One out of every three Spanish children or adolescents has excess weight, which represents a significant and increasing public health problem in Spain. A recent cross-sectional Spanish study on a representative sample of 6139 subjects aged 2–15 years reported prevalence rates of obesity and overweight of 10.3% and 18.8% respectively.1 Obesity was most prevalent from 4 to 5 years of age (18.3%), and overweight from 8 to 9 years (25.5%). Overweight was more common in males, while obesity occurred more frequently in males and girls aged 4–7 years. Higher obesity and, especially, overweight rates were seen in male adolescents aged 12–15 years, possibly because of the influence of fashion and social stereotypes on female body image. There is a North-South-Southwest gradient in prevalence of infantile obesity which agrees with the pattern seen in other Spanish and European studies. Both obesity and overweight had an inverse linear association with socioeconomic status.
Spain has one of the greatest prevalence rates of child obesity in Europe, and is one of the three leading countries with highest rates from 5 to 15 years of age. Despite the increase in child obesity in Spain, parental perception of excess weight suggests that social acceptance of obesity in childhood is increasing.
One of the main problems in the study of obesity in children and adolescents is how it should be defined. Use of body mass index (BMI) is recommended. This is difficult because there is no standardized definition of child obesity, and reference curves and tables which are valid and useful in each environment should therefore be used. A second problem is selection of the cut-off points defining the normal weight, overweight, and obesity categories in this population.2
Several Spanish and international organizations and initiatives have developed reference curves and tables that faithfully represent the population for which they are prepared. All of them have advantages and disadvantages.
The BMI references most widely used in Spain are those included in the 2004 growth curves and tables (longitudinal and cross-sectional studies) of the Faustino Orbegozo Foundation, those derived from the 2008 Spanish cross-sectional growth study, and those provided in the 1988 growth curves and tables (semilongitudinal study) of the Faustino Orbegozo Foundation.
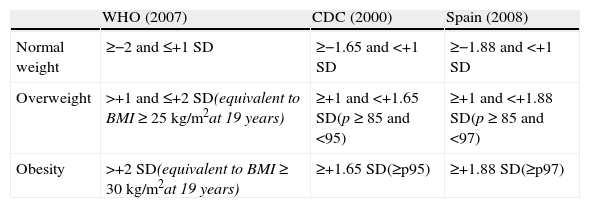
The most recent prospective Spanish study was conducted on 137 children and adolescents aged 8–16 years.3 Participants in this study were classified as normal weight, obese, or overweight subjects based on the 2007 WHO criteria, the 2000 criteria of the US Centers for Disease Prevention and Control (CDC), and the criteria of the 2008 Spanish cross-sectional study (Table 1). The relationship between cardiometabolic comorbidities and BMI cut-off points for age was also compared using these three standards. Forty-eight percent of participants were considered obese based on WHO criteria, while 43% were rated as obese based on CDC criteria and 16% based on national references. To summarize, results suggest that the BMI references and cut-off points of the WHO and CDC may be more helpful for identifying subjects with biochemical and vascular comorbidities and a potentially higher risk of future untoward events.
Classification criteria by BMI Z-score for age and sex.
| WHO (2007) | CDC (2000) | Spain (2008) | |
| Normal weight | ≥−2 and ≤+1 SD | ≥−1.65 and <+1 SD | ≥−1.88 and <+1 SD |
| Overweight | >+1 and ≤+2 SD(equivalent to BMI≥25kg/m2at 19 years) | ≥+1 and <+1.65 SD(p≥85 and <95) | ≥+1 and <+1.88 SD(p≥85 and <97) |
| Obesity | >+2 SD(equivalent to BMI≥30kg/m2at 19 years) | ≥+1.65 SD(≥p95) | ≥+1.88 SD(≥p97) |
CDC, US Centers for Disease Prevention and Control; SD, standard deviation; BMI, body mass index; WHO, World Health Organization; P, percentile.
Pathological body fat accumulation in childhood and adolescence has mid- and long-term consequences. It is associated to higher rates of hypertension, type 2 diabetes mellitus, dyslipidemia, liver steatosis, metabolic syndrome, and early atherosclerosis, amongst others. Presence of these risk factors does not necessarily imply morbidity in young age, but predicts for an increased risk of developing cardiovascular disease in subsequent stages of life. These risk factors are rather stable in adolescents and tend to persist in adult age even if BMI improves. Children with excess weight who were obese as adults had a higher risk of type 2 diabetes mellitus, hypertension, dyslipidemia, and carotid atherosclerosis. Luckily, risks of these conditions in children with excess weight who normalize their BMIs in adult age are similar to those of people who were never obese.4
Development of atherosclerosis starts in childhood and accelerates in the presence of obesity.5 Although clinical complications of atherosclerosis, such as myocardial infarction and stroke, usually occur in middle-aged or elderly subjects, the atherogenic process has been show to star in childhood. Extent and severity of atherosclerosis correlate to BMI and lipid profile in children and adolescents.
Adolescents with excess weight and those with a decreased physical fitness have greater risk of developing feeding behavior disorders.6 Excess body fat has been associated to increased risk of developing anorexia nervosa, bulimia, purgative behavior, and binge eating disorder in children and adults. High fitness levels may positively influence mood and self-esteem in young people.
Adequate intervention during the early plastic stages of development may improve health during the course of life. There are three critical periods for development of obesity: the fetal stage, the childhood growth period, and the pubertal or growth stage in adolescence.
Excess weight gain during pregnancy and maternal smoking are well-studied prenatal risk factors for obesity in childhood. The best-documented postnatal risk factors include shorter duration of breast-feeding and sleep during childhood. Pre-school children whose mothers did not smoke or gain excess weight during pregnancy, were breastfed for at least one year, and slept at least 12h daily had a 6% prevalence of obesity, as compared to a 29% prevalence in children with all risk factors. Prevalence rates were similar (4% and 28%, respectively) when they were 7–10 years old.7
Prenatal and postnatal periods are suitable to start behavioral changes that allow for reducing incidence of obesity and its complications because: (1) mothers are especially predisposed to modify their behavior to benefit their children; (2) frequent medical visits are required, and interventions related to health care have great potential; and (3) they are relatively short periods, and behavioral interventions are more successful in the short term. If these effective interventions start during pregnancy and are maintained after birth, they may decrease the risk of maternal obesity in future pregnancies.
Prevention of obesity in children and adolescents is therefore important to decrease the risks of metabolic consequences during childhood and adult age. Although no ideal prevention program has been developed, a multidisciplinary approach combined with school, healthcare, and community interventions and family involvement may possibly provide the best results.
Few children are born obese. Obesity rather develops over time, as children progress from childhood to adolescence. It is obvious that without an adequate, feasible, and sustainable multisectorial intervention, prevention of the current obesity epidemic in children and adolescents predicts for a future of early onset clinical cardiovascular disease. Effective programs for prevention of excess weight in childhood and adolescence need to be developed.
Please cite this article as: Calañas-Continente A. Un liderazgo poco favorecedor. Endocrinol Nutr. 2014;61:395–397.