To elaborate a diagnosis of the situation regarding the assistance in the Services and Units of Endocrinology and Nutrition (S°EyN) of the National Health System of Spain (SNHS) and to develop, based on the results obtained, proposals for improvement policies in the S°EyN.
Material and methodsCross-sectional descriptive study of the patients treated in the S°EyN departments of acute general hospitals of the SNHS in 2016. Data were obtained through RECALSEEN 2017, an “ad hoc” survey designed specifically for this purpose, and the Minimum Basic Data Set of discharges given by the S°EN of the SNHS (2015).
Results88 responses of S°EyN have been obtained forma total of 125 acute general hospitals of more than 200 beds installed in the SNHS (70% answers). 47% of the S°EyN respondents were services and 31% sections. The average of endocrinologists by S°EyN was 7.4±4.4, and the average rate of endocrinologists per 100,000 inhabitants was 2.3±1. The most relevant care activities were the consultation (average of 12.3 first consultations per thousand inhabitants and year), day hospital (median of 2000 sessions/year) and in-hospital consultations (median of 900 in-hospital consultations/year). 83% of S°EyNhad a Clinical Nutrition Unit. The number of dietitians, nutrition technicians and nutritionists in the Clinical Nutrition Unit was low. In relation to quality management, a large margin for improvement was detected; only 35% of S°EyN had a responsible of quality and 38% had implemented process management for those most frequent processes in the unit. There were notable differences in structure, resources and activity of S°EyN between Autonomous Communities.
ConclusionsRECALSEEN 2017 survey is a useful tool for the analysis of S°EyN. The remarkable variability found in the structure, activity and management indicators probably indicates significant differences and, therefore, a wide margin for improvement.
Elaborar un registro de situación de los Servicios y Unidades de Endocrinología y Nutrición (S°EyN) del Sistema Nacional de Salud (SNS) y valorar sus recursos asistenciales para desarrollar, a partir de los resultados obtenidos, propuestas de políticas de mejora en los S°EyN.
Material y métodosEstudio descriptivo transversal de los pacientes atendidos en los S°EyN en hospitales generales de agudos del SNS en 2016. Se utilizaron datos obtenidos mediante RECALSEEN 2017, una encuesta «ad hoc» diseñada específicamente para este fin y de las altas dadas por los S°EyN registradas en el CMBD del SNS (2015).
ResultadosDe un total de 125 hospitales generales de agudos de más de 200 camas instaladas del SNS español, se han obtenido 88 respuestas de los S°EyN, que representan el 70%. El 47% de los S°EyN que respondieron eran servicios y el 31% secciones. El promedio de endocrinólogos por S°EyN era de 7,4±4,4, siendo la tasa media de endocrinólogos por cada 100.000 habitantes de 2,3±1. Las actividades asistenciales más relevantes eran la consulta (promedio de 12,3 primeras consultas por mil habitantes y año), hospital de día (mediana de 2.000 sesiones/año) e interconsulta hospitalaria (mediana de 900 interconsultas/año). El 83% de los S°EyN incorporaban una Unidad de Nutrición Clínica. La dotación de dietistas, técnicos en nutrición y bromatólogos en las Unidades de Nutrición Clínica era baja. En relación con la gestión de la calidad se detectó un amplio margen de mejora; solamente un 35% de los S°EyN tenían responsable de calidad y el 38% había implantado una gestión por procesos para aquellos más frecuentemente atendidos por la unidad. Existen notables diferencias en estructura, recursos y actividad de los S°EyN entre Comunidades Autónomas.
ConclusionesLa encuesta RECALSEEN 2017 es útil para el análisis de los S°EyN. La notable variabilidad hallada en los indicadores de estructura, actividad y gestión probablemente indica relevantes diferencias y, por tanto, un amplio margen de mejora.
In the coming years, specialists in Endocrinology and Nutrition will face important challenges derived from the increasing prevalence of health problems inherent to the specialty and from the progressive technification of diagnostic and therapeutic processes.1–6 In addition, there is a marked tendency in developed western countries toward increased professionalism and self-regulation.7,8 In 2002, scientific organizations in Internal Medicine in both Europe and the United States jointly published “Medical Professionalism in the New Millennium: A Physician Charter”.3 In this context, RECALSEEN, a project of the Spanish Society of Endocrinology and Nutrition (Sociedad Española de Endocrinología y Nutrición [SEEN]), was conceived to determine the structure, organization and functioning of the Services and Units of Endocrinology and Nutrition (SUEN) of the Spanish National Health System (SNHS).
