Fine-needle aspiration biopsy (FNAB) is the reference procedure for thyroid nodule evaluation. Its main limitations are inadequate samples, which should be less than 20%.
ObjectiveTo analyze the learning curve of the procedure by comparing the results of a non-experienced endocrinologist (endocrinologist 2) to those of an experienced one (endocrinologist 1).
Material and methodsSixty FNABs were analyzed from February to June 2016. Each endocrinologist made 2 punctures of every nodule in a random order. This order and the professional making every puncture were unknown to the pathologist who examined the samples.
ResultsEndocrinologist 1 had a higher percentage of diagnoses than endocrinologist 2 (82% vs. 72%, p=0.015). In the first 20 FNABs, the difference between both physicians was remarkable and statistically significant (80% vs. 50%, p=0.047). In the following 20 FNABs, the difference narrowed and was not statistically significant (90% vs. 65%, p=0.058). In the final 20 FNABs, the difference was minimal and not statistically significant (75% vs. 70%, p=0.723).
ConclusionsThe learning curve of ultrasound-guided FNAB may be completed in a suitable environment by performing it at least 60 times. Although the guidelines recommend at least 3 punctures per nodule, 2 are enough to achieve an accurate percentage of diagnoses.
La punción-aspiración con aguja fina (PAAF) es la técnica de referencia en la evaluación de los pacientes con nódulos tiroideos. Su mayor limitación son las muestras inadecuadas, que deberían ser menos del 20% de los casos.
ObjetivoAnalizar la curva de aprendizaje de dicha técnica de un endocrinólogo sin experiencia (endocrinólogo 2), comparando sus resultados con los obtenidos en los mismos nódulos por un colega experimentado (endocrinólogo 1).
Material y métodosSe realizaron 60 PAAF entre los meses de febrero y junio de 2016. Cada endocrinólogo realizó 2punciones de cada nódulo en un orden establecido aleatorizadamente. El orden de las punciones y el endocrinólogo que las realizaba eran datos desconocidos para la patóloga que analizó las muestras.
ResultadosEn el total de las PAAF, el endocrinólogo 1 tuvo un porcentaje de diagnósticos significativamente superior al endocrinólogo 2 (82 vs. 72%; p=0,015). En las primeras 20 PAAF la diferencia entre ambos fue notable y estadísticamente significativa (80 vs. 50%; p=0,047). En las siguientes 20 PAAF la diferencia se redujo y ya no tenía significación estadística (90 vs. 65%; p=0,058). Y en las últimas 20 la diferencia fue mínima y sin significación estadística (75 vs. 70%; p=0,723).
ConclusionesLa curva de aprendizaje de la eco-PAAF puede completarse en un entorno adecuado haciéndola un mínimo de 60 veces. Aunque las guías recomiendan al menos 3punciones por nódulo, 2son suficientes para conseguir un porcentaje adecuado de diagnósticos.
Fine-needle aspiration biopsy (FNAB) is the reference procedure for assessing patients with thyroid nodules. Initially described in 1934,1 its use became generalized after the favorable publications of Walfish2 and Gershengorn.3 Described in detail in numerous texts,4–7 all of its variants have in common that three to six punctures are performed8,9 with a 22 to 27G needle to obtain at least six groups of 10 follicular cells,10,11 the characteristics of which are analyzed microscopically.
The greatest limitation of FNAB are inadequate samples, which in expert hands occur in 2–20% of cases,12 although some authors suggest a more realistic rate of 15–25%.13 This continues to occur despite improvements that have reduced their incidence, such as use of ultrasound in its performance,14,15 standardization of different aspects of the procedure, including smear number and preparation,16 needle size17 and rinsing of the remnants. The presence of a pathologist who observes the samples at the site of puncture may also decrease this percentage.18
The learning curve of a procedure is the number of times it has to be performed until an adequate number of successes are achieved. Little is known about this curve in the case of FNAB: most of the few existing publications analyze improvements in the results of professionals with proven prior experience19,20 or who perform at the same time as FNAB aspiration of extrathyroid nodules21; or procedures far from the standard, such as computed tomography-guided thyroid aspiration.22
This was a prospective study to analyze the learning curve of FNAB of an endocrinologist with no experience, comparing his/her results to those obtained in the same nodules by an experienced colleague.
Patients and methodsThe Department of Endocrinology and Nutrition of the Complexo Hospitalario Universitario de Vigo has a weekly clinic that lists patients for whom FNAB is requested. Punctures are performed by an endocrinologist with 21 years of experience in the procedure. During the study period, an endocrinologist with no experience in performing FNAB also attended the procedure.
