Diabetes mellitus (DM) is one of the most prevalent chronicdiseases and has a significant health and social impact. Strict control of blood glucose levels and other risk factors for vascular disease (VD) reduces complications and mortality and is related to the quality of care received. Although care should be interdisciplinary, based on the coordination of primary care (PC) and hospital care (HC), little information is available on the effectiveness of the different existing intervention models.
ObjectiveTo assess, in a population with DM from a healthcare area, the impact on health, quality of care, and effectiveness in the use of resources of a specific model of shared management of patients with DM (Instrument for Evaluation of Models of Chronic Care in Diabetes Mellitus; IEMAC-DM).
Patients and methodsA quasi-experimental before-after intervention study in patients with DM in the Cádiz-San Fernando Healthcare Area (Andalusia, Spain) that allows for identifying the capacity of the program to improve the quality indicators both in the whole population with DM and in that referred to HC. For this, a working group consisting of healthcare professionals of different profiles and care levels was set up. An initial self-assessment was done using the IEMAC-DM tool and, after analysis of the preliminary results, improvement strategies were established and implemented. Finally, the clinical and resource management results were assessed before and two years after the implementation of the model.
ResultsDuring the study period, no significant changes were seen in process indicators related to laboratory practices or examinations in the health area. The proportion of patients with acceptable metabolic control [glycosylated hemoglobin (HbA1c) level < 8%] was 49% in 2015 and 45% in 2017. The number of admissions related to acute myocardial infarction (AMI) and stroke remained constant, but there was an increase in the standardized ratio of major lower limb amputations (1.5 vs. 1.9). Of the 295 patients referred from PC to HC, the proportion of adequate referrals increased from 40% in 2015 to 76% in 2017 (P = .001). In the referred patients, a significant improvement was seen in the mean difference in glycosylated hemoglobin levels (HbA1c; 1.14 ± 1.73%; 95% CI: 0.73–1.55; P = .0001) and cholesterol (11.28 ± 40 mg/dL; 95% CI: 2.07–20.48; P = .012).
ConclusionsThis study shows that an intervention based on a chronicity care model adapted to patients with DM improves certain aspects related to the quality of care and the degree of metabolic control. Improving health outcomes will require long-term evaluation and, probably, other additional interventions.
La diabetes mellitus (DM) es una de las patologías crónicas más prevalentes en nuestro medio con un importante impacto sanitario y social. El control estricto de la glucemia y de otros factores de riesgo de enfermedad vascular (EV) reduce las complicaciones y mortalidad y se relaciona con la calidad de la atención recibida. Aunque ésta debe ser interdisciplinar, basada en la coordinación entre Atención Primaria (AP) y Atención Hospitalaria (AH), existe escasa información sobre la efectividad lograda por los diferentes modelos de intervención existentes.
ObjetivoEvaluar en una población con DM de un área sanitaria el impacto en salud, calidad asistencial y efectividad en el uso de recursos de un modelo específico de gestión compartida para el paciente con DM (Instrumento de Evaluación de Modelos de Atención ante la Cronicidad en Diabetes Mellitus; IEMAC-DM).
Material y métodosEstudio de intervención cuasi experimental, antes-después, en pacientes con DM en el Área Sanitaria Cádiz-San Fernando (Andalucía, España) que permite identificar la capacidad del programa para mejorar los indicadores de calidad tanto en toda la población con DM como en la derivada al AH. Para ello, se constituyó un grupo de trabajo con profesionales sanitarios de distintos perfiles y niveles asistenciales. La autoevaluación inicial se realizó mediante la herramienta IEMAC-DM y tras el análisis de resultados preliminares se establecieron e implantaron estrategias de mejora. Finalmente, se evaluaron los resultados clínicos y de gestión de recursos antes y a los dos años de la implantación del modelo.
ResultadosDurante el período de estudio, los indicadores de proceso relacionados con prácticas analíticas o exploraciones en el área sanitaria no sufrieron variaciones significativas. El porcentaje de pacientes con aceptable control metabólico [hemoglobina glicosilada (HbA1c) < 8%] fue del 49% en 2015 y del 45% en 2017. El número de ingresos relacionados con Infarto Agudo de Miocardio (IAM) y Accidente Vascular Cerebral (AVC) se mantuvo constante pero hubo un incremento en la razón estandarizada de amputaciones mayores de miembros inferiores (MMII; 1,5 vs 1,9). De los 295 pacientes derivados desde AP a AH, el porcentaje de derivación adecuada se elevó del 40% en 2015 al 76% en 2017 (P = ,001). En la totalidad del grupo derivado hubo una mejora significativa en la diferencia media de los niveles de HbA1c (−1,14 ± 1,73%; IC95%: 0,73–1,55; P = ,0001] y de colesterol (−11,28 ± 40 mg/dl; IC95%: 2,07–20,48; P = ,012)].
ConclusionesEn el presente estudio demostramos que una intervención basada en un modelo de atención a la cronicidad adaptado a pacientes con DM consigue mejorar aspectos—subrogados-relacionados con la calidad asistencial y grado de control metabólico. La mejora de resultados en salud requerirá evaluación a largo plazo y, casi con toda probabilidad, otras intervenciones adicionales.