The RECALSEEN project, developed by the SEEN with the collaboration of the IMAS Foundation, follows in the wake of other similar projects developed by other scientific-medical bodies.9–11 Its objectives are: (1) to examine the state of patient care for endocrine and nutrition disorders in the SUEN; and (2) to develop proposals for improving the quality and efficiency of the care of these diseases. The RECALSEEN project has two main sources of information: the RECALSEEN Survey and the database of the Minimum Basic Data Set of the SNHS. The present article describes the results obtained from the survey concerning the professional and organizational aspects of Endocrinology and Nutrition, its structure and functioning, and assesses what is needed in order that a more adequate response to the existing challenges and the demands of patients, the healthcare system, and society in general can be provided.12
Material and methodsA cross-sectional descriptive study was made among the SUEN of the SNHS referring to 2016. The study considered the SUEN found in general acute care hospitals (therefore excluding hospitals from groups not falling within 1–5 of the classification of the Spanish Ministry of Health, Social Services and Equality [Ministerio de Sanidad, Servicios Sociales e Igualdad, MSSSI]13), and with 200 beds or more.
The study variables were compiled using an ad hoc web-based questionnaire accessed using individualized codes for each SUEN supervisor. The questionnaire consisted of 144 items. The Units were classified according to hospital size: type 1<500; type 2≥500 beds. The survey was compiled from March to September 2017. After completing the data collection period, the SUEN supervisors were asked for confirmation of data apparently out of range. All the data shown were obtained from the survey.
Statistical analysisQualitative variables were reported as frequency distributions (number of cases and percentages), and quantitative variables as the mean, median, and standard deviation (SD). The chi-squared test was used to compare qualitative variables, while the Student's t-test was used to compare quantitative variables. In all tests, the null hypothesis was rejected with an alpha error of <0.05. The STATA version 13.0 statistical package was used throughout.
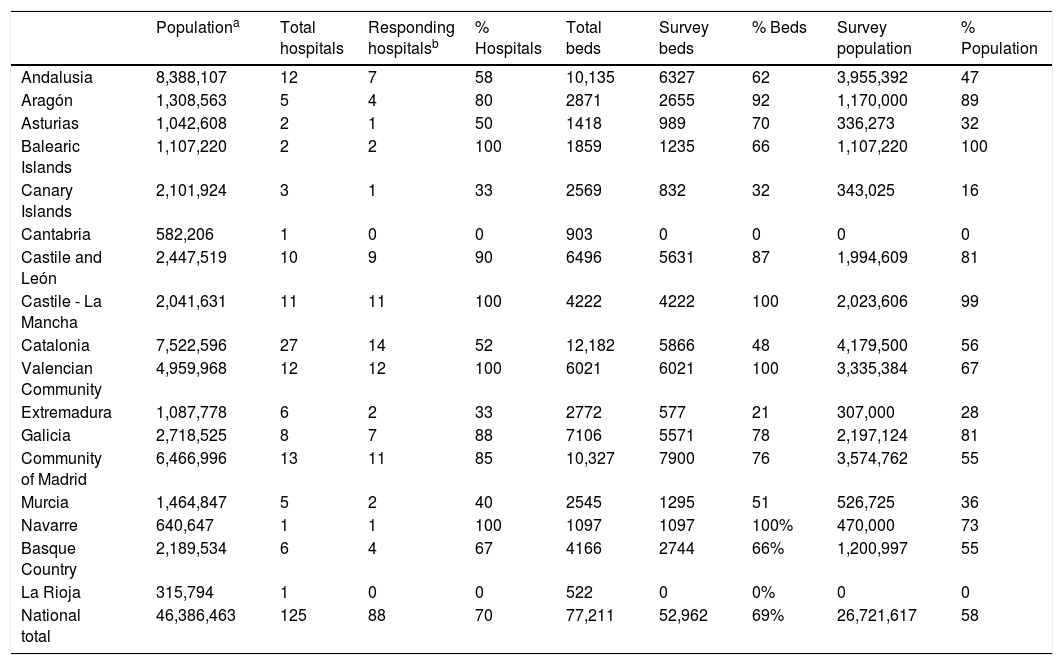
ResultsEighty-eight responses were obtained from the SUEN corresponding to a total of 125 general acute care hospitals (70%) of the SNHS with 200 or more beds. The response rate weighted against the number of beds was 69% and 58% of the total estimated population in the recruitment areas of the respective hospitals. Forty-two of the SUEN that answered the survey were located in hospitals with fewer than 500 beds and 46 in hospitals with 500 or more beds. The survey response rate varied among the different Autonomous Communities, and in 5 of them it was found to be less than 50% (Table 1).
Sample representativeness.
