change in treatment at discharge, and a significant HbA1c reduction was seen three months after discharge in the postimplementation phase (P = 0.04). The professionals assigned the protocol a score of 4.5 on a 1–5 scale.
ConclusionsIncorporation of a nurse consultant expert in diabetes as key component of a hyperglycemia management program ensures that a majority of patients admitted to hospital for hyperglycemia receive treatment with a basal-bolus regimen and improves blood glucose control during hospital stay and after discharge.
La eficacia y seguridad de los protocolos de manejo de la hiperglucemia hospitalaria con pautas basal-bolo están ampliamente demostradas, pero su implementación es insuficiente. El objetivo del estudio fue valorar la implantación y determinar la eficacia y seguridad de un protocolo de manejo de la hiperglucemia hospitalaria basado en la terapia basal-bolo y la incorporación de una enfermera consultora.
Material y métodosLa evaluación se realizó en 10 unidades de hospitalización. Se revisaron retrospectivamente los datos durante la hospitalización y a los 90 días tras el alta de 400 pacientes postimplantación y 200 pacientes preimplantación del protocolo. El grado de satisfacción de los profesionales se valoró mediante un cuestionario a los 12 meses de la implantación.
ResultadosLa proporción de pacientes con pauta basal-bolo en el ingreso fue superior en el grupo postimplantación (58% frente a 9%, p < 0,001). La media de las glucemias prepandiales y al acostarse durante el ingreso fue menor en el grupo postimplantación (164 ± 41 mg/dl frente a 196 ± 50 mg/dl, p < 0,001). La proporción de pacientes con glucemias > 300 mg/dl fue menor (36,3% frente a 50,5%; p < 0,001) y con glucemias < 70 mg/dl fue superior (15% frente a 9%, p = 0,040) en el grupo postimplantación. La adición e intensificación de la insulina fue la principal modificación del tratamiento al alta y se observó reducción significativa de la HbA1c a los 3 meses del alta en la fase postimplantación (p = 0,04). La valoración del protocolo por parte de los profesionales fue de 4,5 en una escala de 1 a 5.
ConclusionesLa incorporación de una enfermera consultora experta en diabetes como elemento central del programa de manejo de la hiperglucemia consigue que la mayoría de los pacientes hospitalizados con hiperglucemia reciban tratamiento con una pauta basal-bolo y una mejora del control glucémico durante la hospitalización y tras el alta.
Hyperglycemia during hospital admission is a significant, growing and often underestimated complication in terms of prevalence, morbidity and costs.1–4 Observational studies show that hyperglycemia during hospital admission affects 35–40% of all patients. In addition to acting as a marker of severity, it has important adverse effects that influence patient prognosis, with an impact in terms of increased morbidity, mortality and infection rates.4,5 In addition, patients with diabetes mellitus (DM) remain in hospital for an average of 1–3 more days than non-diabetic individuals, and are more likely to require admission to the Intensive Care Unit (ICU).6 Furthermore, the hospitalization of diabetic patients accounts for 50% of the healthcare costs attributed to DM.7–9
In Spain, the publication of consensuses on the management of hyperglycemia in hospital6 and on the treatment at discharge of patients with hyperglycemia7 has led to the progressive implementation at many centers of hyperglycemia management protocols based on basal-bolus regimens, with variable success.8–11 Two multicenter studies conducted in Spain confirm the efficacy and safety of the recommendations,12,13 though the situation is still far from ideal.8,14,15
At Hospital de la Santa Creu i Sant Pau in Barcelona (Spain), the hyperglycemia management protocol based on basal-bolus therapy incorporated the nurse consultant as a key element for the implementation and development of the protocol. The purpose of this study was to assess the efficacy and safety of the protocol for the management of inpatient hyperglycemia, comparing it to the situation in the pre-implementation period, and to assess the degree of satisfaction of the professionals responsible for care in the hospital wards.