Diabetes mellitus (DM) is a chronic condition with a high health, economic, and social impact.1–4 It is associated to a high risk of vascular disease (VD) both in itself and because of its frequent association with other risk factors.1 Over time, a high proportion of patients with DM experience macrovascular complications such as acute myocardial infarction, cerebrovascular accident, and distal arterial disease, and microvascular complications such as diabetic retinopathy and diabetic nephropathy.2 Complications derived from DM decrease life expectancy and quality, and their severity is closely related to age, time since onset of DM, degree of metabolic control, and quality of the care received.5,6 Based on the above, the Andalusian Health Service (SAS) considers diabetes a priority problem. As a result of this consideration, the Andalusian Comprehensive Plan for Diabetes Mellitus (PIDMA) and the Integrated Care Process (PAI) for DM were created in 2003—and subsequently consolidated7,8—their priorities include health promotion, early diagnosis, prevention of complications, and promotion of a proactive approach of patients to their condition that allows for continued improvement. Actions promoted include healthcare integration and multidisciplinary team work, efficient referral of patients from primary care (PC) to hospital care (HC), and promotion of communication skills.
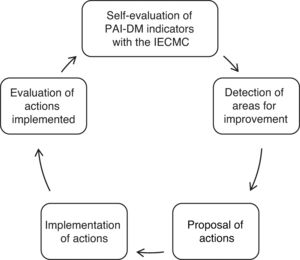
However, despite the efforts made to reduce the impact of DM, the Di@bet.es study9 shows that both DM prevalence and complication rates10 and poor metabolic control11 continue to be significantly high in Spain. In our setting (healthcare area of Hospital Universitario Puerta del Mar de Cádiz [HUPM]), over 50% of patients with type 2 DM (T2DM) have poor metabolic control (HbA1c ≥ 8%), and approximately 60% have two or more risk factors for VD in addition to DM itself. Poor metabolic control associated to the high prevalence of risk factors for VD undoubtedly contributes to the great impact of chronic complications in our area.10,11 Because of the recognized value of implementation of coordinated and strategic activities in diabetes care,12–14 an Advanced Diabetes Center (ADC) staffed by PC and HC physicians and nurses (Department of Endocrinology and Nutrition of the HUPM) was created in 2014 to identify the degree of adaptation of our organizational setting to the comprehensive care of patients with DM as disseminated by the PIDMA and PAI-DM. The value of the ADC was assessed using the Instrument for Evaluation of Care Models for Chronic Diabetes Mellitus (IECMC-DM),15 which allows healthcare organizations to assess their approach to chronic disease while offering a map of actions to improve care for patients with DM.
