Minimally invasive parathyroidectomy (MIP) has been shown to be similar to bilateral neck examination in terms of efficacy and morbidity, with a level of evidence 1b1 (4 randomized, controlled trials). Prior neck surgery, particularly prior thyroid surgery (PTS) in patients with primary hyperparathyroidism (PHP), is considered by most surgeons to be a contraindication for MIP on the grounds that fibrosis and adhesions caused by prior surgery may cause a distortion of tissues and structure location and make access through a minimal incision difficult, as well as being associated with greater morbidity. The purpose of this letter is to review the use of MIP in the literature in patients with PHP and PTS, and to report the results of two patients who met these conditions and underwent surgery at our department.
Sixty-two patients with PHP underwent surgery from September 2010 to November 2014. The initial surgical approach was MIP and intraoperative PTH monitoring (IOPM) in 55 patients and direct bilateral neck exploration in seven patients.
The criteria for performing MIP included the surgical indication of PHP; no family history of PHP; unilateral gland disease located by at least one imaging test, if disagreement favored the result of scintigraphy; and adequate information to each patient based on his/her history. A history of prior neck surgery and PTS were not considered as reasons for exclusion.
Four patients (6%) had PTS. Two patients had undergone contralateral hemithyroidectomy, and although MIP was performed with an excellent outcome and they could be considered as having PTS, they were excluded from this study to avoid any addition of confounding factors. Thus, patients with surgery ipsilateral to adenoma location were considered for this study. These were two patients with a history of papillary thyroid carcinoma, of whom patient 1 had undergone total thyroidectomy, central neck lymphadenectomy (level VI), and functional left lymph node dissection (levels I–V), while patient 2 had undergone total thyroidectomy (Table 1). Preoperative laryngoscopy was performed in both patients. Preoperative localization was performed using scintigraphy with TC-99m-sestamibi in both patients, with SPECT/CT merged images in patient 2. Ultrasonography performed in both patients did not allow for visualization of the adenoma. Thus, scintigraphy was the only positive localization procedure in both cases.
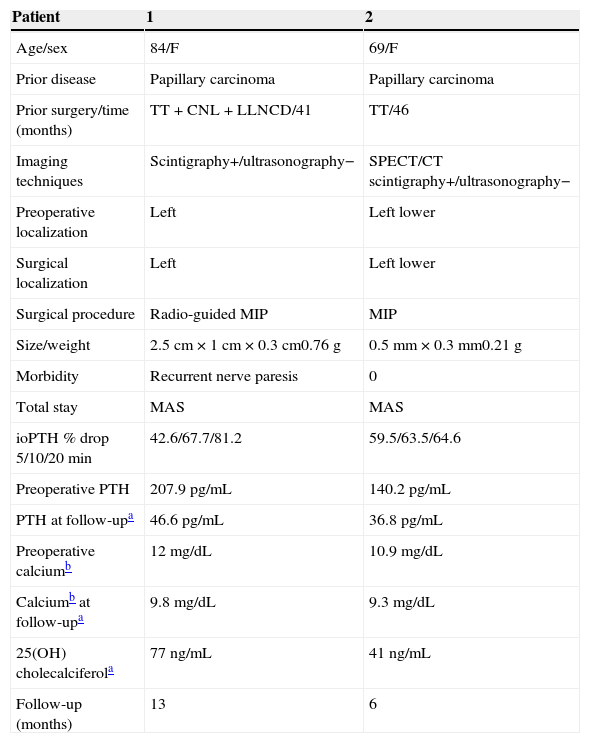
Patient data.
| Patient | 1 | 2 |
|---|---|---|
| Age/sex | 84/F | 69/F |
| Prior disease | Papillary carcinoma | Papillary carcinoma |
| Prior surgery/time (months) | TT+CNL+LLNCD/41 | TT/46 |
| Imaging techniques | Scintigraphy+/ultrasonography− | SPECT/CT scintigraphy+/ultrasonography− |
| Preoperative localization | Left | Left lower |
| Surgical localization | Left | Left lower |
| Surgical procedure | Radio-guided MIP | MIP |
| Size/weight | 2.5cm×1cm×0.3cm0.76g | 0.5mm×0.3mm0.21g |
| Morbidity | Recurrent nerve paresis | 0 |
| Total stay | MAS | MAS |
| ioPTH % drop 5/10/20min | 42.6/67.7/81.2 | 59.5/63.5/64.6 |
| Preoperative PTH | 207.9pg/mL | 140.2pg/mL |
| PTH at follow-upa | 46.6pg/mL | 36.8pg/mL |
| Preoperative calciumb | 12mg/dL | 10.9mg/dL |
| Calciumb at follow-upa | 9.8mg/dL | 9.3mg/dL |
| 25(OH) cholecalciferola | 77ng/mL | 41ng/mL |
| Follow-up (months) | 13 | 6 |
MAS, major ambulatory surgery; CNL, central neck lymphadenectomy; MIP, minimally invasive parathyroidectomy; TT, total thyroidectomy; LLNCD, left lateral neck complete dissection.