| Populationa | Total hospitals | Responding hospitalsb | % Hospitals | Total beds | Survey beds | % Beds | Survey population | % Population | |
|---|---|---|---|---|---|---|---|---|---|
| Andalusia | 8,388,107 | 12 | 7 | 58 | 10,135 | 6327 | 62 | 3,955,392 | 47 |
| Aragón | 1,308,563 | 5 | 4 | 80 | 2871 | 2655 | 92 | 1,170,000 | 89 |
| Asturias | 1,042,608 | 2 | 1 | 50 | 1418 | 989 | 70 | 336,273 | 32 |
| Balearic Islands | 1,107,220 | 2 | 2 | 100 | 1859 | 1235 | 66 | 1,107,220 | 100 |
| Canary Islands | 2,101,924 | 3 | 1 | 33 | 2569 | 832 | 32 | 343,025 | 16 |
| Cantabria | 582,206 | 1 | 0 | 0 | 903 | 0 | 0 | 0 | 0 |
| Castile and León | 2,447,519 | 10 | 9 | 90 | 6496 | 5631 | 87 | 1,994,609 | 81 |
| Castile - La Mancha | 2,041,631 | 11 | 11 | 100 | 4222 | 4222 | 100 | 2,023,606 | 99 |
| Catalonia | 7,522,596 | 27 | 14 | 52 | 12,182 | 5866 | 48 | 4,179,500 | 56 |
| Valencian Community | 4,959,968 | 12 | 12 | 100 | 6021 | 6021 | 100 | 3,335,384 | 67 |
| Extremadura | 1,087,778 | 6 | 2 | 33 | 2772 | 577 | 21 | 307,000 | 28 |
| Galicia | 2,718,525 | 8 | 7 | 88 | 7106 | 5571 | 78 | 2,197,124 | 81 |
| Community of Madrid | 6,466,996 | 13 | 11 | 85 | 10,327 | 7900 | 76 | 3,574,762 | 55 |
| Murcia | 1,464,847 | 5 | 2 | 40 | 2545 | 1295 | 51 | 526,725 | 36 |
| Navarre | 640,647 | 1 | 1 | 100 | 1097 | 1097 | 100% | 470,000 | 73 |
| Basque Country | 2,189,534 | 6 | 4 | 67 | 4166 | 2744 | 66% | 1,200,997 | 55 |
| La Rioja | 315,794 | 1 | 0 | 0 | 522 | 0 | 0% | 0 | 0 |
| National total | 46,386,463 | 125 | 88 | 70 | 77,211 | 52,962 | 69% | 26,721,617 | 58 |
Forty-seven percent of the SUEN that answered the survey were Services and 31% were Sections. The median number of endocrinologists assigned to each Service was 7, with a broad variability (mean: 7.4±4.5). Sixty-seven percent of the SUEN had hospitalization beds assigned, with a median of four beds per Unit, and 37.5% had day hospital facilities dependent upon the Service itself.
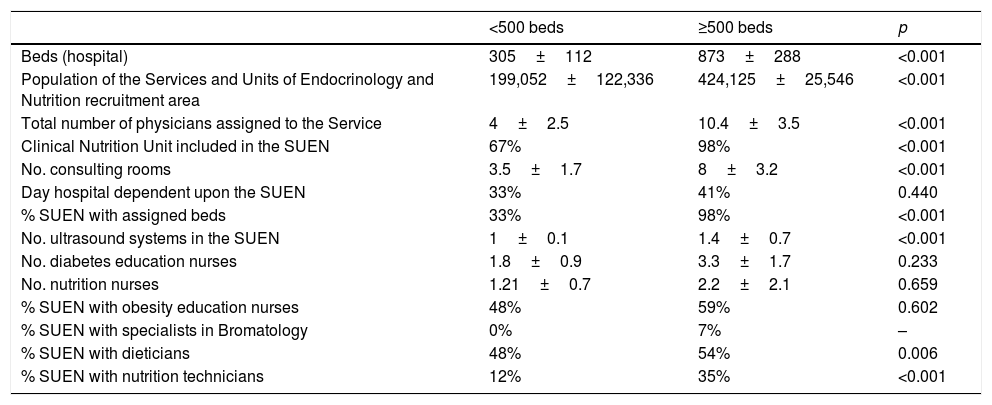
The SUEN had a median of two diabetes education nurses (mean: 2.6±1.6) and one nurse dedicated to nutrition; however, 35% of the SUEN did not have a nurse dedicated to nutrition. Twenty-six percent of the SUEN with an integrated Clinical Nutrition Unit (CNU) had no nurses dedicated to this activity. Overall, significant differences in structure and resources were found among the SUEN depending on the size of the hospital in which they were located (Table 2).
Structure of the Services and Units of Endocrinology and Nutrition according to hospital size.
| <500 beds | ≥500 beds | p | |
|---|---|---|---|
| Beds (hospital) | 305±112 | 873±288 | <0.001 |
| Population of the Services and Units of Endocrinology and Nutrition recruitment area | 199,052±122,336 | 424,125±25,546 | <0.001 |
| Total number of physicians assigned to the Service | 4±2.5 | 10.4±3.5 | <0.001 |
| Clinical Nutrition Unit included in the SUEN | 67% | 98% | <0.001 |
| No. consulting rooms | 3.5±1.7 | 8±3.2 | <0.001 |
| Day hospital dependent upon the SUEN | 33% | 41% | 0.440 |
| % SUEN with assigned beds | 33% | 98% | <0.001 |
| No. ultrasound systems in the SUEN | 1±0.1 | 1.4±0.7 | <0.001 |
| No. diabetes education nurses | 1.8±0.9 | 3.3±1.7 | 0.233 |
| No. nutrition nurses | 1.21±0.7 | 2.2±2.1 | 0.659 |
| % SUEN with obesity education nurses | 48% | 59% | 0.602 |
| % SUEN with specialists in Bromatology | 0% | 7% | – |
| % SUEN with dieticians | 48% | 54% | 0.006 |
| % SUEN with nutrition technicians | 12% | 35% | <0.001 |
SUEN: Departments and Units of Endocrinology and Nutrition.
