To conduct a prospective study in patients with type 2 diabetes mellitus (T2DM) with no microvascular complications, analyzing the association between various baseline risk factors and development of microvascular complications at follow-up.
MethodsA prospective, observational study in 376 patients with T2DM enrolled in 2004. The clinical end-point was urinary albumin excretion (UAE) > 30mg/24h and/or presence of retinopathy at follow-up in 2007. Baseline variables included age, gender, duration of T2DM, fasting plasma glucose, glycated hemoglobin (HbA1c), systolic and diastolic blood pressure, body weight, height, body mass index, waist circumference, total cholesterol, triglycerides, high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), high sensitive C-reactive protein (hs-CRP), fibrinogen, UAE, creatinine, smoking status, exercise, alcohol consumption, use of hypoglycemic and lipid-lowering drugs, antihypertensive medications, and other data related to family history of diabetes and risk factors.
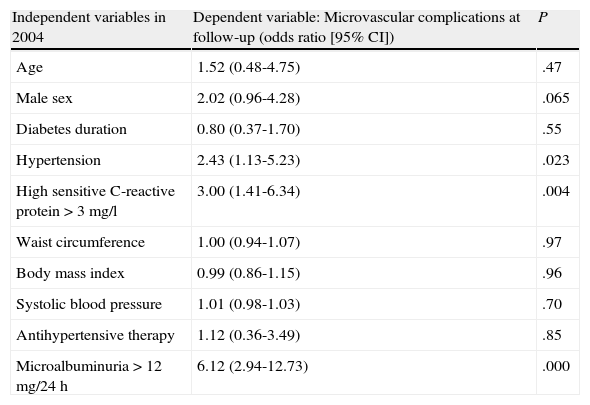
ResultsNinety-five subjects (25.2%) developed a microvascular complication at the end of the follow-up period. In logistic regression analyses, the main independent risk factors were UAE >12mg/24h (odds ratio [OR]: 6.12; P=.000), hs-CRP> 3mg/L (OR: 3.00; P=.004), and hypertension (OR: 2.43; P=.023).
ConclusionsUAE levels higher than 12mg/24h, hs-CRP >3mg/L, and presence of hypertension were all independent risk factors for development of microvascular complications in patients with T2DM studied.
Realizar un estudio prospectivo en sujetos con diabetes mellitus tipo 2 (DM2) sin complicaciones microvasculares, analizando la asociación entre varios factores de riesgo al inicio y el desarrollo de complicaciones microvasculares durante el seguimiento.
MétodosEstudio prospectivo, observacional en 376 sujetos con DM2 incluidos en 2004. El objetivo clínico final fue la excreción urinaria de albúmina (EUA) > 30mg/24h y/o presencia de retinopatía al final del seguimiento en 2007. Basalmente las variables fueron: edad, sexo, duración de la diabetes, glucosa plasmática en ayunas, hemoglobina glucada (HbA1c), presión arterial sistólica y diastólica, peso, talla, índice de masa corporal, circunferencia de la cintura, colesterol total, triglicéridos, colesterol unido a lipoproteína de alta densidad (c-HDL), colesterol unido a lipoproteína de baja densidad (c-LDL), proteína C reactiva de alta sensibilidad (PCR-as), fibrinógeno, EUA, creatinina, tabaquismo, ejercicio, consumo de alcohol, utilización de medicación hipoglucemiante, hipolipemiante e hipotensora, y otros datos relacionados con los antecedentes familiares de diabetes y factores de riesgo.
ResultadosAl final del seguimiento 95 sujetos (25,2%) desarrollaron una complicación microvascular. En el análisis de regresión logística, los principales factores de riesgo independientes fueron la EUA > 12mg/24h (odds ratio [OR]: 6,12; p=0,000), la PCR-as > 3mg/l (OR: 3,00; p=0,004) y la hipertensión (OR: 2,43; p=0,023).
ConclusionesLos niveles de EUA superiores a 12mg/24h, la PCR-as > 3mg/l y la presencia de hipertensión fueron factores de riesgo independientes para el desarrollo de complicaciones microvasculares en los sujetos con DM2 estudiados.