Material and methodsImplementation of the hyperglycemia management protocolThe protocol for the management of hyperglycemia in non-critically ill patients is based on the recommendations of the Spanish consensuses.6,7 In addition to establishing the basal-bolus insulin regimen as an essential element, it includes instructions for estimating the dose and initial insulin distribution based on the patient’s characteristics, the adjustments according to the capillary blood glucose controls, adaptation to special situations, and treatment reconciliation at discharge.6,7
The protocol was implemented in three hospital units at a time and over a period of three months until all the units were covered, except Psychiatry, Gynecology and Obstetrics, and Pediatrics. To this effect, a first phase comprised information and the involvement of the medical and nursing management bodies, as well as of the ongoing training department of the hospital. An educational intervention was then conducted targeted at physicians and nurses, including an explanation of the protocol and the resolution of practical cases, and the distribution of the action protocol among all the healthcare departments and units (Appendix B annex). A total of 45 training sessions were held in 2012, attended by 220 physicians and 245 nurses. The sessions for physicians lasted 45 min each and were given by the endocrinologist in charge, while those for nurses lasted four hours and were given by the nurse consultant. Having been started in three hospital units, three new units were added to the program every three months, while it remained active in the previous units, until all the targeted specialties were covered. In each unit, the diabetes nurse consultant supervised (first daily and subsequently upon demand) the start up and development of the protocol, consulting the Department of Endocrinology and Nutrition if necessary.
Evaluation of the hyperglycemia management protocolThe evaluation was carried out during 2013 and 2014 in 10 hospital units with patients from medical and surgical specialties (Cardiology, Pneumology, Neurology, General and Digestive Surgery, Traumatology and Orthopedic Surgery, Gastrointestinal Diseases, Hematology, Internal Medicine, Medical Oncology and Palliative Care, ENT, Neurosurgery and Chest Surgery). For the evaluation, data recorded from 400 subjects with a first hospital admission episode after the start of the protocol (40 patients from each unit) and from 200 subjects hospitalized in the same units in the 12 months prior to the start of the protocol (20 patients from each unit) were retrospectively reviewed. We included patients over 18 years of age with a prior diagnosis of DM or without DM but with some persistent glycemia elevation episode (>140 mg/ mg/dl) during their hospital stay, and with a minimum duration of admission of four days. To assess the degree of satisfaction with the protocol, a survey of physicians and nurses was conducted one year after its start, including 7 items relating to the application of the protocol and the role of the nurse consultant. A total of 150 surveys were delivered to the different units for completion by the physicians and nurses of each unit. Delivery was preceded by a brief presentation in which collaboration was requested and confidentiality and anonymity were guaranteed. The study was approved by the Ethics Committee of Hospital de la Santa Creu i Sant Pau.
The following information was collected for each patient: 1) general clinical and diabetes-related conditions prior to admission; 2) length of hospital stay and hospital admissions in the previous 6 months and 90 days after hospitalization; and 3) data relating to treatment and glycemic control during the hospital stay and after discharge, including glycosylated hemoglobin (HbA1c) concentration recorded during admission or in the previous three months and three months after discharge, glycemia values through preprandial and bedtime capillary blood glucose monitoring, and the frequency of hypoglycemia (blood glucose <70 mg/dl) and hyperglycemia (>300 mg/dl). The capillary blood glucose values were used to determine mean blood glucose in the first 24 h, mean blood glucose during admission, and mean blood glucose in the 24 h prior to discharge.
Statistical analysisData analysis was performed using the SPSS version 22 statistical package.
Qualitative variables were expressed as absolute values or percentages, and differences between subgroups were assessed using the chi-squared test.
Quantitative variables in turn were reported using measures of central tendency and dispersion (mean, standard deviation [SD], median, minimum and maximum), and comparisons between the two groups were made using the Student-test for independent samples or the nonparametric Mann–Whitney U-test. Statistical significance was considered for p < 0.05.