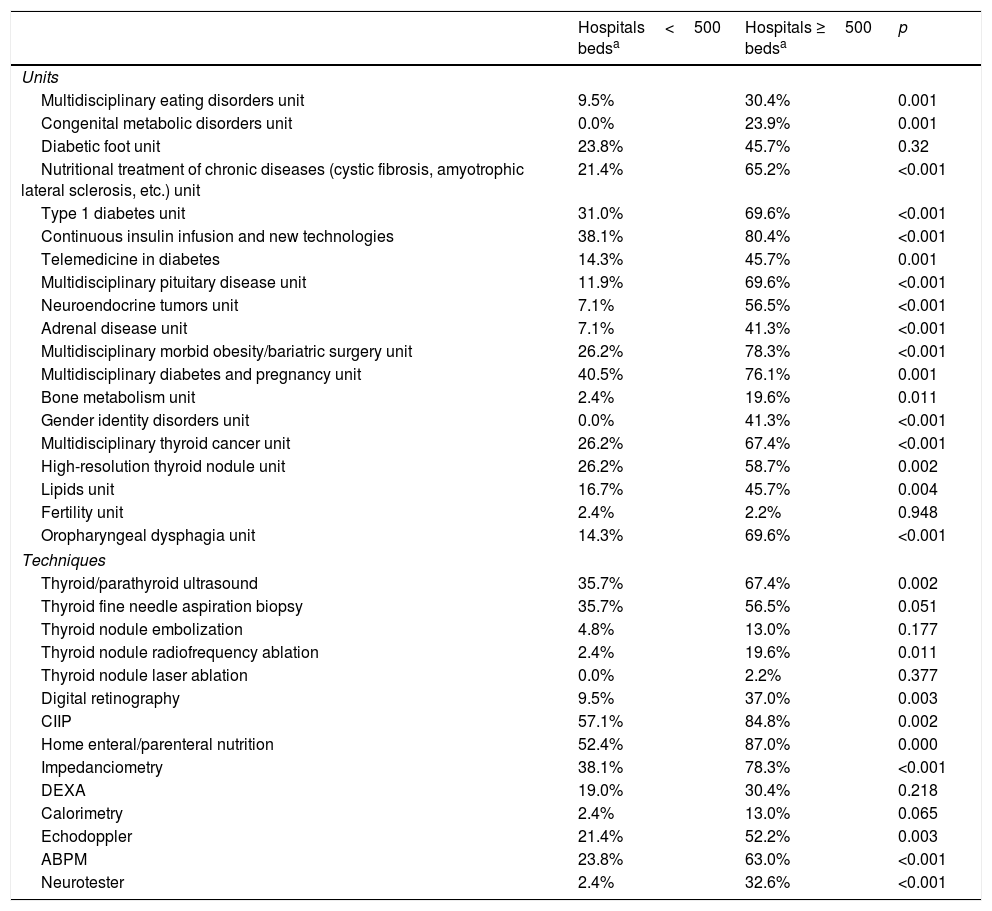
More than 50% of the SUEN had specific units for type 1 diabetes (51.1%), morbid obesity (53.4%), and diabetes and pregnancy (59.1%). Pituitary disease units were found in 42% of the SUEN, thyroid cancer units in 47.7%, high-resolution thyroid nodule units in 43.2%, and multidisciplinary eating disorder units in 26.1%. With respect to the techniques used, over 50% of the SUEN performed thyroid ultrasound (52.3%), continuous insulin infusion pump (CIIP) programs were present in 71.6%, home enteral and parenteral nutrition was provided by 53% and 44%, respectively, and impedanciometry was performed in 59.1%. Fine needle aspiration biopsy (FNAB) of the thyroid gland was performed by 46.6% of the SUEN. There were significant differences in the service portfolios of the SUEN in hospitals with fewer versus more than 500 beds (Table 3).
Service portfolio of the Departments and Units of Endocrinology and Nutrition according to hospital size.