The purpose of this study was to analyze the impact of implementation of this model, IECMC-DM, on the quality of care of patients with DM in a hospital healthcare area.
Material and methodsThis is a quasi-experimental, interventional study to assess the results of the process and health after implementation of a shared management model (IECMC-DM) in patients with DM in a hospital healthcare area.
Study populationThe study enrolled all patients over 18 years of age diagnosed with DM attending the Cádiz-San Fernando healthcare area (10 PC health centers; 234,000 inhabitants) of the public health system of Andalusia with their data recorded in the computer systems (Diraya and Diabaco). Patients with insufficient data, institutionalized residents, on temporary stay and with computer record errors were excluded.
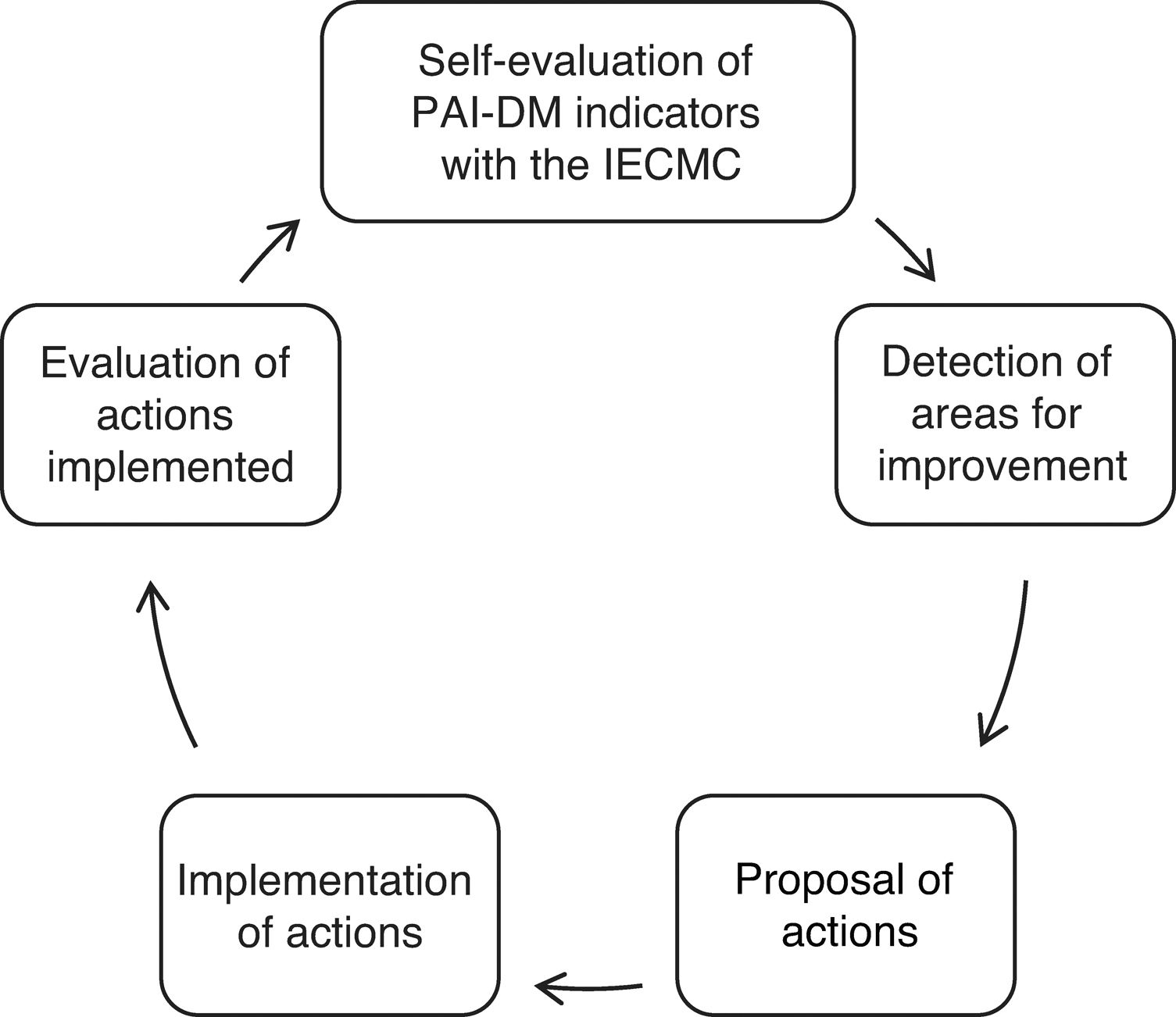
Study protocolA multidisciplinary team of healthcare professionals particularly involved in DM care was formed to implement the project. This consisted of 3 endocrinologists, 10 PC physicians, 2 endocrinology nurses, and 4 PC nurses as references of the HUPM and the corresponding PC health centers. In the first quarter of 2015, the baseline situation was analyzed based on the IECMC methodology to detect organizational weaknesses in the management of patients with DM. The previously selected PAI-DM2 indicators corresponding to 2014 were evaluated. In 2015 (start), 2016 and 2017 (after the intervention), results of the indicators were reviewed again and were compared to the initial data to ascertain any changes attributable to implementation of the strategy. During the initial process, actions to be carried out through regular meetings (2–3 annually) were defined. Improved continuity of care of patients with DM was established as the priority objective. After presentation of results of self-assessment, interventions were proposed both in PC and HC, aimed mainly at optimizing the functioning of the DM Day Hospital (DMDH), revitalizing the role of the reference professional, promoting use of tools for recording clinical and care history, supporting self-care through the development of structured and homogeneous educational material, improvements in care for patients with severe diabetic foot, and enhancing training activities. Response variables were analyzed by comparing their baseline values with those obtained 2 