Diabetic nephropathy has a cumulative prevalence of 30%-40% in patients with type 2 diabetes mellitus (T2DM) and is currently the leading cause of end-stage renal disease.1 There are several markers predicting for the risk of developing renal failure in T2DM patients.2 However, microalbuminuria remains the main and most widely used marker of diabetic renal damage in clinical practice. It is also a marker of organ dysfunction, and has been shown to be associated with an increased risk of cardiovascular morbidity and mortality in T2DM patients.3 The earliest clinical evidence of nephropathy is occurrence of abnormal urinary albumin levels (30-300mg/day), referred to as microalbuminuria. The finding of microalbuminuria is a signal for screening for potential vascular disease and aggressive intervention to reduce all cardiovascular risk factors.4
Diabetic retinopathy is the most common microvascular complication in diabetes, and may lead to severe vision loss.5 Retinopathy lesions (microaneurysm, hemorrhage, cotton wool spots, hard exudates) may reliably be detected using direct ophthalmoscopy.6 People with diabetes should have regular fundus examinations to timely detect sight-threatening retinopathy lesions. Presence of retinopathy not only involves an increased risk of vision loss, but also a two to three-fold excess risk of cardiovascular disease.7
Microalbuminuria is associated with diabetic retinopathy in patients with T2DM and is a reliable marker of retinopathy.8 Moreover, the presence of diabetic retinopathy at baseline is associated with increased proteinuria, lower glomerular filtration rate (GFR), and a higher risk for end-stage renal disease and death in patients with T2DM.9
Several risk factors such as poor glycemic control, dyslipidemia, hypertension, obesity, and cigarette smoking act synergistically to develop nephropathy and retinopathy in patients with T2DM.10–12 Since progression to microvascular complications is likely to occur in a significant proportion of diabetic patients, the role of these risk factors needs to be further explored.
Our aim was to conduct a prospective study in T2DM patients with no microvascular complications (nephropathy and retinopathy), analyzing the association between a variety of baseline risk factors and occurrence of microvascular complications at follow-up.
Materials and methodsStudy population and designA prospective, observational study was conducted at Montes de Barbanza public health center, a specialized secondary referral center covering the 31 urban district of Madrid, Spain. Three hundred and seventy-six patients with T2DM aged ≥18years were enrolled in 2004. Inclusion criteria were normal urinary albumin levels (<30mg/24h) and absence of retinopathy (as assessed by funduscopy) at baseline. Exclusion criteria included type 1 diabetes mellitus, diabetic nephropathy (urinary albumin excretion [UAE] >30mg/24h, or plasma creatinine above normal reference values) and/or retinopathy at baseline.
The clinical end-point was a UAE level >30mg/24h and/or the presence of retinopathy at follow-up in 2007. Mean study period was 3.5years.
Subjects provided written informed consent. The study was approved by the local ethics committee and conducted in accordance with the principles described in the Declaration of Helsinki.
Clinical examination and biochemistryThe following variables were collected from the medical records of patients at baseline, in 2004: age, gender, diabetes duration, fasting plasma glucose (FPG), glycated hemoglobin (HbA1c), systolic (SBP) and diastolic blood pressure (DBP), body weight, height, body mass index (BMI), waist circumference (WC), total cholesterol, triglycerides (TG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), high sensitive C-reactive protein (hs-CRP), fibrinogen, UAE, creatinine, smoking status, exercise, alcohol consumption, use of hypoglycemic and lipid-lowering drugs, antihypertensive medications, and other data related to family history of diabetes and its risk factors.
Patient weight and height were measured to the nearest 0.1kg and 0.1cm respectively. BMI was calculated as weight divided by height squared (kg/m2). WC was recorded, according to Ashwell et al.,13 as the smallest girth between the rib cage and the iliac crest (it was located cranial to the umbilicus). A smoker was defined as someone consuming ≥ one cigarette/day or the equivalent using a pipe, or someone who had stopped smoking within 3 months of recruitment. Subjects were considered to practice exercise if they spent more than 3hours weekly walking or doing any other exercise or sports.
SBP and DBP were measured in all subjects after a 10-minute rest using a standard brachial cuff technique. Hypertension was defined as the need for antihypertensive therapy or untreated patients with SBP ≥ 130mmHg and/or DBP ≥ 80mmHg. Nephropathy was diagnosed if UAE levels > 30mg/24h were found in two of three urine samples taken during a three to six-month period. An Advira 2400 device (Siemens) was used to measure UAE by chemiluminescence.
Ophthalmoscopic examination was performed in all patients by two experienced ophthalmologists from our clinic by funduscopy (using slit lamp and contact lenses) and indirect ophthalmoscopy. If required, fluorescein angiography was performed. Retinopathy was diagnosed by the presence of any of the following lesions: microaneurysm, blot or flame-shaped hemorrhage, hard exudates, cotton wool spots, or evidence of laser treatment for retinopathy.