| Hospitals<500 bedsa | Hospitals ≥500 bedsa | p | |
|---|---|---|---|
| Units | |||
| Multidisciplinary eating disorders unit | 9.5% | 30.4% | 0.001 |
| Congenital metabolic disorders unit | 0.0% | 23.9% | 0.001 |
| Diabetic foot unit | 23.8% | 45.7% | 0.32 |
| Nutritional treatment of chronic diseases (cystic fibrosis, amyotrophic lateral sclerosis, etc.) unit | 21.4% | 65.2% | <0.001 |
| Type 1 diabetes unit | 31.0% | 69.6% | <0.001 |
| Continuous insulin infusion and new technologies | 38.1% | 80.4% | <0.001 |
| Telemedicine in diabetes | 14.3% | 45.7% | 0.001 |
| Multidisciplinary pituitary disease unit | 11.9% | 69.6% | <0.001 |
| Neuroendocrine tumors unit | 7.1% | 56.5% | <0.001 |
| Adrenal disease unit | 7.1% | 41.3% | <0.001 |
| Multidisciplinary morbid obesity/bariatric surgery unit | 26.2% | 78.3% | <0.001 |
| Multidisciplinary diabetes and pregnancy unit | 40.5% | 76.1% | 0.001 |
| Bone metabolism unit | 2.4% | 19.6% | 0.011 |
| Gender identity disorders unit | 0.0% | 41.3% | <0.001 |
| Multidisciplinary thyroid cancer unit | 26.2% | 67.4% | <0.001 |
| High-resolution thyroid nodule unit | 26.2% | 58.7% | 0.002 |
| Lipids unit | 16.7% | 45.7% | 0.004 |
| Fertility unit | 2.4% | 2.2% | 0.948 |
| Oropharyngeal dysphagia unit | 14.3% | 69.6% | <0.001 |
| Techniques | |||
| Thyroid/parathyroid ultrasound | 35.7% | 67.4% | 0.002 |
| Thyroid fine needle aspiration biopsy | 35.7% | 56.5% | 0.051 |
| Thyroid nodule embolization | 4.8% | 13.0% | 0.177 |
| Thyroid nodule radiofrequency ablation | 2.4% | 19.6% | 0.011 |
| Thyroid nodule laser ablation | 0.0% | 2.2% | 0.377 |
| Digital retinography | 9.5% | 37.0% | 0.003 |
| CIIP | 57.1% | 84.8% | 0.002 |
| Home enteral/parenteral nutrition | 52.4% | 87.0% | 0.000 |
| Impedanciometry | 38.1% | 78.3% | <0.001 |
| DEXA | 19.0% | 30.4% | 0.218 |
| Calorimetry | 2.4% | 13.0% | 0.065 |
| Echodoppler | 21.4% | 52.2% | 0.003 |
| ABPM | 23.8% | 63.0% | <0.001 |
| Neurotester | 2.4% | 32.6% | <0.001 |
CIIP: continuous insulin infusion pump; DEXA: dual-energy X-ray absorptiometry (bone densitometry); ABPM: ambulatory blood pressure monitoring; SUEN: Departments and Units of Endocrinology and Nutrition.
A high degree of collaboration of the SUEN with other Units in both the in-hospital and primary care setting was observed. With regard to primary care, 94% of the SUEN reported having some structured relationship; in 86% of the Units this was based on joint referral protocols, while 69% reported communication via e-mail and 47% by mobile phone. The endocrinologist visited the primary care center in 34% of the Units, and 10% held videoconference sessions with primary care.
With regard to the other services of the hospital, 66% of the SUEN had developed an interconsultation service or unit,14 the median in such SUEN being one endocrinologist dedicated full-time to this activity. In the hospitals with more than 500 beds, the prevalence of multidisciplinary units centered on eating disorders (30%), pituitary disease (69%), morbid obesity (78%), diabetes and pregnancy (76%), and thyroid cancer (67%) was greater than in smaller hospitals (Table 3).
Clinical Nutrition UnitsIn 83% of the cases, the Clinical Nutrition Unit (CNU) was incorporated within the SUEN; this percentage increased to 98% in hospitals with 500 or more beds. Fifty-three percent of the SUEN with an integrated CNU had dieticians working in the Unit; 26% had nutrition technicians; and only three SUEN with an integrated CNU reported the presence of specialists in Bromatology. The percentage of hospitals performing nutritional assessment was 56%, and increased to 66% in those SUEN with an integrated CNU. In turn, 81% of the SUEN with an integrated CNU offered home nutrition services.
ActivityDischarges from Endocrinology and Nutrition gradually decreased over the study period, from 10,656 in 2007 to 8698 in 2015. In terms of frequency, this represents a relevant reduction in rate from 29 discharges per 1000 inhabitants and year in 2007 to 23 in 2015 (-20%). In the SUEN with assigned hospital beds, the mean annual discharges totalled 71 patients a year (20 admissions per 100,000 inhabitants and year), with a mean stay of 5±2 days, decreasing from 7.4 days in 2007 to 6 days in 2015. The mean number (year 2016) of day hospital sessions was 1220, with very broad variations, as was also shown by hospital interconsultations (1592) and outpatient consultations, where the SUEN registered 3600 (± 1800) first consultations, with a visiting rate of 12 (± 5.2) per 1000 inhabitants and year, an average delay of 34 (± 30) days, and a successive: first visit ratio of 3.3 (± 1.4). Seventy-two percent of the SUEN had developed forms of non-face-to-face consultation, with an average of 681 such consultations per year.
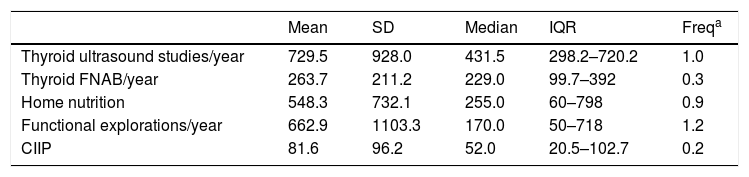
Table 4 shows the number of explorations per Unit (referring to those Units that perform the technique), as well as the frequency corresponding to each technique (estimated for the whole population included in the sample), for a selected number of techniques (those most commonly used by the SUEN).