years after implementation of improvement activities. According to the recommendations of the Andalusian PAI-DM,8 patients with T2DM were seen and monitored in PC, and those with T1DM in HC. Data were taken from the digital history (Diraya and Diabaco), the Minimum Basic Data Set of Andalusia (CMBDA), and the PIDMA. Criteria for patient referral from PC to HC were those included as such in the PAI-DM. Fig. 1 shows a summary of the study protocol.
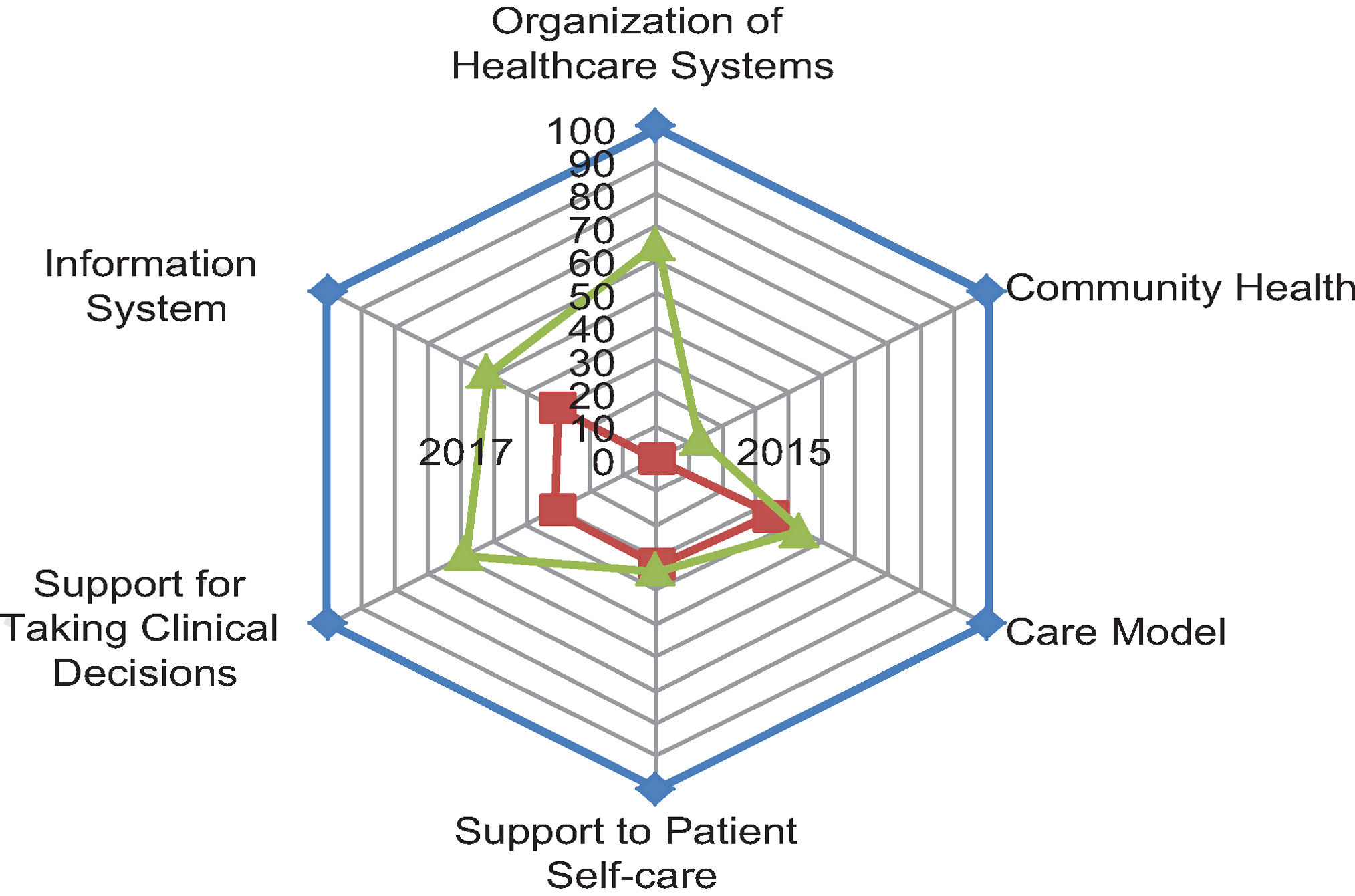
Instrument for evaluation of care model in chronic conditionsThe IECMC tool consists of 6 dimensions, 27 components, and 75 interventions to further improve care for chronic patients, a scale to measure progress, and a web environment for self-assessment of organizations. This exercise allows for identifying both strong areas and those amenable to improvement and guides the plans to be developed. Self-assessment score ranges from 0 and 7500 points.15,16
Data analysisResults were analyzed using SPSS statistical software, version 20.0 for Windows. The descriptive analysis of qualitative variables was based on calculation of frequencies and percentages, while quantitative variables were reported as the mean, the standard deviation (SD) for variables normally distributed, and the median and range for variables not normally distributed. After checking assumption of normality in the sample using a Kolmogorov-Smirnov test, the following tests were performed: to compare quantitative variables between independent groups, a Student’s t-test or a Mann-Whitney’s U test for non-parametric contrast; to compare quantitative variables between related groups (before-after analyses), a Student’s test for paired samples or a Wilcoxon test for non-parametric contrast; to compare qualitative variables between independent groups, a chi-squared test or a Fisher test if required. All significance values will refer to the two-tailed test. Values of P < .05 were considered statistically significant. In addition, to determine the strength of the linear relationship between 2 quantitative variables, the Pearson’s (or Spearman’s) correlation coefficient was determined for non-parametric variables. A multivariate analysis was performed building binary logistic regression models. The independent variables to be included in the models were selected based on clinical and statistical criteria (P < .05 in bivariate analysis), establishing the criterion for inclusion in the model as 0.10 and the exclusion criterion as 0.15 (PIN and POUT).
