Pheochromocytoma is an uncommon neuroendocrine tumor derived from adrenal chromaffin cells. Pheochromocytoma causes signs and symptoms resulting from catecholamine excess, and its diagnosis may represent a challenge conditioned by the sensitivity and specificity of the diagnostic tests.1
We report the case of a 41-year-old woman who reported episodes of palpitations lasting a few minutes, associated with increased blood pressure and occurring in relation to menstruation for the previous two years. There was no associated headache. The patient reported smoking, prior uneventful menses, and two normal term pregnancies. Cardiological study (electrocardiogram, Holter electrocardiogram and blood pressure, and echocardiogram) and chest X-rays were normal, even during symptomatic periods. Physical examination revealed no significant findings. The patient had a weight of 60kg, a height of 169cm, blood pressure of 130/60mmHg, and a heart rate of 80bpm. Ultrasound gynecological examination was normal.
As part of a differential diagnosis of palpitations and high blood pressure, complete laboratory tests were requested including protein, hormones, and tumor markers. Test results included: blood glucose 89mg/dL, normal liver profile, beta-2-microglobulin 1.4mg/L, proteins and immunoglobulins in the normal range, tryptase 7.07ng/mL (<11.5), TSH 1.45μU/mL, calcium 9.8mg/dL, calcitonin 2mg/dL (2–11.5), renin 8pg/mL (3–33), aldosterone 137pg/mL (97–626), chromogranin A 0.8nmol/L (<6). Urinary fractionated metanephrines were normal in two separate measurements. Due to symptom persistence several months later, even during the intermenstrual period, a repeat test was performed, showing a slight increase: normetanephrine/creatinine ratio 167μg/g (<560), metanephrine/creatinine ratio 333,3μg/dL (<260), and vanillylmandelic acid/creatinine ratio 3.74μg/g (<10), with a chromogranin A level of 12nmol/L.
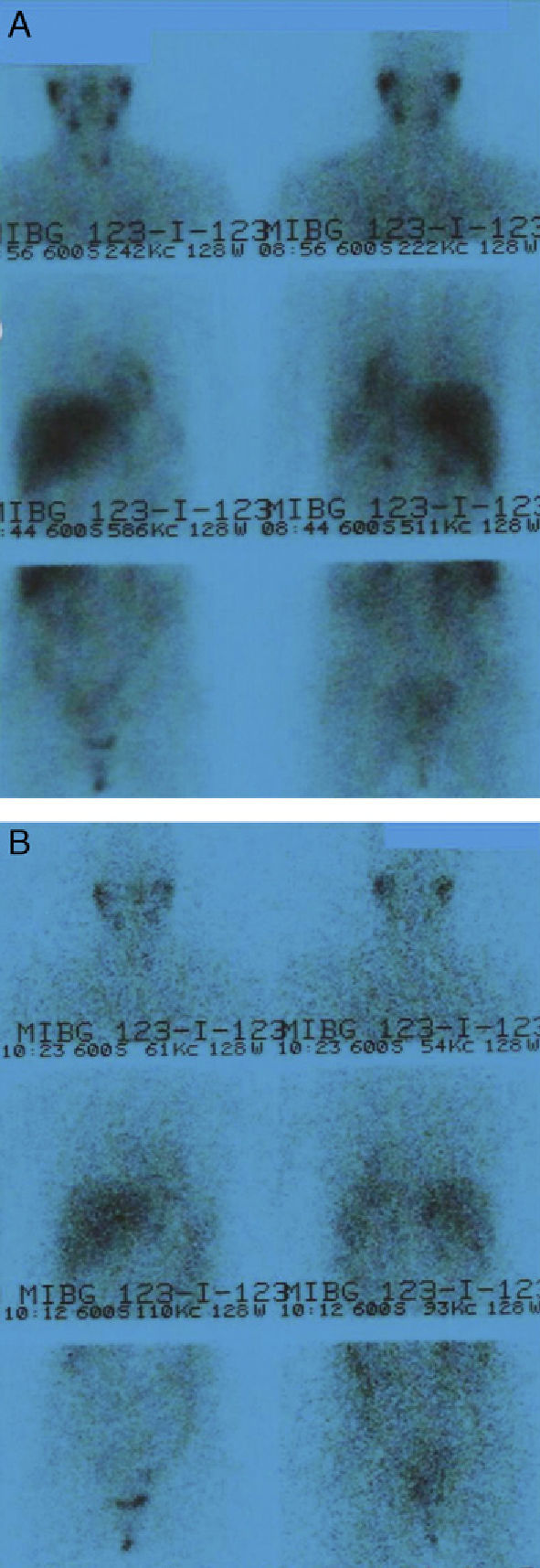
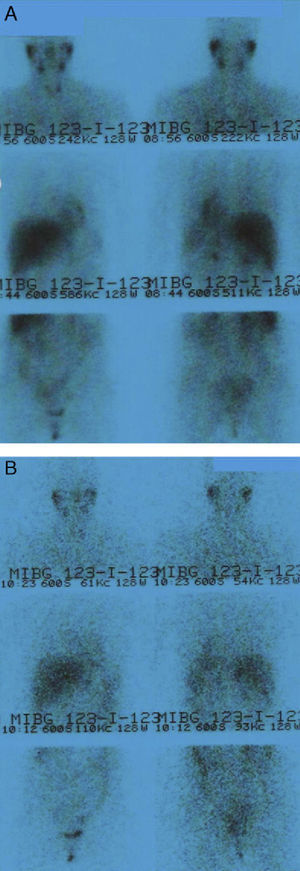
A pheochromocytoma or paraganglioma of potential gynecological location was suspected, and an abdominal computed tomography scan (CT) was requested, which showed normal results. A subsequent 123I-metaiodobenzylguanidine (123I-MIBG) scintigraphy showed no pathological uptake (Fig. 1). An additional CT scan of the neck, mediastinum, and chest showed a thyroid nodule, which was found to be benign in nature after ultrasound-guided fine needle aspiration.