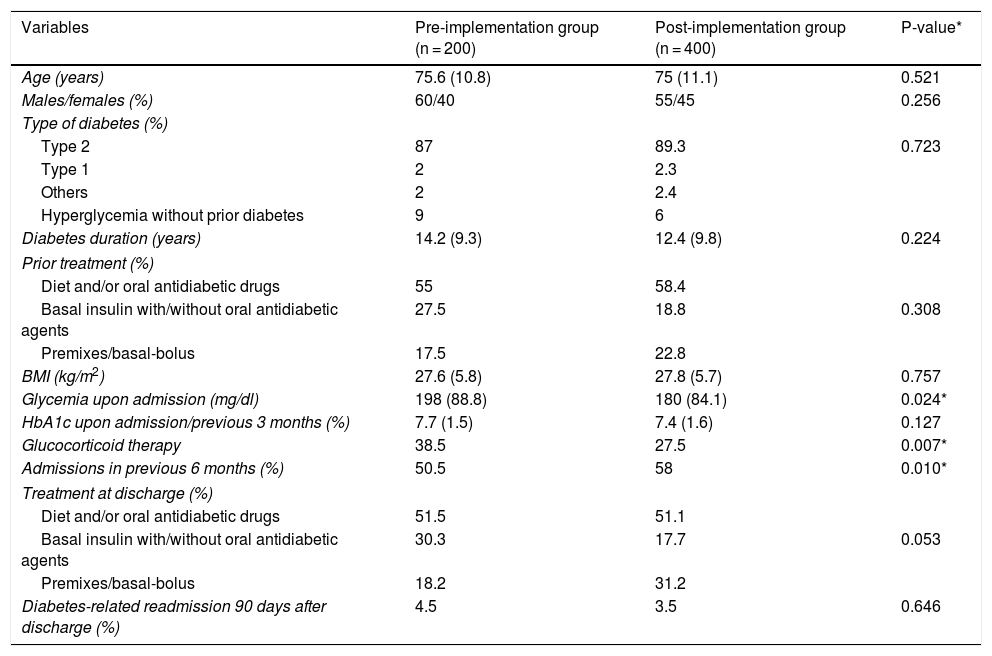
ResultsThe clinical characteristics of the patients at the time of admission are summarized in Table 1. The group of patients prior to implementation of the protocol was characterized by higher blood glucose values upon admission and a greater proportion of individuals treated with glucocorticoids during hospital admission, while the proportion of patients requiring admissions in the previous 6 months was higher in the post-implementation group. There were no significant differences in mean stay.
Characteristics of the patients upon admission and diabetes treatment at hospital discharge in the groups before and after implementation of the hyperglycemia management protocol.
| Variables | Pre-implementation group (n = 200) | Post-implementation group (n = 400) | P-value* |
|---|---|---|---|
| Age (years) | 75.6 (10.8) | 75 (11.1) | 0.521 |
| Males/females (%) | 60/40 | 55/45 | 0.256 |
| Type of diabetes (%) | |||
| Type 2 | 87 | 89.3 | 0.723 |
| Type 1 | 2 | 2.3 | |
| Others | 2 | 2.4 | |
| Hyperglycemia without prior diabetes | 9 | 6 | |
| Diabetes duration (years) | 14.2 (9.3) | 12.4 (9.8) | 0.224 |
| Prior treatment (%) | |||
| Diet and/or oral antidiabetic drugs | 55 | 58.4 | |
| Basal insulin with/without oral antidiabetic agents | 27.5 | 18.8 | 0.308 |
| Premixes/basal-bolus | 17.5 | 22.8 | |
| BMI (kg/m2) | 27.6 (5.8) | 27.8 (5.7) | 0.757 |
| Glycemia upon admission (mg/dl) | 198 (88.8) | 180 (84.1) | 0.024* |
| HbA1c upon admission/previous 3 months (%) | 7.7 (1.5) | 7.4 (1.6) | 0.127 |
| Glucocorticoid therapy | 38.5 | 27.5 | 0.007* |
| Admissions in previous 6 months (%) | 50.5 | 58 | 0.010* |
| Treatment at discharge (%) | |||
| Diet and/or oral antidiabetic drugs | 51.5 | 51.1 | |
| Basal insulin with/without oral antidiabetic agents | 30.3 | 17.7 | 0.053 |
| Premixes/basal-bolus | 18.2 | 31.2 | |
| Diabetes-related readmission 90 days after discharge (%) | 4.5 | 3.5 | 0.646 |
Data expressed as percentages or means (standard deviation).
The proportion of patients receiving basal-bolus insulin during admission was higher in the post-intervention group than in the pre-intervention group (58% versus 9%; p < 0.001). Although the insulin dose was somewhat higher in the post-intervention group (0.36 ± 0.27 IU/kg/day versus 0.31 ± 0.30 IU/kg/day), the difference was not statistically significant (p = 0.057).