Biochemical parameters were measured after an overnight fast. FPG was measured by a glucose oxidase method. HbA1c was tested by high-performance liquid chromatography (reference range, 3.5% to 6.5%). Fibrinogen was measured by Clauss-Assay coagulometry (HORIBA ABX, Spain), and hs-CRP using a Vitros Chemistry System 5.1 FS analyzer (Ortho-Clinical Diagnostics, Johnson & Johnson, Madrid, Spain). HDL-C and TG were tested by enzymatic methods, and LDL-C was calculated using the Friedewald equation.
Patients requiring lipid-lowering therapy or untreated patients with total cholesterol > 5.0 mmol/L and/or TG > 1.7 mmol/L were considered to have dyslipidemia. Dyslipidemia phenotypes were defined as IIa: hypercholesterolemia, IIb: hypertriglyceridemia and IV: hypercholesterolemia + hypertriglyceridemia.
Based on the recommendations for adults with diabetes mellitus from the American Diabetes Association (ADA),14 the following were considered as acceptable target values: HbA1c <7.0%, FPG <7.2 mmol/L, HDL-C >1.1 mmol/L, LDL-C <2.6 mmol/L, TG <1.7 mmol/L, SBP <130mmHg, DBP <80mmHg, BMI <25kg/m2, and current non-smoking status. In addition, according to the WC cut-off points proposed by the World Health Organization as indicators of cardiovascular risk,15 WC measurements of <88cm in women and <102cm in men were considered as goals of body fat distribution.
Statistical analysisA Student’s t test for unpaired samples was used to compare mean levels with standard deviations (SD), and a Chi-square to compare proportions. A receiving operating characteristic (ROC) curve was performed and UAE sensitivity and specificity were calculated. The area under the ROC curve and 95% confidence interval (CI) were calculated. In addition, the optimum cut-off point of UAE for predicting microvascular complications during the follow-up period was sought. The optimum cut-off point was defined as the point on the ROC curve closest to the point (0, 1), i.e. a false positive rate of zero and a 100% sensitivity.
A value of hs-CRP > 3mg/L was chosen as the optimum cut-off point because hs-CRP levels > 3mg/L are associated to a high cardiovascular risk.
Logistic regression analyses were performed with development of nephropathy and/or retinopathy at follow up as dependent variables, and age, gender, diabetes duration, hypertension, hs-CRP >3mg/L, WC, BMI, SBP, UAE >12mg/24h, and other risk factors included at baseline as independent variables.
Odds ratios (OR) were estimated, with an OR >1.0 denoting a positive association. A value of P<.05 was considered statistically significant. All statistical analyses were performed using the SPSS for Windows statistical software package (version 13.0, Chicago, SPSS Inc.).
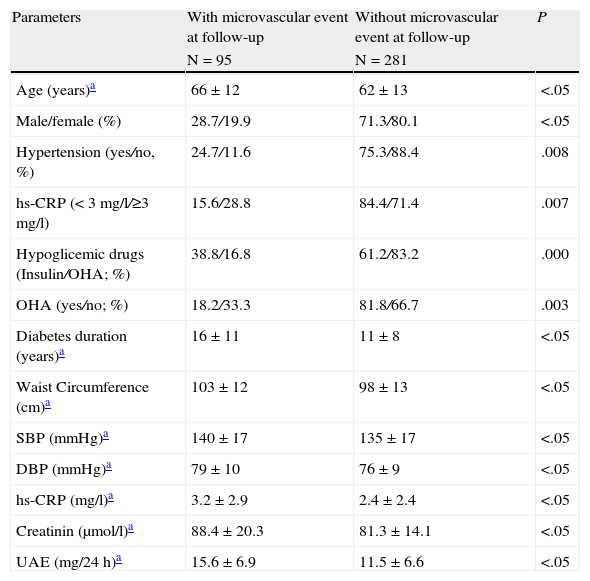
ResultsDuring 2004, 376 patients were recruited into the study. Ninety-five (25.2%) of these patients developed a microvascular complication at follow-up (77 nephropathy and 44 retinopathy). Twenty-six of them developed both retinopathy and nephropathy. No differential features were seen between the groups which developed retinopathy or nephropathy only and those developing both retinopathy and nephropathy. As compared to patients who did not develop microvascular complications at follow-up, those with such complications were predominantly male (P<.05), tended to be older (P<.05), to have higher hypertension rates (P=.008), hs-CRP levels >3mg/L (P=.007), to be taking more insulin (P=.000), and to receive less frequently oral hypoglycemic agents (P=.003). They were also more likely to have a longer mean diabetes duration and higher WC, SBP, DBP, creatinine, microalbuminuria, and hs-CRP values (P<.05 for all). The area under the ROC curve for microalbuminuria was 0.653±0.041 (P<.001), and the cut-off point for microalbuminuria with 67% sensitivity and 63% specificity was 12mg/24h.
