Neuroendocrine tumors (NETs) of the appendix account for approximately 25–30% of all NETs in the gastrointestinal tract and for 35–95% of appendicular tumors.1,2 They are usually diagnosed incidentally after an appendectomy. Goblet cell carcinoid (GCC) tumor is an extremely rare appendicular NET showing a more aggressive biological behavior than all the other appendicular NETs.3
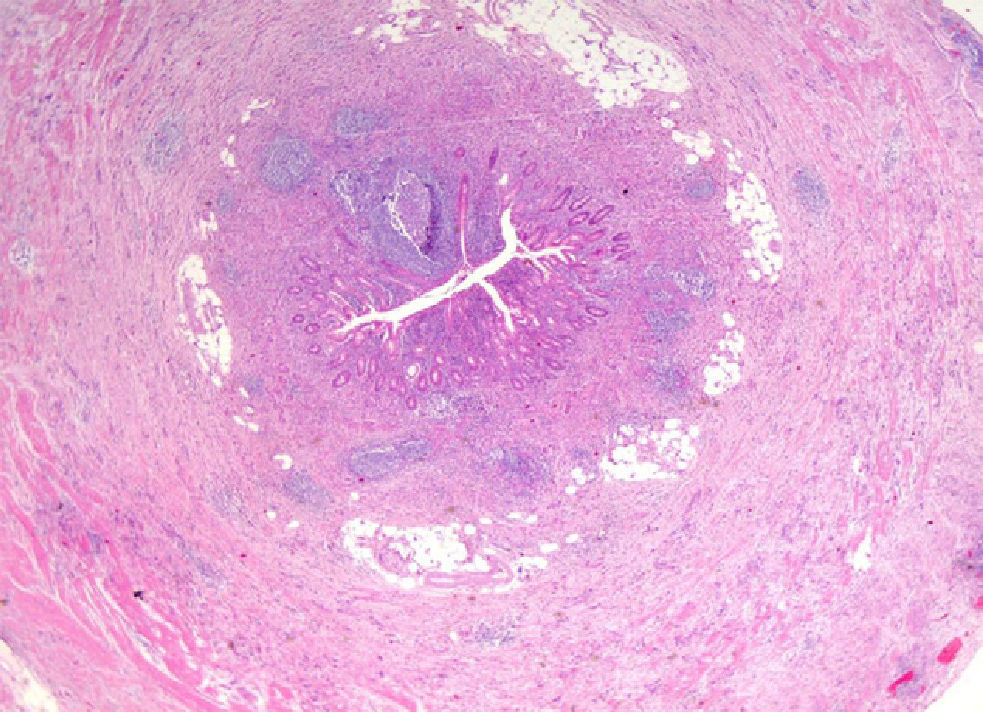
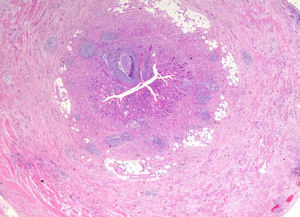
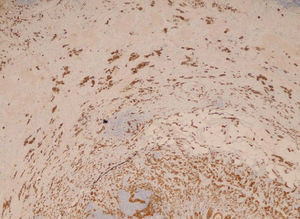
We report the case of a 55-year-old male patient with a history of type 2 diabetes mellitus treated with pioglitazone (30mg/day) who attended the emergency room reporting abdominal pain in the right iliac fossa and who underwent urgent appendectomy based on the clinical suspicion of acute appendicitis. The postoperative course was uneventful, but a pathological study of the surgical specimen showed changes consistent with ulcerative-phlegmonous appendicitis and a GCC or adenocarcinoid tumor 2.2cm at its largest diameter in contact with the surgical resection margin, infiltrating up to the serosa and with a Ki-67 of 40% (Figs. 1 and 2). Based on this pathological finding, a right hemicolectomy was performed four weeks after the appendectomy, with no residual tumor being found in the resected specimen. Postoperative monitoring using imaging tests and tumor markers (CEA, CA-19-9, and CA-125) showed no persistence or recurrence of the primary tumor or metastatic disease 30 months after confirmation of the diagnosis.
The GCC tumor, also called adenocarcinoid or mucinous adenocarcinoid, is a neuroendocrine carcinoma occurring virtually only in the ileocecal appendix which, because of its greater biological aggressiveness, requires a diagnostic and therapeutic approach different from all other appendicular NETs.4 It is an extremely rare tumor with an estimated incidence of approximately 0.05 cases/100,000 population/year and usually represents an incidental finding in 0.3–0.9% of all appendectomies. The mean age at presentation is during the fifth decade of life. This differentiates this tumor from all other NETs, which are usually diagnosed at between 15 and 25 years of age. GCCs are more common among the Caucasian population, and are equally distributed in both sexes.3
The initial presentation in most cases is acute appendicitis caused by tumor obstruction of the appendicular lumen, which is not associated with a hormone hyperfunction syndrome. Other less common clinical signs include those caused by the presence of a pelvic mass, such as abdominal pain, usually intermittent and low, bowel invagination or bleeding, abdominal distention, or secondary genitourinary complications.3,5 More rarely, the tumor is an incidental finding during surgical procedures for unrelated pathological conditions.6 Metastatic disease is found at diagnosis in approximately 11% of cases and is usually located in the ovaries, and less commonly consists of disseminated or extra-abdominal peritoneal carcinomatosis.5,6 A higher incidence of a second synchronous or metachronous neoplasm, preferably located in the colon, has also been reported as being associated with this tumor.4–7 GCC does not cause carcinoid syndrome, and urinary 5-hydroxyindoleacetic acid levels are usually normal.4
GCC has an aggressiveness intermediate between that of classical adenocarcinomas and typical appendicular carcinoid tumors, as 5-year survival rates ranging from 58% to 83% have been reported.7,8 Because of this, its therapeutic management and clinical monitoring more closely resemble those of the former group. Thus, after the appendectomy usually leading to its diagnosis, a right hemicolectomy is recommended within three months, although some authors only advise an appendectomy for tumors with no risk factors of locoregional or metastatic dissemination (a size of less than 1cm with no serosa or cecal mesoappendix invasion and low cell proliferation index). In women, regardless of age, this surgical procedure should be completed with bilateral salpingo-oophorectomy.3 In cases with widely disseminated disease, standard chemotherapy regimens for colorectal cancer based on the administration of 5-fluorouracil are usually administered.
After surgical resection, clinical, biochemical and imaging monitoring should be performed, initially every three to six months and at least annually thereafter.
To sum up, GCC is a rare appendicular neoplasm with greater biological aggressiveness than conventional carcinoid tumors. Its therapeutic management and subsequent clinical monitoring are therefore more similar to those of colorectal adenocarcinoma.
Please cite this article as: Fernández Catalina P, Lorenzo Solar M, Sánchez Sobrino P, Álvarez Álvarez C. Tumor carcinoide apendicular de células globoides. Endocrinol Nutr. 2013;60:e5–e6.