Activity and frequency of Endocrinology techniques.
| Mean | SD | Median | IQR | Freqa | |
|---|---|---|---|---|---|
| Thyroid ultrasound studies/year | 729.5 | 928.0 | 431.5 | 298.2–720.2 | 1.0 |
| Thyroid FNAB/year | 263.7 | 211.2 | 229.0 | 99.7–392 | 0.3 |
| Home nutrition | 548.3 | 732.1 | 255.0 | 60–798 | 0.9 |
| Functional explorations/year | 662.9 | 1103.3 | 170.0 | 50–718 | 1.2 |
| CIIP | 81.6 | 96.2 | 52.0 | 20.5–102.7 | 0.2 |
CIIP: continuous insulin infusion pump; SD: standard deviation; FNAB: fine needle aspiration biopsy; IQR: interquartile range.
There was a disappointingly low level of research activity among the SUEN that responded to the survey. Twenty-four percent of the SUEN had staff dedicated to research, with a median of 1.5 professionals dedicated on a full-time basis. In turn, 48% of the Units had active research projects in the context of competitive national or international public tenders. Likewise, 62.5% of the SUEN were involved in clinical trials, with a median of three trials, and 56% participated in some of the national disease registries (thyroid cancer, multiple endocrine neoplasms, neuroendocrine tumors, continuous insulin infusion, pituitary adenomas).
Fifty-one percent of the SUEN that answered the survey were accredited for resident training (MIR). The accredited Units had an average of one resident in training per specialty year. In turn, 62% of the Units provided training for dieticians.
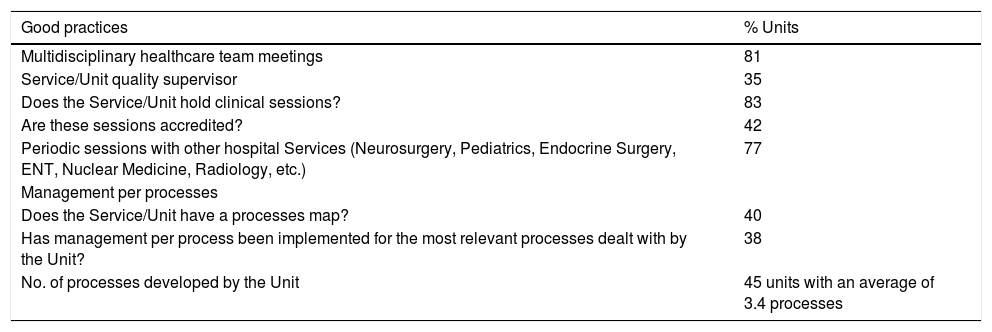
Good practicesEighty-one percent of the SUEN held multidisciplinary meetings with the care team; 77% held periodic sessions with other hospital Services; and 83% held clinical sessions on a regular basis. However, only 42% of these were accredited, there being room for improvement in the designation of quality supervisors (recorded in only 35% of the SUEN) and in process implementation (only 38% reported this resource for the processes most frequently dealt with by the Unit) (Table 5).
Good practices in Departments and Units of Endocrinology and Nutrition.
| Good practices | % Units |
|---|---|
| Multidisciplinary healthcare team meetings | 81 |
| Service/Unit quality supervisor | 35 |
| Does the Service/Unit hold clinical sessions? | 83 |
| Are these sessions accredited? | 42 |
| Periodic sessions with other hospital Services (Neurosurgery, Pediatrics, Endocrine Surgery, ENT, Nuclear Medicine, Radiology, etc.) | 77 |
| Management per processes | |
| Does the Service/Unit have a processes map? | 40 |
| Has management per process been implemented for the most relevant processes dealt with by the Unit? | 38 |
| No. of processes developed by the Unit | 45 units with an average of 3.4 processes |
ENT: Ear, Nose and Throat (Otolaryngology); SUEN: Departments and Units of Endocrinology and Nutrition.