Ethical considerationsAs this was an intervention in organizational aspects of the care activity in the healthcare area and the population data was analyzed anonymously, patients enrolled were not requested their informed consent. The project was approved by the Research Ethics Committee of HUPM, Cadiz.
ResultsThe characteristics of the population (213,691 inhabitants) of the healthcare area under study and the different quality indicators analyzed are described below.
Process indicatorsAccording to the process indicators established by the SAS, the proportions of patients included in the digital clinical history (Diraya) with a diagnosis of DM in the general population over 18 years of age were similar (8.5% in 2015 and 8.3% in 2017).
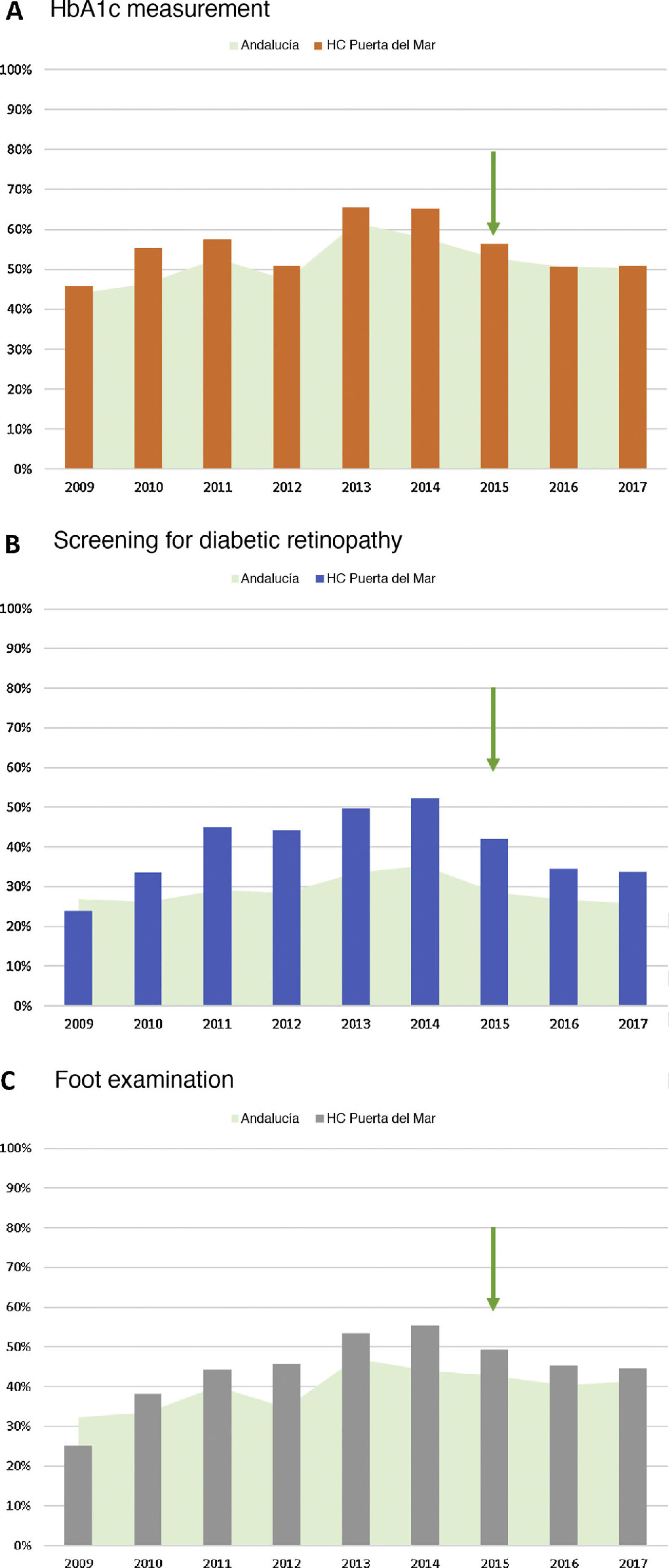
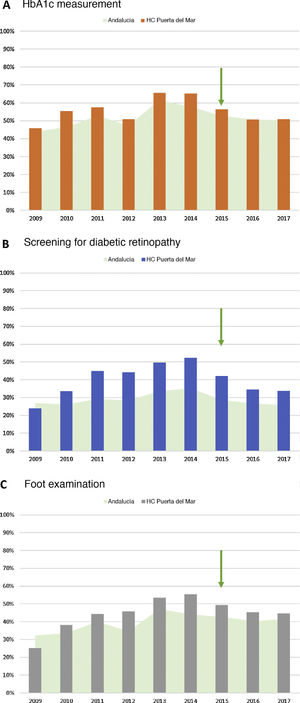
As regards laboratory studies, the proportion of patients with DM performed at least one HbA1c measurement recorded during 2015 was 56.4%, with a slight decrease in subsequent years (Fig. 2).
Proportion of patients performed process indicators in the study population (HUPM healthcare area) from 2009 to 2017: A) HbA1c measurement; B) performance of retinography in the screening program; and C) foot examination. Comparison with data taken throughout Andalusia (source: PIDMA). The arrow indicates the year the procedure started.
HC: hospital care; HbA1c: glycosylated hemoglobin; HUPM: Hospital Universitario Puerta del Mar de Cádiz; PIDMA: Comprehensive Plan for Diabetes Mellitus of Andalusia.
With regard to retinography for the screening of diabetic retinopathy, the proportion of patients with DM registered who had been performed at least one retinography in the past 2 years was 42.2% in 2015 and decreased to 33.8% in 2017 (Fig. 2). As to diabetic foot screening, the proportion of patients with DM undergoing at least one foot examination in the past year was 49.3% in 2015, and decreased to 44.6% at 2 years (Fig. 2).
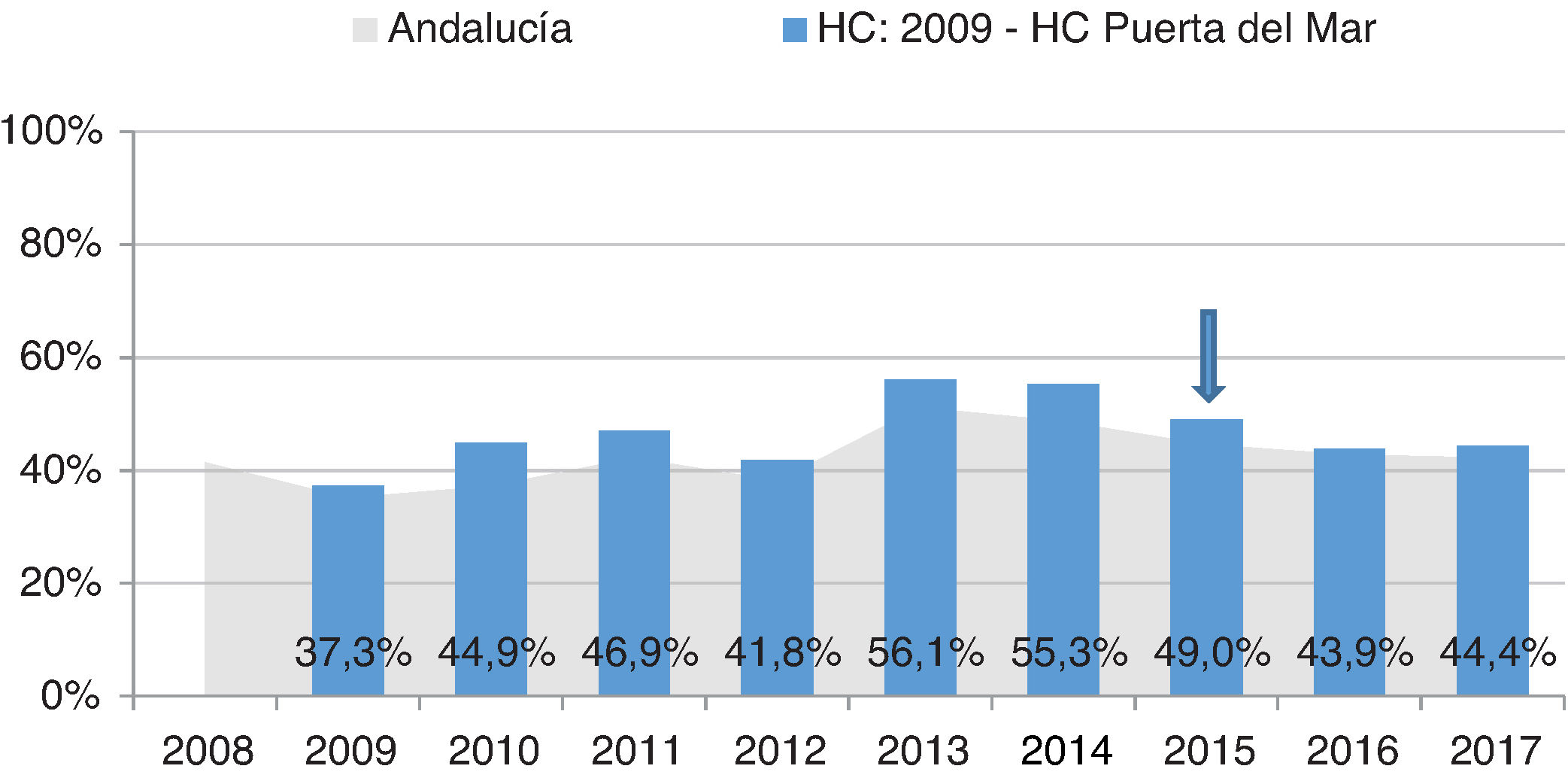
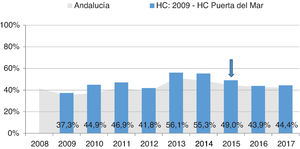
Intermediate resultsAs regards intermediate results, the proportion of patients with optimum metabolic control (HbA1c < 7%) decreased slightly from 34.7% in 2015 to 30.8% in 2017. The proportion of patients with acceptable metabolic control (HbA1c < 8%) also increased from 49% in 2015 to 44.4% in 2017 (Fig. 3). As to the results of the examinations to screen for complications, those from patients with normal retinography were 80.5% in 2015 and 83.5% in 2017. On the other hand, the proportion of patients with normal foot examinations was really low, only 20.1% in 2015 and 24% in 2017 (data not shown).
