Papillary thyroid microcarcinoma (PMC) is defined as a papillary carcinoma 1cm or less in size. PMC is a variant of papillary carcinoma, the most common thyroid cancer, which has a very good prognosis and in which distant metastases and death (0.4–1% per year) are exceptional.1
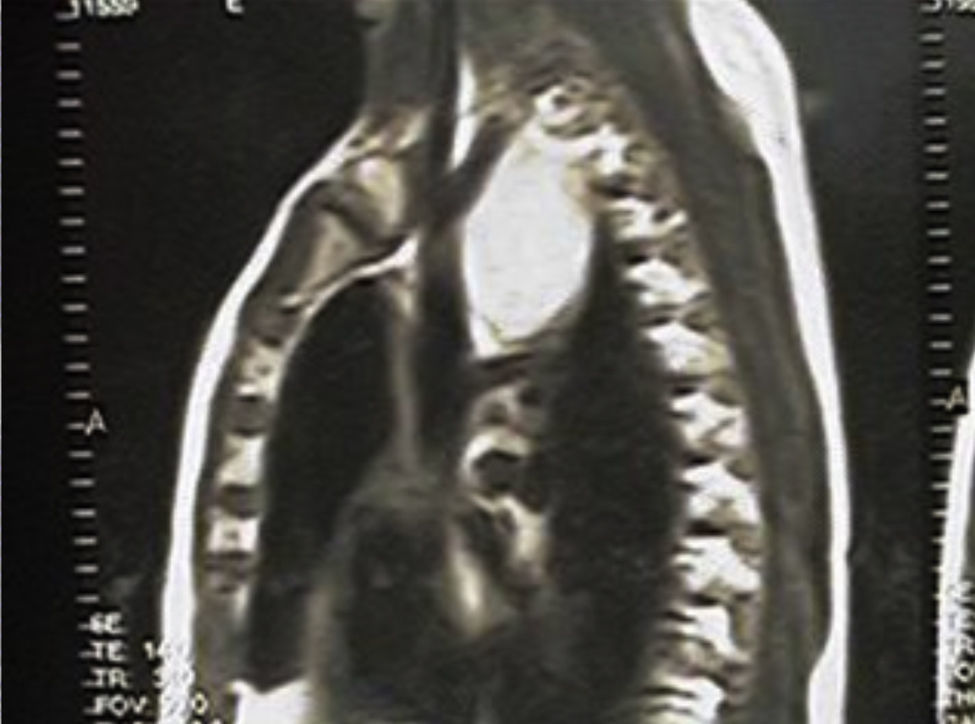
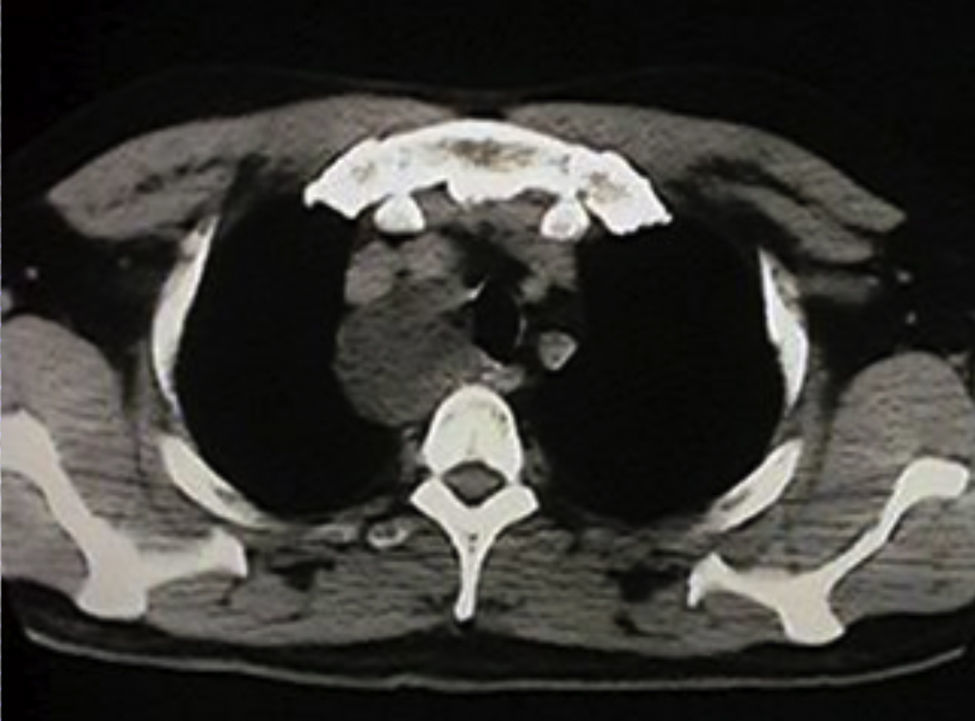
We report a patient who was diagnosed with metastasis of a papillary microcarcinoma as the result of an evaluation of a mediastinal mass. This was an asthmatic patient aged 38 years with no history of neck irradiation or family history of thyroid cancer. The surgery department referred the patient to the endocrinological department after surgery for a cystic tumor, 7cm in diameter, in the posterosuperior mediastinum (Figs. 1 and 2) after the histological study reported the finding in an intraoperative biopsy of a cystic wall of fibrous tissue with thyroid follicles without atypia and associated lymphocyte infiltrate consistent with pharyngeal pouch abnormalities. The final pathological study showed a cystic formation with a wall consisting of fibrous stroma with thyroid follicles, many of them with involutive phenomena, while others showed slight anisonucleosis and some “frosted glass” nuclei. Lymphoid tissue sectors coexisted with histiocyte clusters and calcification foci. The final diagnosis was metastasis from a papillary carcinoma in the cyst-like lymph node. The patient was clinically euthyroid, with a normal thyroid gland on palpation and no adenopathies on physical examination. Ultrasound examination of the thyroid and neck showed a hypoechoic Image 5.7mm×3.1mm in size in the left lobe with no pathological nodes. The functional thyroid study was within normal parameters, with negative antithyroid antibodies. Additional surgery performed in this case consisted of total thyroidectomy with bilateral level VI lymph node excision and the examination of both jugular chains. A delayed biopsy revealed a thyroid papillary microcarcinoma in the right lobe, 2mm in diameter limited by the gland and a small 5-mm follicular adenoma in the left lobe, with bilateral recurrent lymph nodes negative for metastasis. In a hypothyroid state with a TSH level of 85mIU/L and stimulated thyroglobulin level of 2.55ng/mL with negative antithyroid antibodies as measured by an ultrasensitive method, the patient was administered an ablation dose of 150mCi of radioactive iodine, and a whole body scan 1 week later showed radioisotope uptake in the thyroid bed only. Long-term follow-up showed negative total body scans with 2mCi of 131I, negative neck ultrasound examinations, and thyroglobulin levels on TSH inhibitory treatment and in a hypothyroid state following the discontinuation of levothyroxine treatment lower than 2ng/mL. The patient was therefore considered to be free of disease and subsequently underwent annual clinical, ultrasound, and laboratory monitoring. Tumor recurrence was not found after 11 years of follow-up.
Most papillary microcarcinomas remain occult (incidental microcarcinoma) in clinical examination and are found in autopsy studies in up to 36% of patients dying from non-endocrine causes.1 They are also commonly found incidentally in specimens from thyroidectomy performed for a benign disease. Very occasionally, papillary microcarcinoma becomes evident as palpable nodules or metastasis in the cervical lymph nodes. The incidence of papillary thyroid microcarcinoma increased by 100% between 1988 and 2005,2 and the detection of tumors less than 1cm in diameter increased by 49% between 1988 and 2002.3 In our own experience, the incidence of thyroid carcinoma has doubled in the past 20 years.4 It has been postulated that such an increase in detection is due to the widespread use of high-resolution thyroid ultrasound, which allows for the visualization of non-palpable nodules, as well as other imaging diagnostic methods used for various neck examinations, such as echo Doppler of the neck vessels, computerized axial tomography, magnetic resonance imaging, thyroid scintigraphy, and positron emission tomography.