The punctures analyzed in this study were performed during eight clinic working days from 4 February to 30 June 2016. Patients were recruited through the hospital appointment service by order of request, and none of the authors knew these patients or the characteristics of their nodules until the day FNAB was performed.
Before performing the punctures analyzed, the more experienced endocrinologist (endocrinologist 1) performed complete FNABs on four patients and explained in detail to his colleague (endocrinologist 2) the characteristics of the procedure, divided into three parts: aspects prior to the puncture (patient placement, use of ultrasound equipment, marking of the puncture site, etc.), puncture method (angle of entry of the needle into the skin, visualization of the needle in ultrasound equipment, aspiration method) and post-aspiration issues (smearing of samples, rinsing of remnants from the needle, fixation).
Each endocrinologist performed two punctures of each nodule under ultrasound control in a randomly established order and following the procedure described in a previous publication of our group.23 Smears of each sample were identified with the letter A or B, also assigned at random. The pathologist who analyzed the samples was blinded to each physician and the order in which the punctures were performed.
No technical comments were made during the time each FNAB lasted. When the patient left the clinic, any relevant issues were discussed, questions were resolved, and any errors made in each of the three aspects of the procedure described above were corrected. The clinical history of the next patient was then reviewed, and the potential approaches and any technical issues considered of interest were analyzed. Immediately before patient entry into the clinic, the order in which punctures would be performed was decided at random.
The same pathologist separately analyzed and reported, according to the Bethesda classification, the two smears of each patient marked with the letter A and those marked with the letter B. The samples belonging to category 1 were interpreted as non-diagnostic, and those belonging to any other category (2, 3, 4, 5, or 6) as diagnostic.
All patients were informed in detail about the study purpose and the characteristics and risks of the procedure and signed an informed consent form.
Quantitative variables are given as mean ± standard deviation, and qualitative variables as percentage and 95% confidence interval (CI). Differences between percentages were analyzed using a Chi-square test.