Table 1 shows clinical and biochemical data for patients with T2DM who had no nephropathy and retinopathy at baseline in 2004, and classifies them into those who progressed to microvascular complications and those with no progression to complications at follow-up in 2007.
Prospective study, 2004-2007: clinical and biochemical data of type 2 diabetic subjects without nephropathy and retinopathy at baseline in 2004, classified as those who progressed to microvascular complications and those who did not progress to complications at follow-up, in 2007.
| Parameters | With microvascular event at follow-up | Without microvascular event at follow-up | P |
| N=95 | N=281 | ||
| Age (years)a | 66±12 | 62±13 | <.05 |
| Male/female (%) | 28.7/19.9 | 71.3/80.1 | <.05 |
| Hypertension (yes/no, %) | 24.7/11.6 | 75.3/88.4 | .008 |
| hs-CRP (< 3 mg/l/≥3 mg/l) | 15.6/28.8 | 84.4/71.4 | .007 |
| Hypoglicemic drugs (Insulin/OHA; %) | 38.8/16.8 | 61.2/83.2 | .000 |
| OHA (yes/no; %) | 18.2/33.3 | 81.8/66.7 | .003 |
| Diabetes duration (years)a | 16±11 | 11±8 | <.05 |
| Waist Circumference (cm)a | 103±12 | 98±13 | <.05 |
| SBP (mmHg)a | 140±17 | 135±17 | <.05 |
| DBP (mmHg)a | 79±10 | 76±9 | <.05 |
| hs-CRP (mg/l)a | 3.2±2.9 | 2.4±2.4 | <.05 |
| Creatinin (μmol/l)a | 88.4±20.3 | 81.3±14.1 | <.05 |
| UAE (mg/24 h)a | 15.6±6.9 | 11.5±6.6 | <.05 |
DBP: diastolic blood pressure; hs-CRP: high sensitive C-reactive protein; OHA: oral hypoglycemic agents; SBP: systolic blood pressure; UAE: urinary albumin excretion.
In the logistic regression analyses of baseline risk factors for development of microvascular complications at follow-up, the main independent risk factors were urinary albumin excretion > 12mg/24h (OR: 6.12; P=.000), hs-CRP> 3mg/L (OR: 3.00; P=.004), and hypertension (OR: 2.43; P=.023) (Table 2).
Prospective study, 2004-2007: logistic regression analyses in type 2 diabetic subjects with development of microvascular complications at follow-up as dependent variable, and age, gender, diabetes duration and risk factors among the patients without microvascular complications at baseline as independent variables.
| Independent variables in 2004 | Dependent variable: Microvascular complications at follow-up (odds ratio [95% CI]) | P |
| Age | 1.52 (0.48-4.75) | .47 |
| Male sex | 2.02 (0.96-4.28) | .065 |
| Diabetes duration | 0.80 (0.37-1.70) | .55 |
| Hypertension | 2.43 (1.13-5.23) | .023 |
| High sensitive C-reactive protein > 3 mg/l | 3.00 (1.41-6.34) | .004 |
| Waist circumference | 1.00 (0.94-1.07) | .97 |
| Body mass index | 0.99 (0.86-1.15) | .96 |
| Systolic blood pressure | 1.01 (0.98-1.03) | .70 |
| Antihypertensive therapy | 1.12 (0.36-3.49) | .85 |
| Microalbuminuria > 12 mg/24 h | 6.12 (2.94-12.73) | .000 |
CI: confidence interval.
In agreement with findings by other authors,16–19 in our study, baseline levels of UAE >12mg/24h and hs-CRP >3mg./L and the presence of hypertension were exceedingly strong independent risk factors for development of nephropathy and/or retinopathy in 376 patients with T2DM.