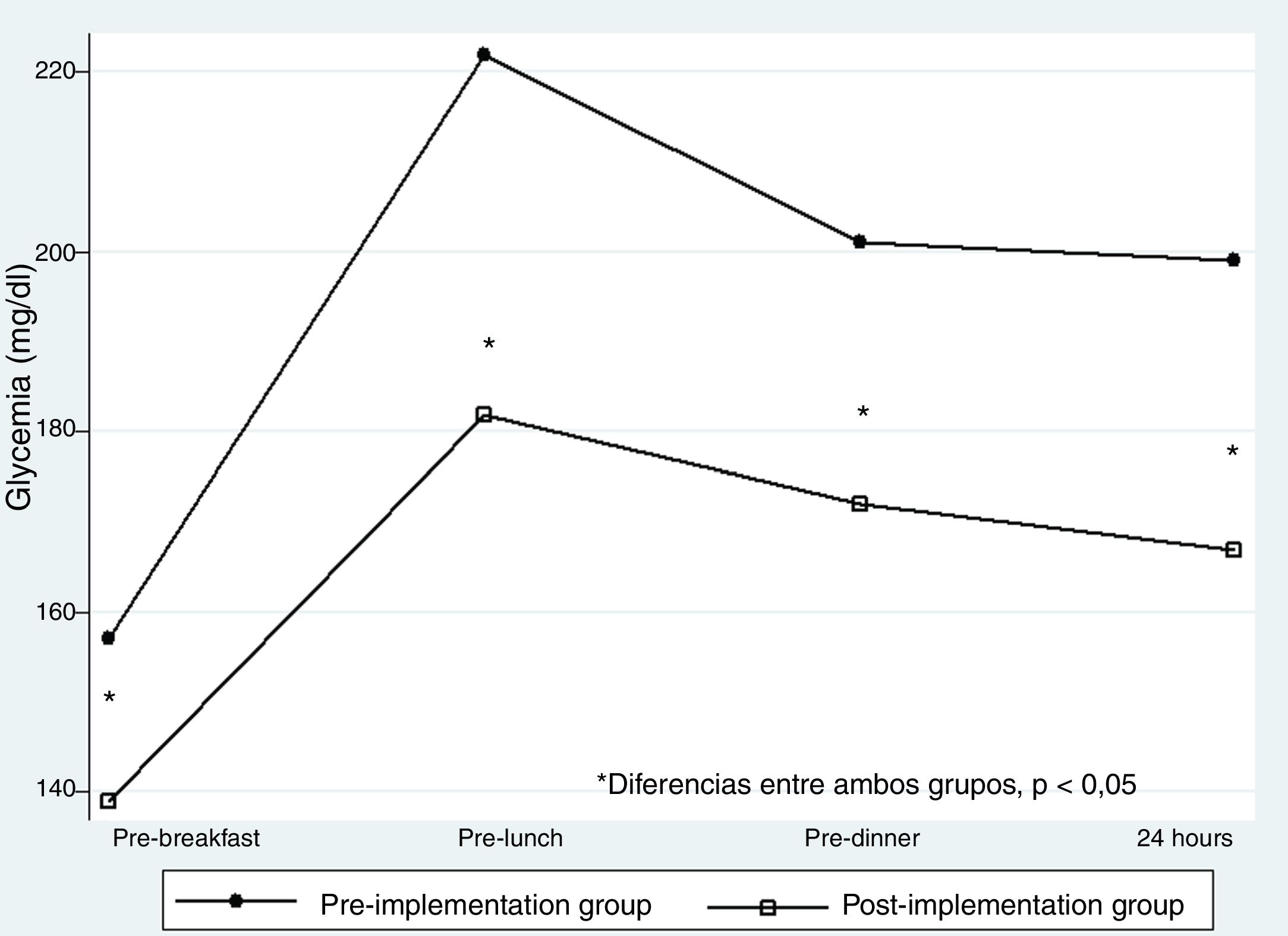
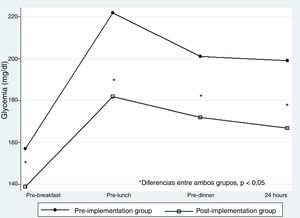
The mean preprandial and bedtime blood glucose levels throughout the hospital stay were lower in the post-intervention group (164 ± 41 mg/dl versus 196 ± 50 mg/dl; p < 0.001). With regard to the pre-intervention group, the reduction was significant (p < 0.001) for the three preprandial glycemia values and bedtime glycemia (Fig. 1).
The proportion of patients with glycemia > 300 mg/dl was lower (36.3% versus 50.5%; p < 0.001), while the proportion of those with glycemia <70 mg/dl was higher (15% versus 9%; p = 0.040) in the group of patients studied after the implementation of the protocol.