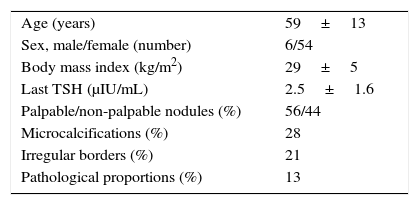
ResultsThe sample consisted of FNABs obtained from 60 individuals. Table 1 shows the characteristics of patients and their nodules. The mean number of punctures per day was eight (range, 6–10).
Characteristics of patients and nodules in which punctures were performed. Quantitative variables are given as the mean±standard deviation (SD). Pathological proportions: the ventrodorsal diameter of the nodule is greater than its latero-lateral diameter.
| Age (years) | 59±13 |
| Sex, male/female (number) | 6/54 |
| Body mass index (kg/m2) | 29±5 |
| Last TSH (μIU/mL) | 2.5±1.6 |
| Palpable/non-palpable nodules (%) | 56/44 |
| Microcalcifications (%) | 28 |
| Irregular borders (%) | 21 |
| Pathological proportions (%) | 13 |
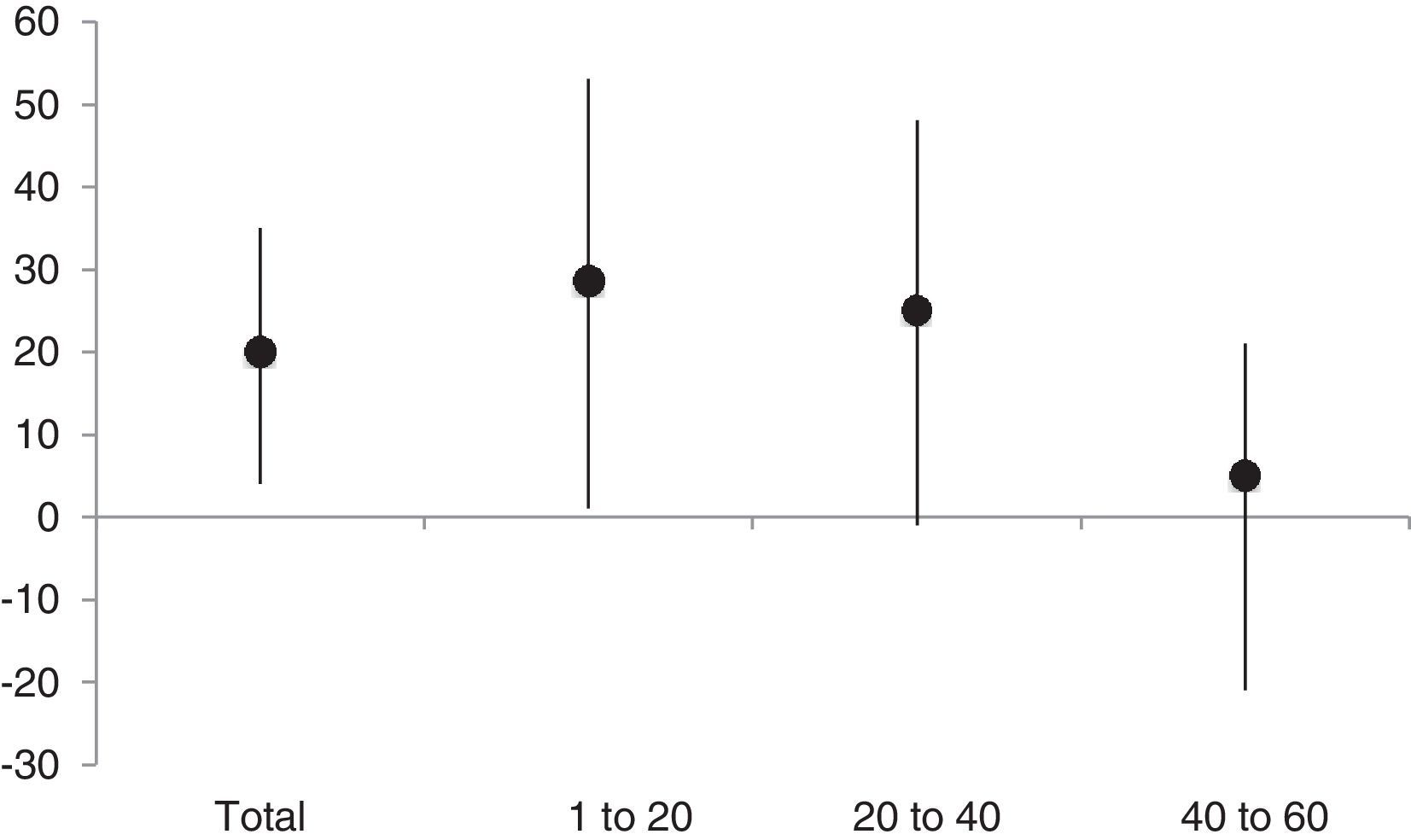
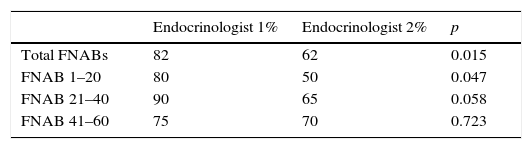
In the 60 FNABs performed, endocrinologist 1 had 82% and endocrinologist 2 had 62% of diagnoses. The difference between the two percentages was 20%, with a 95% CI (4; 35%) (p=0.015) (Fig. 1 and Table 2).
Percentage of diagnostic punctures of both endocrinologists.
| Endocrinologist 1% | Endocrinologist 2% | p | |
|---|---|---|---|
| Total FNABs | 82 | 62 | 0.015 |
| FNAB 1–20 | 80 | 50 | 0.047 |
| FNAB 21–40 | 90 | 65 | 0.058 |
| FNAB 41–60 | 75 | 70 | 0.723 |
p: probability of error; FNAB 1–20: the first 20 punctures; FNAB 21–40: the next 20 punctures; FNAB 41–60: the last 20 punctures performed; Total FNABs: all punctures performed; FNAB: fine-needle aspiration biopsy.
In the first 20 FNABs, endocrinologist 1 had 80% and endocrinologist 2 had 50% of diagnoses. The difference was 30%, with a 95% CI (1; 53%) (p=0.047) (Fig. 1 and Table 2). In the second 20 FNABs, endocrinologist 1 had 90% and endocrinologist 2 had 65% of diagnoses. The difference was 25%, with a 95% CI (∼1; 48%) (p=0.058) (Fig. 1 and Table 2). In the third 20 FNABs, endocrinologist 1 had 75% and endocrinologist 2, 70% of diagnoses. The difference was 5%, with a 95% CI (−21; 31%) (p=0.723) (Fig. 1 and Table 2).
In 11 patients, endocrinologist 1 performed the first two FNAB punctures. In these cases, this endocrinologist had 82% of diagnoses and endocrinologist 2 had 27%. The difference was 55%, with a 95% CI (13; 76%) (p=0.010). Endocrinologist 2 performed the first two FNAB punctures in 13 patients. In these cases, endocrinologist 1 had 77% and endocrinologist 2 had 69% of diagnoses. The difference was 8%, with a 95% CI (−25; 38%) (p=0.658).