Proportion of patients with acceptable metabolic control (HbA1c < 8%) recorded in the HUPM healthcare area from 2009 to 2017. Comparison with data taken throughout Andalusia (source: PIDMA). The arrow indicates the year the procedure started.
HC: hospital care; HbA1c: glycosylated hemoglobin; HUPM: Hospital Universitario Puerta del Mar de Cádiz; PIDMA: Comprehensive Plan for Diabetes Mellitus in Andalusia.
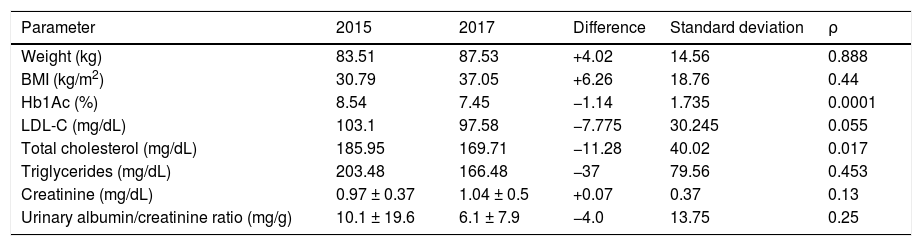
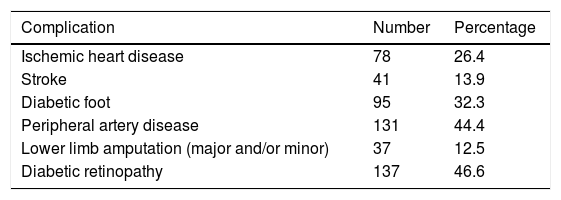
Of all 295 referrals made, the proportion of suitable referrals based on the previously agreed criteria markedly increased as compared to 2015 (40% vs. 76% respectively; P = .001; 95% CI: 26.4–39.02). The most common reason for referral was complicated diabetic foot [100 (34%) patients], followed by acute decompensation or poor DM control [41 (14%) patients]. Overall, mean age of patients referred to the DMDH was 63.0 ± 16.3 years, with a predominance of males and a high prevalence of risk factors for VD (Table 1) and chronic complications of DM (Table 2).
Characteristics of patients referred to the DMDH (n = 295). Clinical and laboratory variables and risk factors for vascular disease (year 2015 vs. 2017).
| Parameter | 2015 | 2017 | Difference | Standard deviation | ρ |
|---|---|---|---|---|---|
| Weight (kg) | 83.51 | 87.53 | +4.02 | 14.56 | 0.888 |
| BMI (kg/m2) | 30.79 | 37.05 | +6.26 | 18.76 | 0.44 |
| Hb1Ac (%) | 8.54 | 7.45 | −1.14 | 1.735 | 0.0001 |
| LDL-C (mg/dL) | 103.1 | 97.58 | −7.775 | 30.245 | 0.055 |
| Total cholesterol (mg/dL) | 185.95 | 169.71 | −11.28 | 40.02 | 0.017 |
| Triglycerides (mg/dL) | 203.48 | 166.48 | −37 | 79.56 | 0.453 |
| Creatinine (mg/dL) | 0.97 ± 0.37 | 1.04 ± 0.5 | +0.07 | 0.37 | 0.13 |
| Urinary albumin/creatinine ratio (mg/g) | 10.1 ± 19.6 | 6.1 ± 7.9 | −4.0 | 13.75 | 0.25 |
LDL-C: low density lipoprotein cholesterol; HbA1c: glycosylated hemoglobin; DMDH: diabetes mellitus day hospital; BMI: body mass index.
Microvascular and macrovascular complications of patients referred to the DMDH (n = 295).
| Complication | Number | Percentage |
|---|---|---|
| Ischemic heart disease | 78 | 26.4 |
| Stroke | 41 | 13.9 |
| Diabetic foot | 95 | 32.3 |
| Peripheral artery disease | 131 | 44.4 |
| Lower limb amputation (major and/or minor) | 37 | 12.5 |
| Diabetic retinopathy | 137 | 46.6 |
DMDH: diabetes mellitus day hospital.