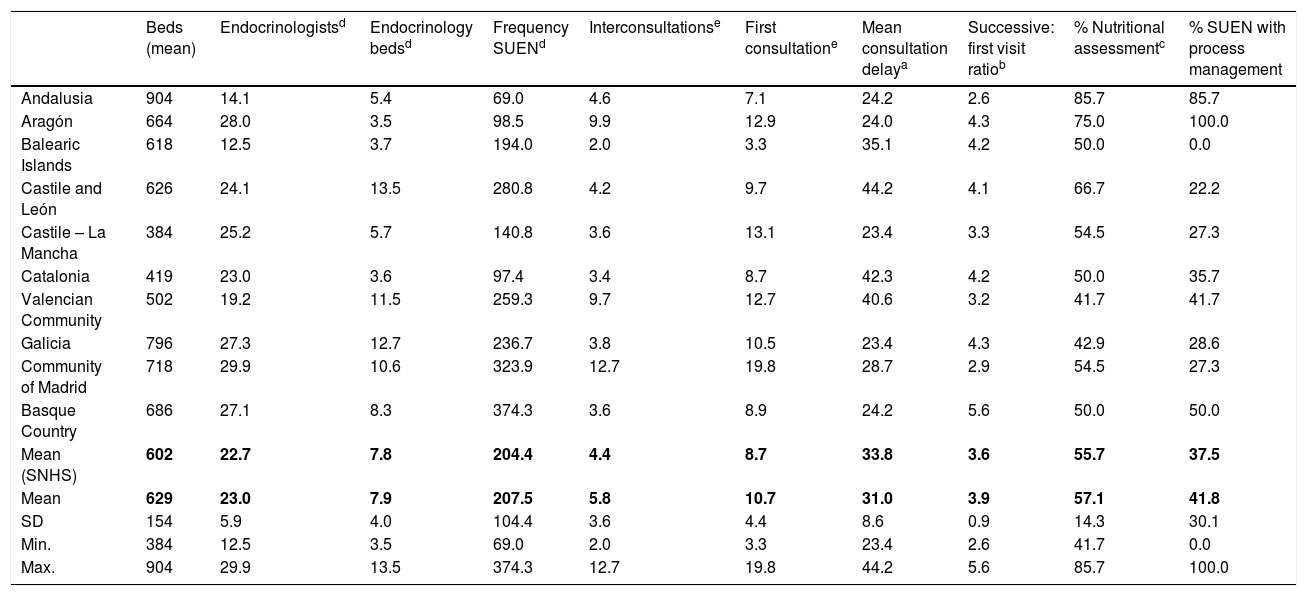
Significant differences were recorded in Endocrinology resources and activities among the Health Departments of the different Spanish Autonomous Communities. In two of them (Cantabria and La Rioja), no center answered the survey. Table 6 compares some resource indicators (acute care hospital beds dedicated to Endocrinology and endocrinologists per million inhabitants), visiting frequency (hospital, consultations, interconsultations), mean stay in the SUEN, mean consultation delay, and some quality indicators.
Comparison of indicators between the health services of the different Spanish Autonomous Communities.
| Beds (mean) | Endocrinologistsd | Endocrinology bedsd | Frequency SUENd | Interconsultationse | First consultatione | Mean consultation delaya | Successive: first visit ratiob | % Nutritional assessmentc | % SUEN with process management | |
|---|---|---|---|---|---|---|---|---|---|---|
| Andalusia | 904 | 14.1 | 5.4 | 69.0 | 4.6 | 7.1 | 24.2 | 2.6 | 85.7 | 85.7 |
| Aragón | 664 | 28.0 | 3.5 | 98.5 | 9.9 | 12.9 | 24.0 | 4.3 | 75.0 | 100.0 |
| Balearic Islands | 618 | 12.5 | 3.7 | 194.0 | 2.0 | 3.3 | 35.1 | 4.2 | 50.0 | 0.0 |
| Castile and León | 626 | 24.1 | 13.5 | 280.8 | 4.2 | 9.7 | 44.2 | 4.1 | 66.7 | 22.2 |
| Castile – La Mancha | 384 | 25.2 | 5.7 | 140.8 | 3.6 | 13.1 | 23.4 | 3.3 | 54.5 | 27.3 |
| Catalonia | 419 | 23.0 | 3.6 | 97.4 | 3.4 | 8.7 | 42.3 | 4.2 | 50.0 | 35.7 |
| Valencian Community | 502 | 19.2 | 11.5 | 259.3 | 9.7 | 12.7 | 40.6 | 3.2 | 41.7 | 41.7 |
| Galicia | 796 | 27.3 | 12.7 | 236.7 | 3.8 | 10.5 | 23.4 | 4.3 | 42.9 | 28.6 |
| Community of Madrid | 718 | 29.9 | 10.6 | 323.9 | 12.7 | 19.8 | 28.7 | 2.9 | 54.5 | 27.3 |
| Basque Country | 686 | 27.1 | 8.3 | 374.3 | 3.6 | 8.9 | 24.2 | 5.6 | 50.0 | 50.0 |
| Mean (SNHS) | 602 | 22.7 | 7.8 | 204.4 | 4.4 | 8.7 | 33.8 | 3.6 | 55.7 | 37.5 |
| Mean | 629 | 23.0 | 7.9 | 207.5 | 5.8 | 10.7 | 31.0 | 3.9 | 57.1 | 41.8 |
| SD | 154 | 5.9 | 4.0 | 104.4 | 3.6 | 4.4 | 8.6 | 0.9 | 14.3 | 30.1 |
| Min. | 384 | 12.5 | 3.5 | 69.0 | 2.0 | 3.3 | 23.4 | 2.6 | 41.7 | 0.0 |
| Max. | 904 | 29.9 | 13.5 | 374.3 | 12.7 | 19.8 | 44.2 | 5.6 | 85.7 | 100.0 |
Mean values in boldface.
