Pneumopericardium and pneumomediastinum are uncommon and potentially serious conditions. In adults, most cases are iatrogenic in origin, caused by surgical or endoscopic procedures, or mechanical ventilation. A case related to coronary angioplasty has even been reported. Chest trauma, both open and closed, is another common cause. They have also been reported in connection with other less common conditions such as gastric or esophageal perforation with the formation of pericardiac fistulas, asthma attack, pneumonia, diabetic ketoacidosis, and cocaine use. Some spontaneous cases have also been reported.1–4
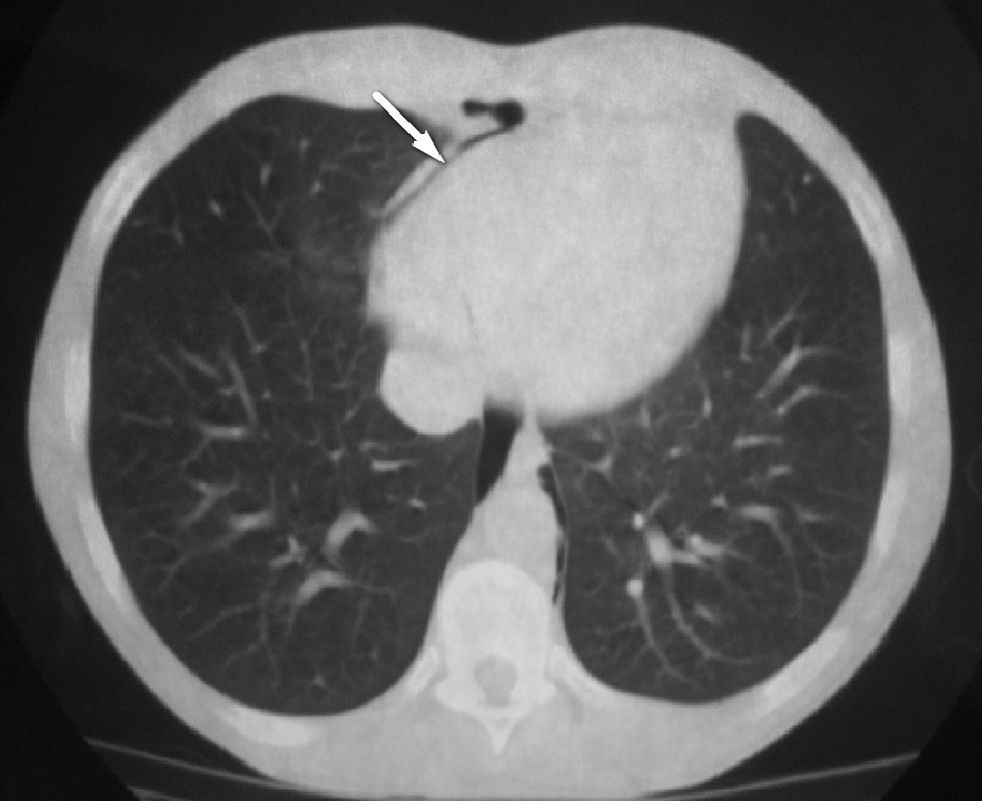
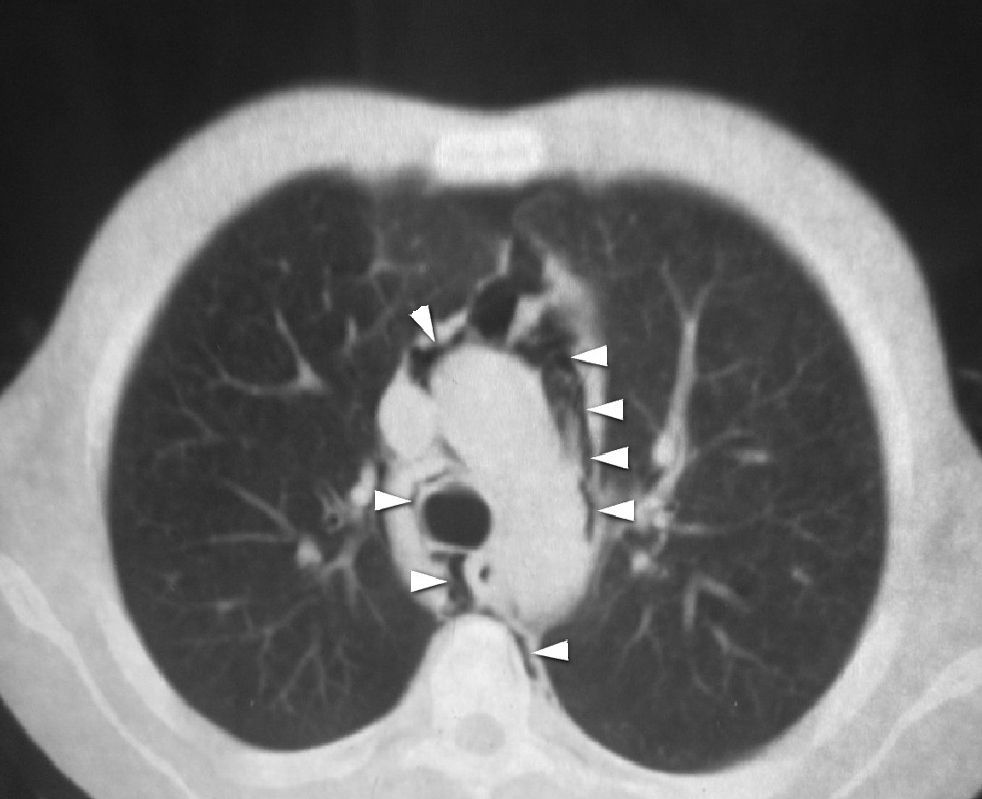
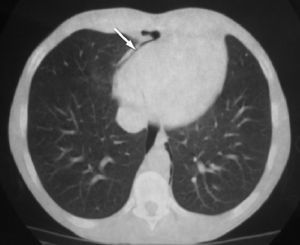
We report the case of a 23-year-old male patient with type 1 diabetes mellitus starting three years before with no chronic complications and poor metabolic control (glycosylated hemoglobin, 8.5%). The patient smoked one pack of cigarettes daily and was a habitual cocaine user. He attended the emergency room for vomiting over the previous 24h. The patient reported no chest pain or dyspnea. A physical examination revealed a dehydrated patient with a heart rate of 100bpm and blood pressure values of 100/60mmHg. Cardiopulmonary auscultation was normal. Laboratory test findings included metabolic acidosis with venous pH of 6.98, plasma glucose of 671mg/dL, and positive urinary ketones consistent with diabetic ketoacidosis. A urine drug screen was positive for cocaine. An electrocardiogram showed no findings of interest. Chest X-rays showed a left paracardiac radiolucent band and air levels in the mediastinum and subcutaneous cell tissue in the neck. Based on these findings, a computed tomography scan (CT) was performed, which confirmed the presence of air in the mediastinal space and anterior pneumopericardium and ruled out disease in the lung parenchyma (Figs. 1 and 2). An echocardiogram ruled out the presence of cardiac tamponade. Treatment was started with water and electrolyte replacement and intravenous rapid insulin, which led to a gradual improvement in his general state of health and a normalization of blood glucose and the acid–base balance. The course of pneumopericardium and pneumomediastinum was satisfactory, with progressive and spontaneous resolution within a week.
In the reported patient, pneumopericardium and pneumomediastinum had two potential causes, namely diabetic ketoacidosis and cocaine use. In a patient with diabetic ketoacidosis, their occurrence is explained by increased thoracic pressure and a change in the gradients in lung alveoli secondary to vomiting. However, pneumopericardium and pneumomediastinum occur before the start of vomiting in some cases, the etiology of which