Osteonecrosis is an ischemic process in the juxta-articular bone. Two forms of osteonecrosis are distinguished, one in which infarction occurs in bone marrow, causing no clinical signs, and another involving the cortical medulla, with a more florid clinical picture.
Multifocal osteonecrosis is defined as a disease affecting three or more separate anatomical regions. Its preferential locations include the femoral head, distal femur, proximal humeri, and calcanei.
As regards its pathogenesis, it has been related to long-term corticosteroid treatment, alcohol abuse, hemoglobinopathies, malignant tumors, human immunodeficiency virus, connective tissue disease, Gaucher's disease, or radiotherapy, with glucocorticoids being one of the causes in 5–25% of cases. No prior trigger is known in 40% of cases, and the condition is then considered idiopathinc.1
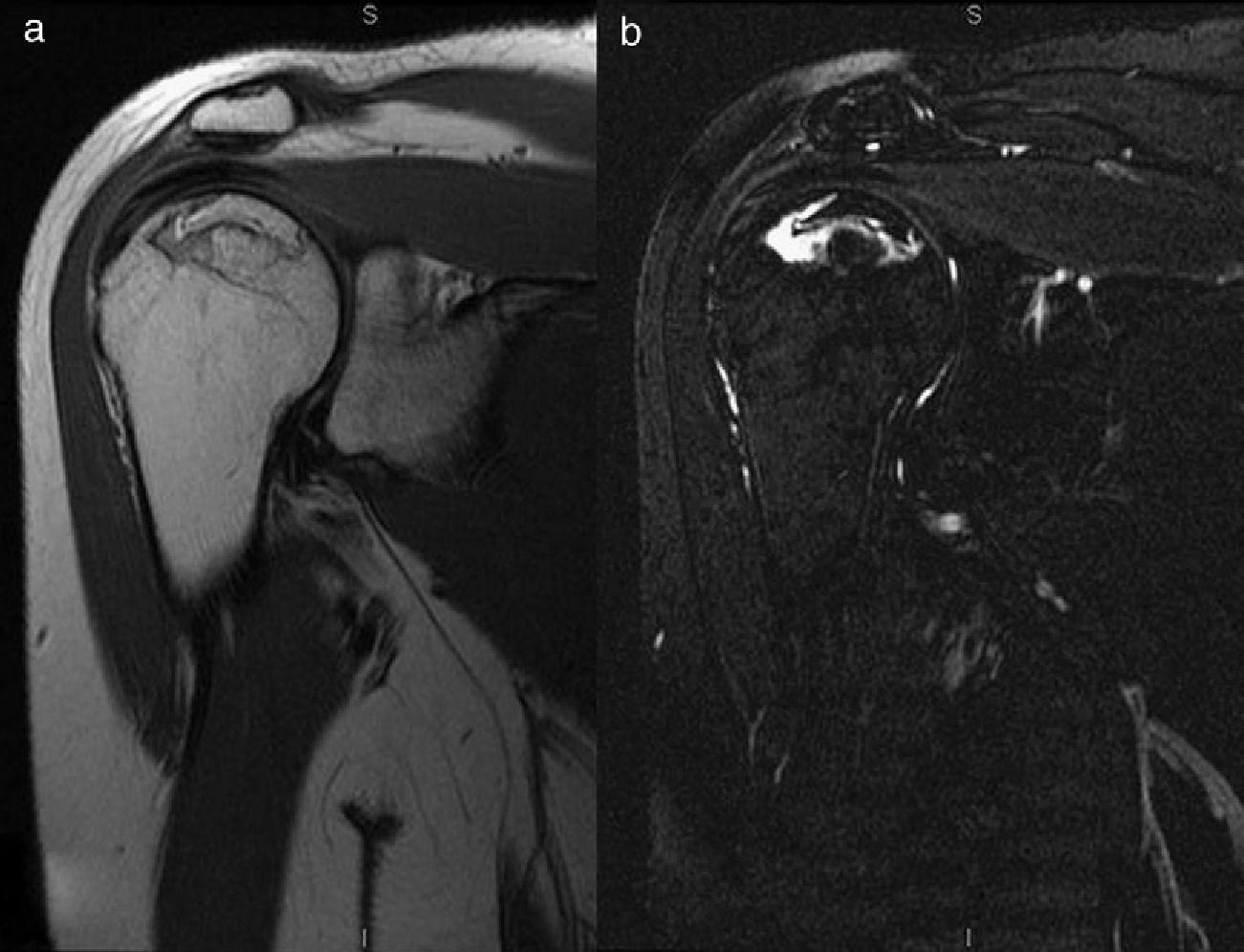
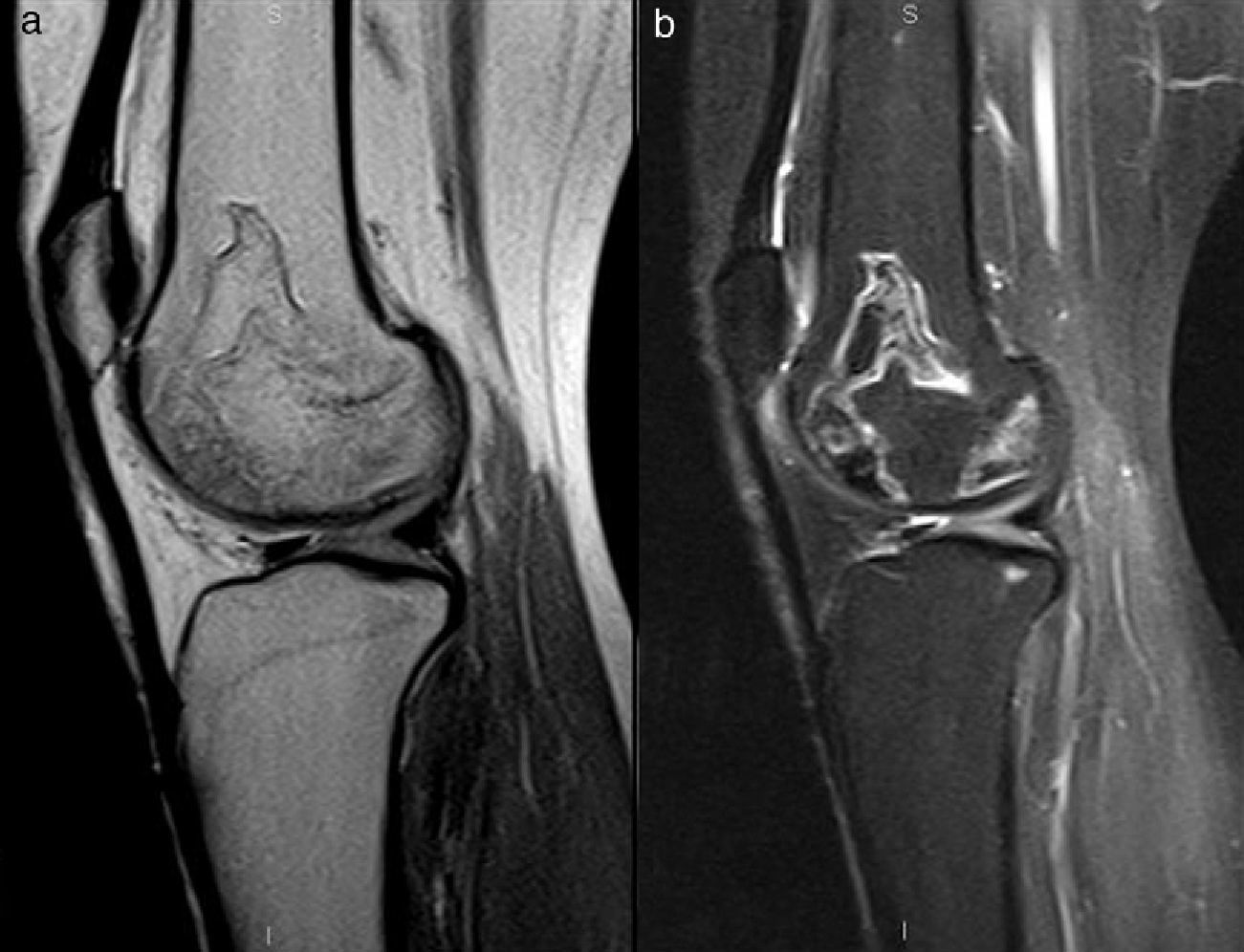
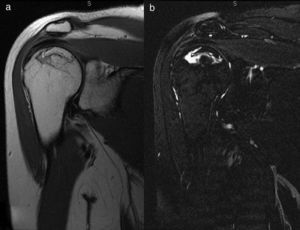
We report the case of a 32-year-old female patient who reported mechanical pain in both knees and was referred to the radiodiagnosis department for bilateral magnetic resonance imaging (MRI). Her history included, in addition to smoking five cigarettes daily, an infrachiasmatic suprasellar tumor detected by cranial MRI one year and a half before during work-up for infertility and increased prolactin levels. A pituicytoma inducing panhypopituitarism was diagnosed and surgery was performed. Hormone replacement therapy consisting of different drugs, including hydrocortisone at doses of 20mg in the morning and 10mg in the evening, was subsequently administered. Fourteen months later, and without having received higher hydrocortisone doses for any intercurrent condition, bilateral pain in the hips and shoulders (Fig. 1) led to MRI being performed, which revealed avascular necrosis in these locations. Surgery was performed on both heads, consisting of decompression and filling with a bone graft, and hydrocortisone