The main characteristics of patients referred for diabetic foot include advanced age (69.1 ± 11.8 years). Most of them were males (61.6%) with an acceptable metabolic control (HbA1c 7.6 ± 1.4%) and a long disease duration (17.1 ± 10.2 years). Forty-nine percent of them were on insulin therapy and 34% on non-insulin therapy, and the remaining 17% received combined therapy. Most of them had complications, including retinopathy (54.5%), nephropathy (39%), polyneuropathy (77.1%), distal arterial disease (69.5%), and coronary artery disease (42.4%); 15% had prior amputations (10% minor and 5% major).
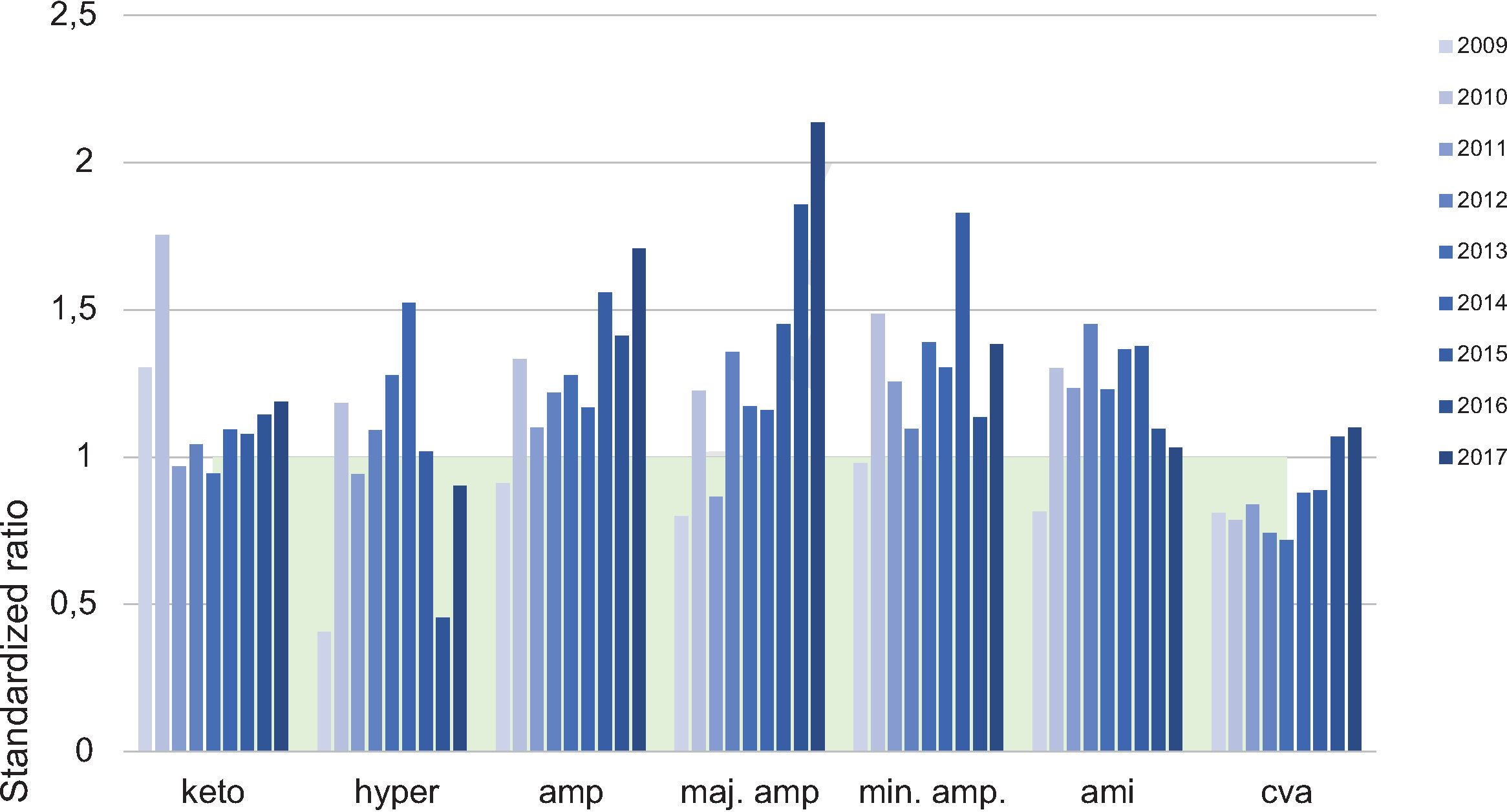
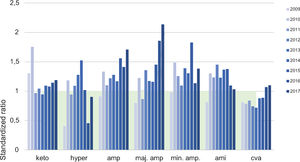
Final health outcomes indicatorsData obtained from the analysis of the CMBDA of patients admitted for complications of DM show no sustained trend in any of the complications assessed (ketoacidosis, hyperosmolar hyperglycemic decompensation, acute myocardial infarction, and stroke), except for persistent elevation of major amputations in the past 3 years. The standardized ratio to the Andalusian mean in 2015 was 0.88 (95% CI: 0.63–1.16) and 1 (95% CI: 0.87–1.14) in 2017 (Fig. 4).
Source: Hospital admissions for complications of DM in the period 2009–2017 at the HUPM. CMBDA. amp: amputations; maj. amp: major amputations; min. amp: minor amputations; cva: cerebrovascular accident; keto: diabetic ketoacidosis; CMBDA: Minimum basic data set in Andalusia; hyper: hyperosmolar hyperglycemic decompensation; HUPM: Hospital Universitario Puerta del Mar de Cádiz; AMI: acute myocardial infarction.