Both patients underwent surgery with MIP under IOPM and general anesthesia. A transverse 2.5–3cm incision was made at the theoretical location of the adenoma, and the thyroid cell was accessed laterally, outside the sternohyoid muscle, along the jugular-carotid vascular axis. Radio-guided surgery was performed in patient 1 because she had the additional distorting factor of lymphadenectomy of the central neck compartment. One hour after the administration of the radiotracer 99mTc-MIBI, a deposit with a count rate of 1452cps and a 2.3-fold adenoma-background ratio, which corresponded to the adenoma, was detected. IOPM consisted of measurements at baseline, before resection, and 5, 10, and 20min after resection. A decrease ≥50% 10min after resection as compared to the highest PTH level at baseline or before resection was considered to be an intraoperative confirmation of success. The biochemical cure criteria of IOPM were met in both cases.
The patients were eligible for major ambulatory surgery. At discharge, they received treatment consisting of 500mg of calcium/8h and 0.25μg of calcitriol/day to prevent postoperative hypocalcemia. The last dose was taken on the morning of the sixth postoperative day, and calcium and PTH levels were measured on day 7, and at month 1, month 6, and one year after surgery.
Patient 1 experienced transient paresis of the recurrent laryngeal nerve. A radio-guided procedure was used, and adenoma separation required significant manipulation of the nerve, which encroached on the pathological parathyroid. Laryngoscopy conducted at three months showed a complete recovery, with normal vocal cord mobility.
The patients were followed up for 13 and 6 months respectively. Both patients have maintained normal calcium levels.
A search was made in PubMed in all languages until January 31 2015 using the following strategy: ([minimally invasive parathyroidectomy] OR [focused parathyroidectomy] OR [targeted parathyroidectomy]) AND ([thyroid surgery] OR [thyroidectomy] OR [cervical endocrine surgery] OR [reoperative neck]). A total of 492 articles were found. The abstracts were reviewed, and any articles and their references that could contain information about MIP and PTS were analyzed.
Only three articles reporting MIP in patients with prior central neck surgery were found.2–4 Two of them3,4 were part of the same series, which was fully reported in the second article.4 Norman and Denham2 reported 21 patients with persistent PHP (14), recurrent PHP (3), and PHP with no prior parathyroid surgery (4). The latter four patients with PHP were the only ones who had undergone prior ipsilateral hemithyroidectomy or total thyroidectomy. All adenomas had been located with high-resolution scintigraphy with sestamibi only. Radio-guided MIP without IOPM was used, with no morbidity and a 100% cure rate. Seventeen patients were discharged on the same day.
Dimas et al.4 performed MIP without IOPM in 24 patients with PTS (total or subtotal thyroidectomy). Selection criteria included unilateral disease located before surgery by at least two imaging techniques, one of them scintigraphy with sestamibi. All patients were discharged on the first postoperative day. There was no morbidity, and disease persistence was reported in one patient.
Literature reports of MIP in patients with PTS are exceptional; the MIP series published do not specify this situation, or directly exclude patients with PTS from this approach5 or warn that it may prevent it.6 MIP in patients with persistent or recurrent PHP is more common.7
The use of IOPM has been recommended for patients who undergo MIP based on a single localization procedure.8–10 If no agreement exists in preoperative localization with sestamibi and ultrasound and the surgeon decides to perform MIP, the use of IOPM is indicated because the prevalence of multiglandular disease in this group is 17%.8–10
Although two patients, in addition to those previously reported, are insufficient for any conclusions to be drawn, MIP may be a valid option in patients with PTS, even with a single localization technique such as scintigraphy. The limited dissection involved and the targeted character of the procedure are theoretical advantages for the patient (a decreased risk of complications, a shorter hospital stay, a smaller scar) and decrease costs, although specific studies are needed to provide adequate evidence of this.
Please cite this article as: de la Plaza Llamas R, Ramia Ángel JM, Kühnhardt Barrantes AW, Gonzales Aguilar JD, Valenzuela Torres JC. Paratiroidectomía mínimamente invasiva en pacientes con cirugía tiroidea previa. Endocrinol Nutr. 2015;62:414–416.