dosage was decreased to 10mg in the morning and 5mg in the evening. At the time of evaluation, MRI was performed on both knees, revealing several lesions with signal intensity similar to that in the bone marrow, with geographical contours and peripheral hyperintensity in STIR sequence, in the femoral metaphysodiaphyseal region, some of which reached the condylar cortical surface, as well as the tibial epiphysis, consistent with bone infarcts (Fig. 2). Overall, the findings described were consistent with multifocal osteonecrosis secondary to corticosteroid treatment.
1.5T MRI of the right shoulder. Coronal proton density-weighted (1.a) and fat-saturated proton density-weighted (1.b) series were performed. A geographical lesion reaching the cortical surface with a pathognomonic signet ring sign is seen as a circumscribed subchondral hyposignal outlining the osteonecrosis and with a hyperintense halo inside, which is evident with fat saturation.
1.5T MRI of the left knee. A sagittal proton density sequence (2.a) and STIR are shown. Two lesions with characteristics similar to that described in Image 1, consistent with osteonecrosis and coming into contact with the anterior and posterior condylar cortical surface are shown.
Osteonecrosis is bone death with the collapse of its structure causing joint pain, bone destruction, or function loss.2 Several terms have been used as synonyms, but there are nuances that differentiate them. The term avascular necrosis should be used when bone involvement occurs in the epiphyseal region or subchondral bone. We will speak of bone infarcts when the involved areas are the metaphysis or diaphysis, although such infarcts may extend up to the epiphysis or subchondral bone.3 Avascular necrosis is usually post-traumatic, occurring after a femoral neck fracture or hip fracture-dislocation. In the absence of prior trauma, osteonecrosis is usually bilateral and occurs in younger subjects. It may be due to multiple causes, already mentioned.