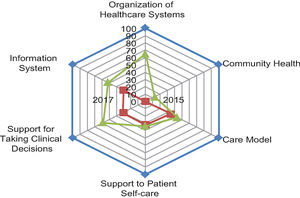
With regard to the results derived from the IECMC-DM analysis, the initial score was 1415 points in the first quarter of 2015 and 2270 points in December 2017 (P = .02) (Fig. 5). The marked improvement achieved with intervention in the organizational aspects of SAS and the low impact seen on patient self-care, healthcare model, and community health should be stressed.
DiscussionThe results of a quality of care before-after study intended to assess an intervention model for chronic patients adapted to patients with DM (IECMC-DM) are reported. Favorable results were seen 2 years after implementation of the model, particularly in all aspects related to information systems, support to clinical decision-making, and to the public health system itself.
In the specific care aspects, there has been a marked increase, from 40% in 2015 to 76% in 2017, in the proportion of adequate referrals from PC to HC according to the criteria previously agreed by the working group. This improvement is due, at least in part, to the actions taken to disseminate the activity and referral pathways to the DMDH, including development of informative material, data entry into the corporate intranet, training sessions, and preparation of a “referral sheet” to be completed by the referring physician. The most common reasons for referral were acute and chronic complications of DM, and the most common among these was severe diabetic foot. It should be noted that, in this case, and despite the improvement measures taken, no reduction was achieved in lower limb amputations, that remained high as compared to the average in Andalusia. With regard to the process and health outcomes indicators, most values have remained stable in recent years, and no significant changes from the previous years have been noted in the proportion of patients included in the digital history, HbA1c measurement, screening for chronic complications, and admissions for acute or chronic complications, except for major amputations. This impairment is difficult to explain, but should not be attributed to intervention. Other factors such as changes in social and economic determinants (such as the recent crisis) or incorporation of new drugs in recent years may have been relevant, but this could not be analyzed. Like other authors, we found that the debate generated by the methodology of the intervention with IECMC-DM allowed for detecting areas for improvement and facilitating communication between the different levels, particularly direct communication with the DMDH.17
Quality of care, mainly focused on coordination of PC and HC, is crucial for improving health outcomes and other quality indicators, and this can be achieved using specific plans and strategies that, although effective, have not yet been sufficiently tested.12,13,18 However, many other factors such as family, economy, marital status, sex, and level of healthcare services play a determinant role.19–21 This would justify that there has been little change in aspects such as the patient's level of self-care, the structure of the care model, and the level of community health, which have a significant complexity and are influenced by multiple factors. Thus, although the intervention was performed in a healthcare area following the indications of PAI-DM and a marked improvement was achieved in the organizational aspects of the healthcare system, no significant changes were seen in other aspects evaluated (particularly health outcomes), probably due to the complexity of the intervention and the difficulties inherent to the analysis of the results.
As significant limitations of the study, it should be noted that analysis of final health outcomes requires a longer follow-up time and that efficiency values are not yet available; in addition, the interventions performed were not individually considered to be able to identify and promote those that were most effective. On the other hand, information on treatment changes or a detailed characterization of the type of DM would have been important, but were not considered indispensable to assess the impact of the action, and only the current indicators in the PAI-DM were used.
To sum up, implementation of a specific management model for the care of patients with DM (IECMC-DM) in a hospital healthcare area improves the degree of information of professionals on the activities they have to perform, communication between PC and HC, patient referral criteria, and the public health model. Evaluation of the final health outcomes in the longer term would be needed, as well as performance of an efficiency study and external validation to justify implementation of this model in other healthcare areas, because there is a wide room for improvement in coordinated PC-HC care for patients with DM.
FundingMSD Spain collaborated in this study by providing help and support to the working group for its activities.
Part of this study was funded by the project ITI0029-2017 (FEDER and Health Department of the Regional Government of Andalusia). Instituto de Investigación Biomédica e Innovación de Cádiz (INIBICA).
AuthorshipIMG and MAD designed the study, analyzed and interpreted the data, prepared the first draft of the manuscript, carried out a critical review of the contents, and approved the final version of the article. SCG, LL and EMS collected and updated some of the data obtained; MJF and AZ actively supported the execution of the work.
All authors made critical contributions to the content and approved the final version of the study.
Conflicts of interestThe authors of this article have no conflicts of interest in relation to the objective or the results of this article.
Hospital Puerta del Mar: José Ortego Rojo, Francisco J. Vilchez López, Mar Roca Rodríguez, Marta Iturregui Guevara, Alicia Abal Cruz, Ana Montero Galván.
C.S. La Laguna: Julián Correa de la Calle and Pilar Vicioso Ruiz.
C.S. Rodriguez Arias: Juan Manuel Martínez Muñoz and Ana Amor Cruceira.
C.S. La Paz: Eusebio Rocha Vega.
C.S. La Merced: M. José Serrano Muñoz and Teresa Almagro Villar.
C.S. El Mentidero: Pilar Cordón Pulito.
C.S. Loreto: Inmaculada Casas Ciria and Joaquín Quijano Sánchez.
C.S. Joaquín Pece: Luisa M. Gómez Dominguez.
C.S. Puerta Tierra: Margarita Trinidad Ballester Díaz.
Please cite this article as: Mateo-Gavira I, Carrasco-García S, Larran L, Fierro MJ, Zarallo A, Mayoral Sánchez E, et al. Modelo específico de coordinación entre atención primaria y hospitalaria para la atención a pacientes con diabetes mellitus. Evaluación de resultados a dos años (2015–2017). Endocrinol Diabetes Nutr. 2021;68:175–183.