The key issues facing the next generation of endocrinologists will be those of a specialty that is permanently and rapidly changing within the context of a innovating biotechnological environment, in both the research and clinical practice spheres. In its translational aspect, big-data management, new technologies applied to information management and transmission, the proliferation of consensuses, recommendations and clinical guidelines, omnipresent “evidence-based medicine”, and the increasingly important role of patients in decision-making and the self-care of their disease appear to be critical areas for improving the efficiency and effectiveness of specialists in Endocrinology and Nutrition.
One significant observation is the disappointingly low presence of endocrinologists per million inhabitants in two Spanish Autonomous Communities (Andalusia and the Balearic Islands, with 14.1 and 12.5 endocrinologists per million inhabitants, respectively), while in the other Communities the number comes close to the global average (23±5.6 endocrinologists per million inhabitants). This can be interpreted in the context of health policy decision-making (placing greater emphasis on specialists in Internal Medicine, who are more “polyvalent”, in smaller district hospital centers). The lesser availability of endocrinologists may give rise to inter-territorial imbalances and inequities, by obliging complex endocrinological patients not amenable to follow-up by other specialists (type 1 diabetes, pituitary tumors, multiple endocrine neoplasms, congenital metabolic disorders, thyroid cancer, etc.) to be obliged to travel to more distant centers in order to receive adequate care.
It is important to emphasize certain ambulatory care services, such as day hospitals, which were present in 37.5% of the SUEN, and which probably explain the progressive decrease in the number of SUEN admissions. The development of such services implies a degree of improvement in the care of patients in this specialty. Mention should also be made of the incorporation of diagnostic and therapeutic techniques to the specialty, as regards both new technologies (continuous insulin infusion) and home nutrition. In the case of thyroid nodule studies, ultrasound and FNAB in turn allow for a faster and more efficient diagnosis. The gradual incorporation of these techniques to most SUEN also entails a significant margin for improvement, since there are important variations in both the mean number of techniques performed by the SUEN and in frequency per area.
The results of our survey reflect the important development of joint work with the primary care teams, and although marked diversity is observed, mention should be made of the existence in larger hospitals of multidisciplinary units led by specialists in our field, targeted to high-complexity medical problems that need to be addressed in a tertiary setting. Such units should be promoted, and their development remains a topic for improvement in the SUEN (Table 3).
In addition, Clinical Nutrition Units are becoming increasingly important due to the relevance of the management of malnutrition in the hospital and community setting with reference to complex chronic patients and patients with cancer. Likewise, a marked aging of the patients seen in the hospital admission wards of the different medical specialties has been reported.15,16 These patient groups have specific requirements, including attention to their nutritional status,17,18 and are characterized by frailty and vulnerability that imply risks during hospitalization, which may worsen if not adequately treated, and that can lead to further readmissions.18–20 In this context, the Clinical Nutrition Unit is seen as a supporting unit for the medical and surgical services of the hospital, and an essential element for improving patient quality of life and for avoiding readmissions.18,21 This aspect is a relevant area for improvement in hospitals with fewer than 500 beds. At present, the growth of the specialty is largely attributable to the demand for care generated by hospital clinical nutrition, and in this regard the number of hospitals with nutrition units is gradually increasing.22
Lastly, caution is required regarding the reliability of the estimates regarding the differences between Autonomous Communities. Such reliability depends on the representativeness of the sample corresponding to each Community (the greater the percentage survey response rate, the greater the reliability of the results obtained) and the possible presence of bias (e.g., in relation to the size of the hospital in which the SUEN is located). However, since the study sample was large, it seems reasonable on the basis of the available data to affirm that there are probably significant differences in resources and activities in our specialty among the different Autonomous Communities.
ConclusionsThe RECALSEEN 2017 survey discloses relevant aspects of the organization, structure and management of Services and Units of Endocrinology and Nutrition. The average number of endocrinologists per million inhabitants is quite homogeneous throughout the SNHS, with the exception of Andalusia and the Balearic Islands, where the presence of these professionals is markedly lower. The main activity of endocrinologists continues to focus on the outpatient clinic, together with increasing activity at the day hospital and, particularly, hospital interconsultations. The great majority of the hospitals have a Clinical Nutrition Unit integrated in the SUEN, though the human resources are limited. A progressive development of specific units is seen (type 1 diabetes and new technologies, gestational diabetes, high-resolution thyroid nodule units), together with a greater participation in multidisciplinary units (bariatric surgery, eating disorders, gender dysphoria). Lastly, the wide variability observed in the structural, activity and management indicators of these Units probably reflects important differences, and therefore suggests that there is considerable room for improvement.
Financial supportThe RECALSEEN survey has benefited from an unconditional grant from Laboratorios Menarini.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Botella Romero F, Elola Somoza FJ, Navarro González E, Fernández Pérez C, Bernal Sobrino JL, Bretón Lesmes I. RECALSEEN. La atención al paciente en las unidades de Endocrinología y Nutrición del Sistema Nacional de Salud. Endocrinol Diabetes Nutr. 2019;66:425–433.