The distribution of the different treatments received by the patients before admission and after discharge in both study groups is shown in Table 1. The main change in treatment at discharge was the addition and intensification of insulin, particularly in the post-intervention group.
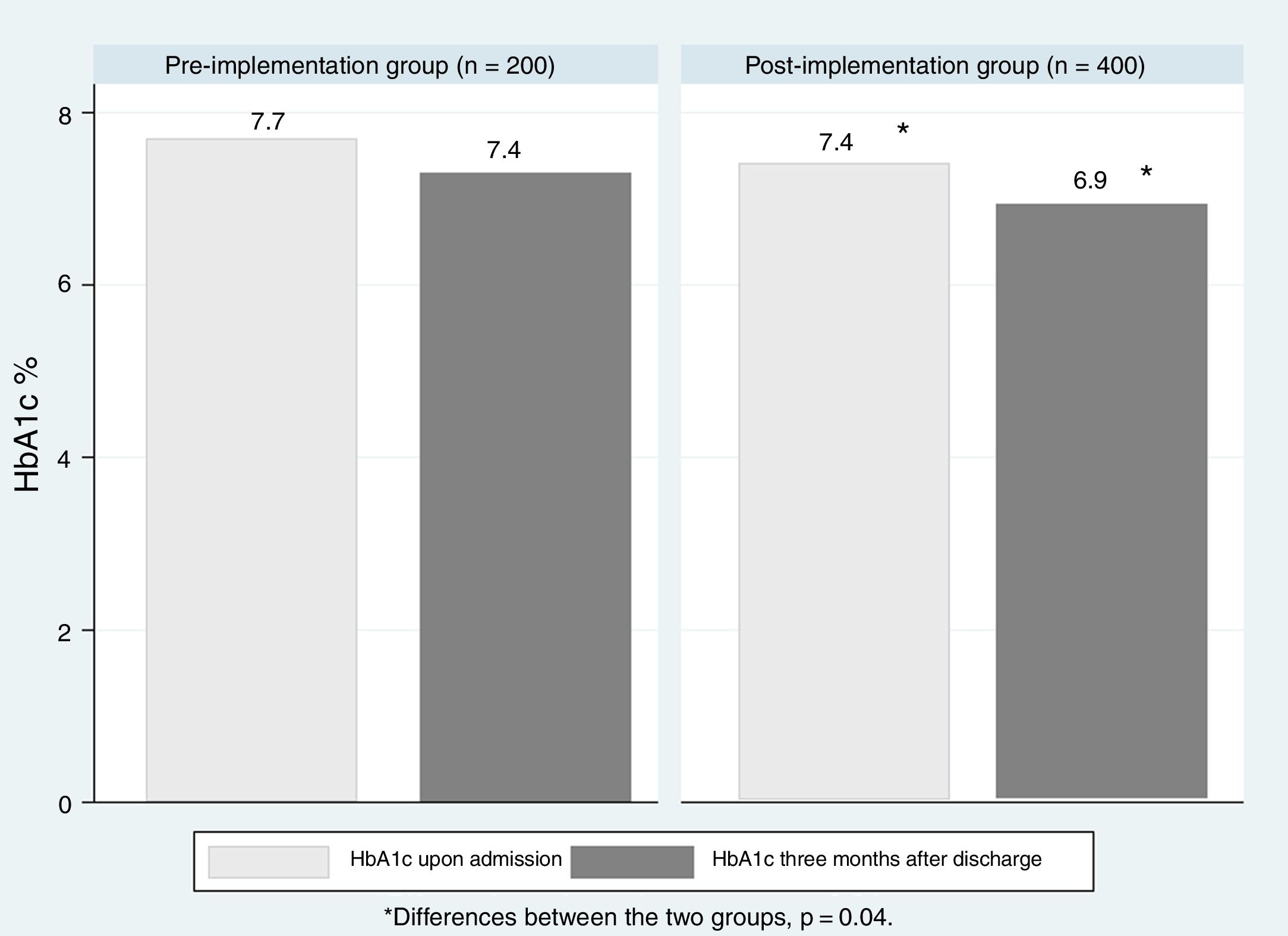
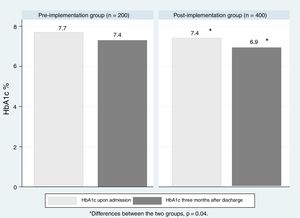
The measurement of HbA1c upon admission or in the last three months was available for 106 of the 200 patients in the pre-implementation group (58.3%) and for 289 of the 400 patients in the post-implementation group (72.3%) (p = 0.006). At 90 days after discharge, HbA1c determinations were available for 57 patients (28.5%) in the pre-implementation group and for 144 patients (36%) in the post-implementation group (p = 0.05). As can be seen in Fig. 2, the treatment modifications were associated with a significant decrease in HbA1c at three months after discharge in the post-implementation group (p = 0.04), while the decrease was not significant in the pre-implementation group (p = 0.157). The proportion of patients readmitted due to acute complications of diabetes was similar in the patients studied before and after the start of the protocol (4.5% versus 3.5%; p = 0.646).