123I-MIBG scintigraphy (dose of 185MBq). Anterior and posterior views of neck–chest–abdomen at 24h (A) and anterior and posterior views of neck–chest–abdomen at 48h (B). No pathological findings are seen. Images show a distribution of the radiopharmaceutical consistent with physiological distribution from the initial acquisitions.
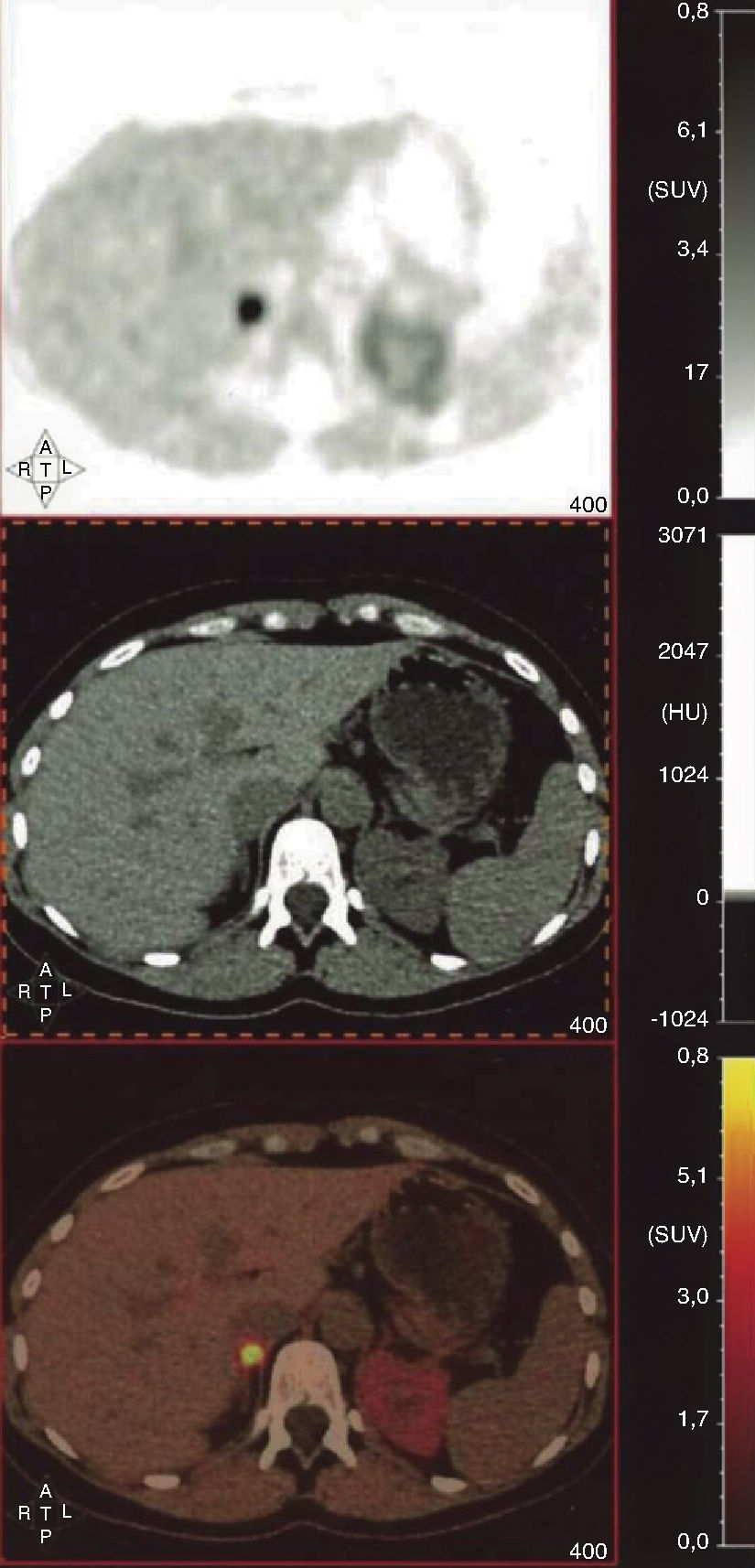
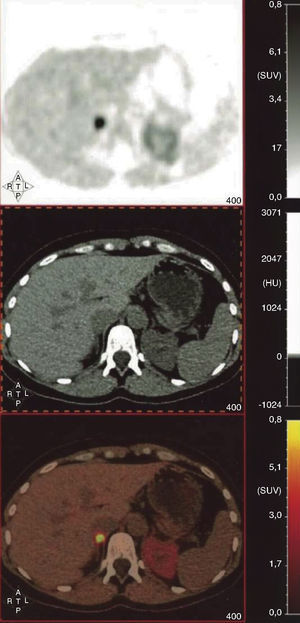
Despite the inconclusive biochemical results and the repeated negative test results, the clinical signs of the patient prompted us to request 18F-dihydroxyphenylalanine positron emission tomography (18F-DOPA-PET-CT), which showed increased uptake in the right adrenal gland (SUVmax 9.59) (Fig. 2) consistent with pheochromocytoma. Alpha-adrenergic blockade was started, with good blood pressure control, followed by beta-blockade before surgery. The pathological laboratory confirmed the suspicion and reported no findings suggesting histological aggressiveness (Ki67 <2% and immunohistochemistry positive for ENE, S-100, chromogranin A, synaptophysin, CD56, PGP 9.5, and vimentin). A genetic study has been requested.
