Choristoma or heteropia is a congenital anomaly consisting of a heterotopic remnant of cells or microscopically normal tissues, i.e., a growth of normal tissue in an abnormal location. This heterotopic remnants can contain different types of cells or tissues in different tissues or organs of the body. Heterotopic remnants are usually of little importance, but can be confused clinically with neoplasms.
Pituitary choristoma is rare. Heterotopic remnants in the pituitary gland have been reported in both anterior and posterior pituitary.1 Foci of ganglionic cells have been found in the neurohypophysis.2 On the other hand, focal squamous epithelia in the anterior pituitary is a common finding but it is rather metaplastic from parenchymal cells than ectopic tissue.3 Lastly, small foci of ectopic salivary gland tissue have been demonstrated in the posterior lobe of pituitary glands.4
Intrasellar symptomatic salivary gland is very rare although it could be considered in the differential diagnosis of intrasellar masses.5 We report a new case of symptomatic pituitary salivary gland choristoma and discuss the most relevant aspects of this pathology in relation to the prevalence, clinical diagnosis and therapeutic outcomes.
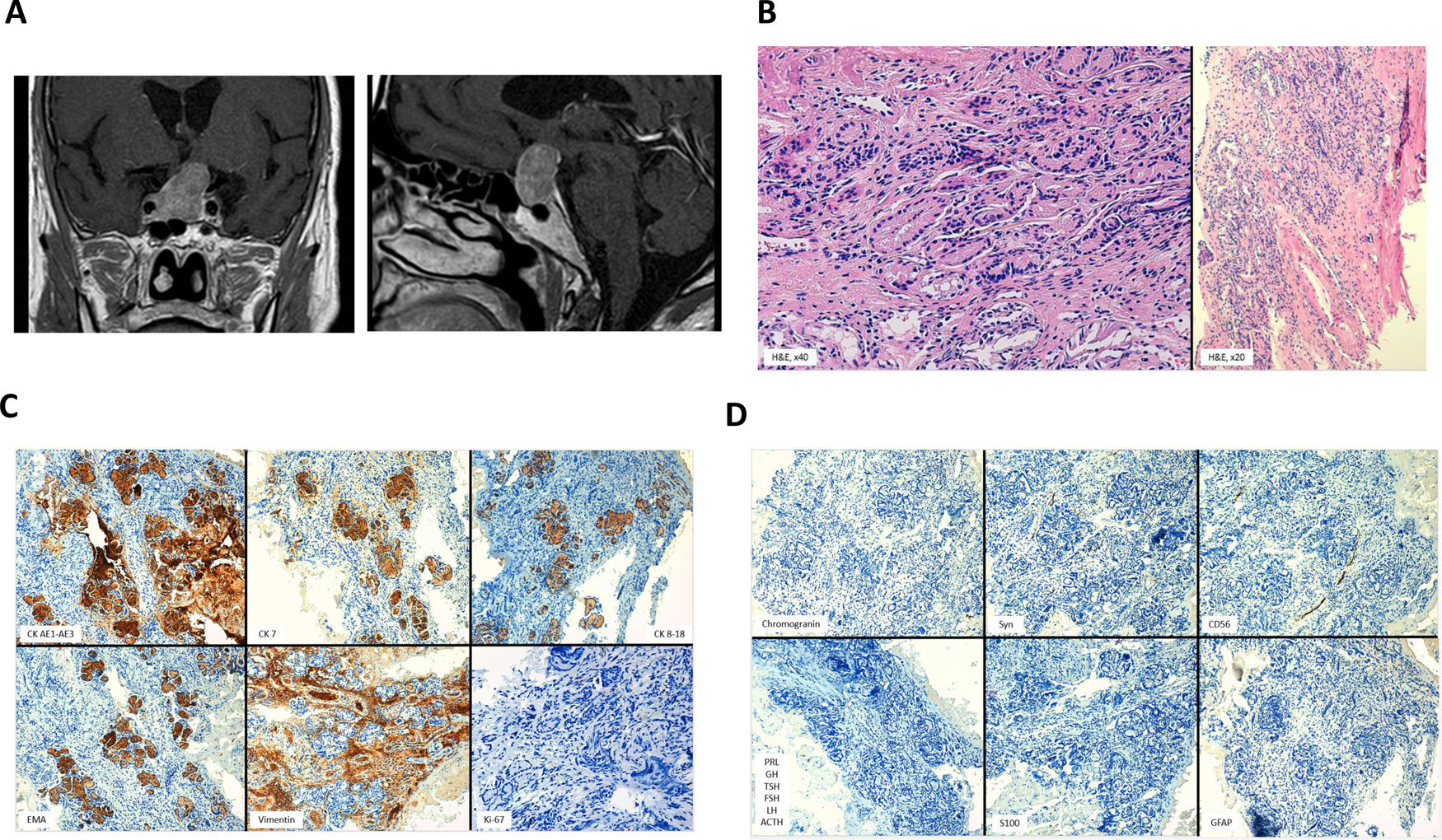
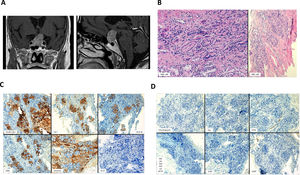
A 71-year-old man underwent surgery for a sellar–suprasellar lesion after consulting for severe headache for 7 days and binocular diplopia of several hours of evolution. Visual campimetry was consistent with chronic bilateral glaucoma and less likely with incongruous right homonymous hemianopia. Bitemporal hemianopia was ruled out. The fundus was normal. Preoperative hormonal evaluation showed the presence of hypopituitarism (gonadotropins, GH, TSH and ACTH deficiency). PRL was normal (5.8ng/ml). Pituitary MRI showed a large expansive mass (26mm×28mm×17mm) in sellar region suggestive of macroadenoma with extension mainly to the right cavernous sinus and to the left suprasellar region with significant compression of the optic tract and hypothalamic structures (Fig. 1A and B). The postoperative period was favorable with an improvement in headache and previous diplopia. No cerebrospinal fluid fistula or diabetes insipidus was developed. The patient was discharged on replacement hormonal treatment with hydrocortisone, levothyroxine and testosterone. The histopathological study was compatible with sellar choristoma of salivary gland (Fig. 1B-D).