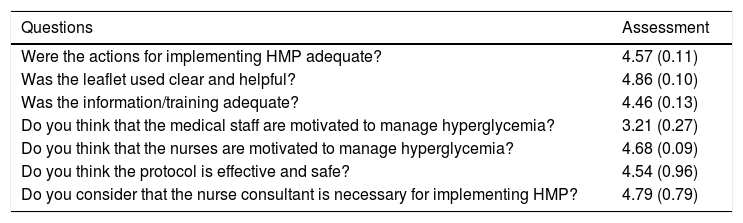
Eighty satisfaction surveys of the 150 distributed among the different units were completed 12 months after the implementation of the protocol. The results are summarized in Table 2. The aspects most valued by the professionals were the clarity and usefulness of the leaflet and the importance of the nurse consultant for the implementation of the protocol.
Satisfaction of the professionals with the hyperglycemia management protocol (HMP) and the role of the nurse consultant.
| Questions | Assessment |
|---|---|
| Were the actions for implementing HMP adequate? | 4.57 (0.11) |
| Was the leaflet used clear and helpful? | 4.86 (0.10) |
| Was the information/training adequate? | 4.46 (0.13) |
| Do you think that the medical staff are motivated to manage hyperglycemia? | 3.21 (0.27) |
| Do you think that the nurses are motivated to manage hyperglycemia? | 4.68 (0.09) |
| Do you think the protocol is effective and safe? | 4.54 (0.96) |
| Do you consider that the nurse consultant is necessary for implementing HMP? | 4.79 (0.79) |
Score from 1–5. Data reported as the mean (standard deviation).
The present study confirms that hyperglycemia management protocols involving basal-bolus insulin regimens are safe and effective. In addition, we contribute new information supporting incorporation of the nurse consultant as a key element in the strategy for implementing programs for the management of inpatient hyperglycemia.
Despite the extensive information available on the efficacy and safety of protocols for the management of hyperglycemia using basal-bolus regimens, the implementation of such protocols is still insufficient,8,10,11,14,15 and despite their proven inefficacy,16,17 mobile rapid insulin regimens are still the only insulin regimen used in a large proportion of hospitalized patients.14,18,19 Fear of hypoglycemia, together with a lack of skills on the part of management and an unwillingness to adjust insulin regimens on the part of other physicians, as well as clinical inertia and the lack of protocolized regimens for the management of hyperglycemia,6 constitute the main barriers to the effective management of inpatient hyperglycemia.
Our protocol is based on the recommendations of the Spanish consensuses on the management of hyperglycemia in hospital and on the treatment of hyperglycemic patients at discharge,6,7 the efficacy and safety of which have been demonstrated in different multicenter studies.16,20,21 The most novel contribution lies in the strategy followed for implementing the protocol. In addition to involving the different organizational entities of the institution related to care and training, the most significant element, in our opinion, is the incorporation of the nurse consultant as a key figure in the program. Ward nurses are essential in the treatment of inpatient hyperglycemia and in the discharge process, particularly in surgical departments, where they are involved in the management of diabetes, being responsible for insulin administration, blood glucose monitoring, diet, the treatment of hypoglycemia and therapeutic education. In this context, it makes sense to acknowledge the relevance of the nurse consultant for hospitalized patients as an expert in diabetes management and as a model for the ward nurses.22,23
Thus, the effect exerted by the nurse consultant on diabetes management during hospital admission and in the discharge process is mediated by his or her influence upon the nurses and physicians responsible for the direct care of patients admitted to hospital due to conditions other than diabetes.