Of the 60 patients analyzed, 26 had some ultrasonographic sign of malignancy as listed in Table 1 (microcalcifications, pathological size, or irregular borders). Endocrinologist 1 had 85% of diagnostic punctures in this group and 79% in all other patients, with a 95% CI (−24; 16%) (p=0.742). Endocrinologist 2 had 54% of diagnostic punctures in this group and 68% in all other patients, with a 95% CI (−10; 36%) (p=0.298).
DiscussionWe think that this is the first publication to report the learning curve of the reference procedure for FNAB. A 2015 publication stated that: «… there is no answer to the question […] on the number of UG-FNABs required for a person to achieve an adequate diagnostic rate».24
The sample analyzed corresponds to the requests for puncture of thyroid nodules performed by endocrinologists from a department of endocrinology and nutrition. These patients were referred to this department by their healthcare area physicians. We understand that the demographic characteristics of the sample and the characteristics of nodules analyzed would be similar to those seen in thyroid FNAB procedures performed at endocrinology clinics elsewhere.
Since early 2016, our department applied the 2015 American Thyroid Association criteria for FNAB of a thyroid nodule. One of its recommendations is to avoid diagnostic puncture of cysts, a circumstance that will probably increase the proportion of diagnostic tests because aspiration of cyst contents is a cause of 14% of non-diagnostic punctures.24
An advantage of our study is that the learning curve had as the control group the result of diagnostic punctures performed in the same nodules by an experienced endocrinologist, which could be used as the maximum target that could be achieved by somebody taught by the expert. In any case, the diagnostic rate of the experienced endocrinologist who participated in this study was above the minimum number recommended by the American Thyroid Association, which is 80%. This percentage was only lower than that value in the last 20 FNABs. A review of the FNABs of these nodules showed no significant differences in their characteristics as compared to the other nodules of the sample.
The order of punctures and the letter identifying each professional were randomly assigned in each FNAB. We think that the first measure avoids advantages for the one that performs the last punctures (and can see the way in which his/her colleague approaches the first ones), while the second measure prevents that the pathologist analyzing the samples can identify a priori who performed the puncture.
Each FNAB was performed with the knowledge and skills that each endocrinologist had at the time the patient entered the clinic. No comments or corrections were made during the procedure, but were detailed once the procedure had ended and the patient had left the room, at which time the clinical history of the next patient was reviewed, and the questions and conditions of the puncture to be performed were discussed. We thought that if this was not done, there would be a risk that the experienced professional would have directed, to some extent, each puncture by the inexperienced professional.
The percentage of diagnostic punctures in our sample was significant and markedly favorable to the expert endocrinologist, as was to be expected.
The difference in the diagnostic rates of the two physicians gradually decreased from the start to the end of the study. This suggests that the learning curve worked. This difference was very marked and statistically significant in the first third of the study, decreased in the second third, though with a p value close to 0.05, and was close to 0 in the last third. In addition (data not included in results), the last day of the study, five out of six punctures (83%) were diagnostic for both endocrinologists.
We suspect that performance of the first two punctures of each FNAB by the endocrinologist with more experience may provide an advantage to his colleague when performing their FNABs: watching the technique of his/her colleague may be advantageous for him/her. This was not the case: our data suggest that, at least under the conditions of our study, watching how an experienced endocrinologist performs punctures represents no advantage for his/her colleague.
Differences between the diagnostic rates of nodules with and without some ultrasonographic sign of malignancy were also analyzed to verify whether the proportion of diagnostic FNABs could be lower in the former as compared to the latter. This suspicion was not fulfilled either: differences were minimal, not significant, and not always favorable to nodules with no signs of malignancy.
A report published in 2000 suggested that the learning curve for cervical mass puncture under tomographic control was approximately 40 cases.22 Our data show that at least 60 USG-FNABs are needed, with two punctures in each FNAB, to complete the learning curve of this procedure. They also show that the process can be carried out in eight working days of 7hours. We think that no resident physician in the specialty should complete training without mastering this procedure, regardless of whether or not it is performed at their department.
Although the literature recommends performance of at least three punctures in each FNAB, in our study, each endocrinologist performed two. If the recommended number of punctures had been performed, the diagnostic rate would have undoubtedly increased. A recent publication that analyzed this issue reported proportions of non-diagnostic punctures of 34%, 23%, and 14% when 1, 2 and 3 punctures were made respectively.16
ConclusionsThe learning curve of the USG-FNAB procedure can be completed in a suitable environment with 60 FNABs of two punctures each. In an endocrinological clinic dedicated to this technique, the learning process may be completed in eight days. Although the guidelines recommend at least three punctures per nodule, two are sufficient to achieve an adequate diagnostic rate.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Penín M, Martín MÁ, San Millán B, García J. Curva de aprendizaje de la punción aspiración con aguja fina de tiroides. Endocrinol Diabetes Nutr. 2017;64:539–543.