18F-dihydroxyphenylalanine positron emission tomography (18F-DOPA-PET-CT). Axial sections at abdominal level (SPECT, CT, and fusion). A markedly increased uptake by the right adrenal gland (SUVmax=9.59) is seen in the absence of structural gland enlargement in the CT scan, which is consistent with pheochromocytoma. Activity of the left adrenal gland is normal. No focal deposits suggesting paraganglioma and/or metastases are seen in the neck, chest, abdomen, or pelvis.
The diagnosis of pheochromocytoma is based upon clinical and biochemical data and localization studies. Symptoms are non-specific and show great inter-individual variability. They may mimic many other more common conditions, so that although the presence of pheochromocytoma may sometimes be suspected, the condition is not always diagnosed.2
The test of choice for screening a catecholamine-secreting tumor is the measurement of free plasma or urinary fractionated metanephrines.3 Ideally, both tests should be performed, but urinary measurement is sometimes the only measurement available.4 Equivocal results may sometimes be achieved, as initially occurred in our patient, raising doubts as to whether the diagnostic algorithm should be continued or whether this should be considered as a false positive.2
If the clinical signs and biochemical data are consistent, a localization study is indicated, starting at abdominal levels.4 Anatomical CT scans or magnetic resonance imaging (MRI) (90–100% sensitivity, but low specificity) usually have to be supplemented with functional nuclear medicine tests, including scintigraphy with 123I-MIBG (99% specificity)5 and the somatostatin analog 111In-pentetreotide, which is less commonly used because of its lower yield.6
However, these procedures do not always allow for the identification of tumor location because of their limited spatial resolution. In such cases, PET imaging may be more useful.7 Different radiotracers have been used for this purpose, including 18F-dopamine (18F-FDA), 18F-DOPA, and 18F-deoxyglucose (18FDG), based respectively on the ability of these tumors to incorporate and subsequently decarboxylate amino acids and on cell incorporation of glucose through the GLUT-1 pathway. Other recently designed radiotracers based on the presence of somatostatin receptors (68Ga-DOTA-Tyr3-octreotide [68Ga-DOTATOC] and DOTA-Nal-octreotide [68Ga-DOTANOC]) have given encouraging results, but adequate comparative studies are not available yet.6
Several authors have concluded that 18F-DOPA-PET has a higher yield and, if implemented as a routine procedure, would condition patient management and treatment.7 Some series report false positive rates of 0% and sensitivity values up to 100%, higher than those of other functional tests, even if metanephrine levels are not very high,5,6,8 as occurred in our patient. An additional advantage over 123I-MIBG is that, since 18F-DOPA has a shorter half-life, it allows for a higher dose and earlier image acquisition.9 In addition, differentiation from normal adjacent tissue is enhanced, because healthy adrenal medulla does not take up the radiotracer,6,9 a feature that some authors have proposed optimizing by prior treatment with carbidopa.10
It should be noted, however, that the best diagnostic test in each case is difficult to establish because of the heterogeneity and low prevalence of pheochromocytoma and paraganglioma, and will depend on the individual patient characteristics in terms of the secretory profile, suspected location, the histological characteristics of cell differentiation, biological behavior, and potential association with a genetic mutation.6,11
An adaptation to advances in imaging procedures is required, which includes the possibility that in hospitals where 18F-DOPA-PET is available, it may replace 123I-MIBG, at least partly, because of its greater precision, convenient performance, and less adverse effects for patients, although cost-effectiveness studies assessing its use will be required.
Please cite this article as: Ramós-Leví AM, et al. Tomografía por emisión de positrones marcada con 18-Fluor-dihidroxifenilalanina para el diagnóstico de feocromocitoma. Endocrinol Nutr. 2013;60:336–8.