is not clear.5 As regards cocaine, pneumopericardium and pneumomediastinum have very rarely been reported in relation to the use of this drug. The mechanism has not been fully elucidated, but may consist of alveolar overpressure, which would cause alveolar rupture with a leaking of air contents. Pneumopericardium and pneumomediastinum are often secondary to the mechanical ventilation used in patients in a critical condition secondary to the use of the drug. Spontaneous cases are extremely rare.4,6
The main symptoms of these patients are pleuritic chest pain and dyspnea, but the condition may also be incidentally found in chest X-rays from asymptomatic patients such as the one reported here. Although it does not appear in all patients with pneumomediastinum, a highly characteristic sign in cardiac auscultation is a crunching sound synchronous with heart beat at the anterior chest area (Hamman's sign).7
Chest X-rays represent a very helpful tool and are often sufficient to establish a diagnosis. CT allows for more precise identification of air location and for etiological diagnosis in some cases. There are a number of radiographic findings that may be of help for the differential diagnosis of both conditions. Thus, in pneumopericardium, the air surrounding the heart does not extend beyond the origin of the great vessels, and changes in air location with patient position are characteristic. In pneumomediastinum, the air is distributed throughout the mediastinum and structures such as the aortic arch, trachea, and bronchi, and may even extend to the neck.
The course of the condition is benign in most patients, and symptomatic treatment only is required. However, some complications have been reported, including pressure pneumopericardium and an association with pneumothorax, pneumorrhachis, and mediastinitis.8
It may be concluded that pneumopericardium and pneumomediastinum should be considered in differential diagnosis of chest pain. Fully asymptomatic patients also exist, which makes diagnosis difficult. Chest X-rays should be performed in all patients with diabetic ketoacidosis, not only to rule out infection as the cause of diabetic decompensation, but also to assess the presence of pneumopericardium and pneumomediastinum On the other hand, although the most common cardiac complications of cocaine are myocardial ischemia, arrhythmia and sudden death, myocarditis, and dilated cardiomyopathy, it should not be forgotten that cocaine may also cause pneumopericardium and pneumomediastinum.
Please cite this article as: Garcipérez de Vargas FJ, Gómez Barrado JJ, Moyano Calvente SL, Amaya García MJ, Marcos G. Neumopericardio y neumomediastino en un paciente diabético y consumidor de cocaína. Endocrinol Nutr. 2013;60:e3–e4.