The clinical significance of microcarcinoma is controversial because most series report very low mortality rates, which only exceptionally exceed 2%.5 The incidence of cervical lymph node metastases ranges from 17% to 43%.1 It has been reported that patients with tumors greater than 5mm in size also have metastasis in the lymph nodes of the central compartment with greater frequency.6 This subdivision between 5mm and 10mm and less than 5mm appears to be related to the prevalence of lymph node metastases (59% versus 13% respectively) and extrathyroid extension of the tumor (10% versus 3% respectively),1 i.e. the smaller the tumor, the lower the risk of metastasis. Lymph node metastases have been reported to be associated with multicentricity, extrathyroid infiltration, and disease recurrence.6 However, the presence of these lesions does not result in higher mortality. Extension outside the thyroid capsule, mainly microscopic, is seen in approximately 15–21% of cases, while vascular invasion may occur in approximately 3.5%.7 The development of distant metastases also correlates with tumor diameter, advanced age, and the presence of lymph node metastases at diagnosis.8 The reported prevalence of distant metastases ranges from 1.0% to 2.8%.1,7
The prognosis of papillary thyroid microcarcinoma is usually excellent. However, a significant number of patients may already have at diagnosis multifocal disease or locoregional nodal metastases, which are associated with an increased risk of recurrence from 14% in low risk patients to 86% in high risk patients. The American Thyroid Association currently recommends clinical staging, not only to predict the risk of recurrence or mortality, but to define the use of adjuvant postoperative treatments, including radioiodine ablation, as well as follow-up frequency and modality.9 While the clinical course of thyroid microcarcinoma is considered to be very good, and the different scientific societies think that radioiodine ablation is not required in very low risk patients, the reported case demonstrates that microcarcinoma may show in some cases aggressive behavior leading to distant clinical manifestations. In such cases, molecular analysis can be of value by showing the mutations associated with greater aggressiveness. In recent years, many markers have been assessed in order to optimize diagnostic accuracy and predict the aggressive behavior of tumors even in presurgical cytology samples. More recent prospective studies support the value of certain genetic (BRAF, Ras, RET/PTC) and protein (galectin-3) markers as diagnostic tools for these patients. Although they are not widely used in the clinical setting, the combination of some of these markers will allow in the near future for accurate diagnosis, and also in thyroid microcarcinoma.10
Clinically occult papillary thyroid carcinoma with extensive gross and microscopic metastases in cervical adenopathies is well documented in the literature, but the occurrence of a mediastinal cystic metastasis without clinically detectable metastases in the cervical lymph nodes, as in the reported case, is a rare event.
Please cite this article as: Faure EN, González AJ, Schwarzstein D, Lutfi RJ, Puig-Domingo ML. Microcarcinoma papilar de tiroides diagnosticado por una metástasis quistificada en el mediastino. Endocrinol Nutr. 2013;60:414–416.