(A) Preoperative MRI showing a large expansive mass in the sellar region suggestive of macroadenoma with extension mainly to the right cavernous sinus and to the left suprasellar region with significant compression of the optic tract and hypothalamic structures on coronal (left) and sagittal (right) contrast-enhanced T1-weighted images. Pathological study: (B) Acinar-patterned seromucosal glands (left: H&E, 40×) embedded in a dense fibrovascular stroma (right: H&E, 20×). (C) The epithelium of the glands showed intense immunoreactivity for cytokeratin AE1–AE3, cytokeratin 7, cytokeratin 8–18 and epithelial membrane antigen (EMA) and was negative for vimentin (immunohistochemistry, 20×). The proliferative index Ki67 was less than 1% (immunohistochemistry, 40×). (D) Immunoexpression of neuroendocrine markers (chromogranin, synaptophysin and CD56) (immunohistochemistry, 20×) and of pituitary hormones (immunohistochemistry, 20×) was not observed. The stroma was negative for S100 and glial fibrillary acidic protein (GFAP) (immunohistochemistry, 20×).
Salivary gland ectopy has been documented in multiple organs and body tissues. The intraselar location of the salivary glands generally occurs asymptomatic, having been reported in up to 3.4% in autopsy studies.4 In exceptional cases, these ectopic embryonic remnants can present symptomatically. To date, fewer than 15 cases have been described.5
Two possible explanations have been considered to explain the development of salivary gland tissue in the pituitary.5 On the one hand, during embryogenesis, the salivary gland developed from the primitive epithelium of the oral cavity would be transferred to the sellar region within the wall of Rathke's pouch, which migrates from the primitive oral cavity toward the base of the brain and fuses with an extension of the third ventricle to form the pituitary gland. Another possible explanation would be the transformation of the primitive epithelium of the hypophysis into salivary gland tissue during human embryogenesis.
The clinical course of pituitary salivary ectopia is generally benign, although these remnants may show progressive growth due to active mucous secretion within the ectopic glands. In addition, there is the possibility of a neoplastic transformation leading to a salivary gland-like tumor.6 In our clinical case, both the neoplastic transformation and the progressive accumulation of mucous secretion could explain the clinical presentation.
Most of the reported clinical cases of symptomatic salivary glandular tissue in the pituitary gland correspond to embryonic remnants of salivary tissue, some of them originated in the thickness of a Rathke cleft cyst; however, salivary gland adenomas and carcinomas have also been described, the latter associated with metastasis. Symptomatic pituitary salivary ectopia is more common in women (female–male ratio: 2.3) with a peak incidence in the second and third decade of life (mean age 28 years). The most common form of clinical presentation is headache (65%), followed by visual field alterations (bitemporal hemianopia) (35%) and symptoms of hormonal deficiency (hypogonadism) (20%). The most frequently hormonal alteration is hyperprolactinemia (30%) and the typical image on pituitary MRI is that of a pituitary macroadenoma with suprasellar extension. In the clinical course, diabetes insipidus is present in about 30% of patients.5–18 The treatment used is transsphenoidal surgery with no associated mortality to date. The imaging study is not enough to establish the diagnosis since it is indistinguishable from pituitary adenoma. The diagnosis of salivary gland ectopy can only be made with the histopathological study after transsphenoidal surgery, which seems to be an adequate therapy in most of the cases reported to date.
Informed consentInformed consent was obtained from the patient for the publication of this article.
FundingNo funding.
Conflict of interestNone declared.