Although the role of the nurse is considered to be essential and central to the successful implementation of hyperglycemia management protocols in the hospital,7,24,25 solid evidence of this effectiveness is very limited.26,27
In the present study, the strategy used for implementing the protocol considerably improved the quality of care during hospital admission and after discharge. During hospitalization, and confirming the findings of previous studies,10,14 there was a dramatic increase in the use of basal-bolus insulin regimens, which was accompanied by a clear improvement in glycemic control as assessed by the mean preprandial and bedtime blood glucose levels. As expected, the optimization of glycemic control was associated with a reduction in severe hyperglycemic episodes and an increased frequency of hypoglycemic episodes. The frequency of hypoglycemic episodes was similar to that reported in the literature in non-critically ill patients, ranging from 1 to 33% depending on the glycemic control objectives and the treatment received.12,16,20 The intervention also allowed for the optimization of glycemic control three months after hospital discharge, without increasing readmissions related to diabetes control and treatment. This confirms the data from previous studies10,12,13,28 in that hospital admission is an opportunity for improving glycemic control through adequate planning and treatment reconciliation at discharge. Because of the characteristics of the study, the specific contribution of the nurse to the observed outcomes cannot be established, since it cannot be differentiated from the contributions of all the others involved in patient management. However, given the central role attributed to the nurse consultant in our program and the assessment of his or her contribution by the physicians and nurses in charge of patient care, we consider that the results obtained support the usefulness of the nurse consultant experienced in diabetes in the care of hospitalized patients with diabetes or hyperglycemia.
The results obtained should be considered within the limitations of the study. This was not a randomized trial but a study consisting of a retrospective control group and a prospective group, both set within the context of standard clinical practice, and comparing the new inpatient hyperglycemia management protocol against historical data. This makes it difficult to attribute the observed differences to the intervention or to define the specific contributions of the different participants in the intervention. However, since the study reflects standard clinical practice, we feel that it may be applicable to other centers seeking to improve inpatient hyperglycemia management.
ConclusionsThe current guides advise hospitals to develop standardized protocols based on basal-bolus insulin regimens for the management of hyperglycemia during hospital admission, though their implementation remains inadequate. The findings of this study show that a hyperglycemia management program based on the basal-bolus insulin regimen, and the incorporation of a nurse consultant with expertise in diabetes as central elements, allows most hospitalized patients with hyperglycemia to receive treatment with a basal-bolus regimen and improve glycemic control both during their hospital stay and after being discharged. Although specifically designed future studies are needed to determine the concrete contribution of the nurse consultant, the results obtained provide information supporting the usefulness of incorporating the nurse consultant in the care of hospitalized patients with diabetes. This measure may be applicable in other centers seeking to improve inpatient hyperglycemia management.
Financial supportAnalysis of the results received financial support provided in part by the grant “III Ayuda Guido Rufino de Investigación en Educación Terapéutica en Diabetes” of the Spanish Society of Diabetes. A nurse was contracted to replace the healthcare activities of the nurse consultant through a financial contribution from Sanofi in the context of an agreement with the Institut de Recerca of Hospital de la Santa Creu i Sant Pau.
Conflicts of interestThe authors of the manuscript declare the following potential conflicts of interest. AP has received personal fees for consultancy and/or conferences or travel reimbursement from Sanofi Aventis, Almirall, Novo Nordisk, Eli Lilly, MSD, Boehringer Ingelheim, Esteve, Novartis, Amgen, Menarini and Astra Zeneca.
The other authors declare that they have no potential conflicts of interest.
The authors thank Borja María Marina, Gabriel Gargallo and Ignasi Gich for their support in the development of the study, and for statistical advice. The authors also thank the several hundred physicians of the T1D Exchange clinic registry and the many people with diabetes in the United States who were surveyed regarding the most appropriate name for the parameter replacing eA1C. Special thanks are due to Amy Criego and Janet Davidson at the International Diabetes Center, who consistently insisted on the usefulness of using the word "management" instead of "control". We also thank the members of the medical and nursing teams of the hospital units of Hospital de Sant Pau, where the program was developed, and the colleagues of the Department of Endocrinology and Nutrition and the different management bodies of the hospital for their collaboration and support.
Please cite this article as: María MA, Ramos A, Martínez Roldán MJ, Pujol Giménez I, Pérez A. Implantación de un programa para el manejo de la hiperglucemia en la hospitalización con la incorporación de la enfermera consultora. Endocrinol Diabetes Nutr. 2019. https://doi.org/10.1016/j.endinu.2019.07.010