Several prospective and observational studies conducted on normoalbuminuric type 1 and type 2 diabetics followed up for long periods of time (between 5 and 10years) have found that several potentially modifiable risk factors, such as smoking, poor glycemic control, and UAE predict for the development of incipient and overt diabetic nephropathy16; duration of diabetes, abnormal HbA1c levels, hypertension, and high serum creatinine levels were significantly associated to microalbuminuria, and duration of diabetes, HbA1c, hypertension, and retinopathy were independent variables related to microalbuminuria17; total cholesterol levels, mean blood pressure, and HbA1c were the main factors associated with a decreased renal function and increased albuminuria18; and finally, increased baseline urinary albumin excretion rate, male sex, presence of retinopathy, increased serum cholesterol levels, HbA1c concentration, and age were risk factors for the development of incipient or overt diabetic nephropathy.19
Our findings confirm known predictive factors, such as UAE16,19 and hypertension,17,18 for the development of nephropathy in patients with type 2 diabetes. UAE is an independent risk factor for diabetic retinopathy in elderly type 2 diabetics.20 Cross-sectional studies in patients with T2DM have found microalbuminuria to be associated with diabetic retinopathy and to be a reliable marker of retinopathy8; diabetic maculopathy is closely associated with diabetic nephropathy and with several atherosclerotic risk factors, suggesting that these factors could have a significant role in the pathogenesis of maculopathy.12 Moreover, the presence of diabetic retinopathy at baseline in 1513 patients with T2DM and nephropathy was associated with increased proteinuria, lower GFR, and a higher risk for end-stage renal disease and death; these factors appeared to be independent from arterial blood pressure, glycemic control, hypercholesterolemia, and ethnicity.9 These data suggest that microalbuminuria may be a marker for the risk of development of proliferative retinopathy.
Our study suggests that UAE levels >12mg/24h are the most significant independent risk factor for development of nephropathy and/or retinopathy in the T2DM patients studied. However, according to current guidelines, the UAE cut-off level for progression to nephropathy is 30mg/24h.
In this study, hs-PCR levels > 3mg/L were an independent risk factor for development not only of diabetic nephropathy, but also of diabetic retinopathy. Inflammatory markers in early diabetic nephropathy in patients with type 2 diabetes are elevated and are independently associated with UAE. It may be hypothesized that released pro-inflammatory cytokines may participate in occurrence of kidney damage.21 Increased levels of sialic acid, a marker of inflammation, in serum and microalbumin were strongly related to the presence of microvascular complications such as diabetic nephropathy and retinopathy and some cardiovascular risk factors, such as hypertension and high waist to hip ratios, in Caribbean type 2 diabetic patients.22 The frequency of hs-CRP values higher than 1.0mg/L, which are thought to involve at high risk for cardiovascular disease, was also high in subjects with complicating hypertension and low in diabetic patients with retinopathy.23 On the other hand, fibrinogen might be more closely associated with diabetic microangiopathy than hs-CRP.24 Inflammatory parameters in T2DM patients with early stage nephropathy are independently associated with UAE.25 Elevated hs-CRP levels enhance the relationship between blood pressure (which has been shown to be the main determinant of microalbuminuria in diabetes and hypertension) and microalbuminuria. This interaction was found independently of other factors.23 It has been suggested that hs-CRP may be a marker of vascular disease, which indicates impaired self-regulation of glomerular pressure and/or dysfunction of glomerular endothelium. Both these factors may increase microalbuminuria.
This prospective study also showed hypertension to be an independent baseline risk factor for development of nephropathy, as previously reported by less extensive studies.17,18 Hypertension is a well known risk factor for development of kidney disease.18 Microalbuminuria is also associated with early renal damage due to hypertension. In the HOPE study,26 an association was found between hypertension and microalbuminuria in diabetic patients. High blood pressure is a significant marker for progression from microalbuminuria to nephropathy.27 Recent data have shown that an improved blood pressure control is beneficial to reduce the incidence of macular edema28 and suggest that renin-angiotensin system blockers might reduce the incidence of diabetic retinopathy.29
In conclusion, UAE levels >12mg/24h, hs-CRP levels >3mg/L, and hypertension were all independent risk factors for development of nephropathy and/or retinopathy in the T2DM patients studied. Decreases in levels of these risk factors in patients with T2DM without microvascular complications may prevent nephropathy and/or retinopathy. Further studies in similar populations are needed to confirm our results.
Conflicts of interestCristina Fernández Pérez has acted as a scientific advisor or consultant for Merck Sharp & Dohme, S.A., Spain.
Statistical analysis was supported by a grant from Merck Sharp & Dohme, S.A., Spain.