There are two theories regarding the pathogenesis of bone infarcts secondary to the use of corticosteroids. According to the mechanical theory, osteonecrosis induced by steroids causes microfractures and bone collapse. The second theory attributes such infarcts to fat accumulation in bone marrow, fat embolism due to fatty liver, vasculitis, or blood hyperviscosity resulting from the use of such substances.4
In the pathological study of bone specimen including the bone infarct, four areas are distinguished: a central area of dead cells surrounded by an area of ischemic damage, an area of active hyperemia, and a normal tissue area.
The clinical course of osteonecrosis is unpredictable. The clinical signs depend on the affected site. In osteonecrosis of the hip, one of the main locations, the patient has pain in the gluteal region or hip which worsens on walking, going up and down stairs, and sitting, with difficulty in rotating. Early diagnosis is required in order to start treatment as soon as possible. While plain X-rays are the most accessible imaging procedure, they only detect the condition in advanced cases. MRI is the most sensitive test, and may detect osteonecrosis in its early stages.5 Imaging procedures should help to determine disease severity and guide treatment. The extent of epiphyseal involvement (established by several classifications as less than 15%, 15–30%, or greater than 30% of epiphyseal volume6) is the best predictor of bone collapse.7
There are several classifications of the stage of osteonecrosis. One of the most widely used is the Ficat classification, consisting of stages 0–IV. Grade 0 is defined by a double line in the contour of the bone that causes no symptoms when the symptomatic contralateral bone is examined, and grade IV is defined as bone collapse with cartilage destruction and joint space narrowing. Bone infarcts show a characteristic appearance in MRI8–11 with a hypointense peripheral halo in T1 related to the reactive sclerosis of serpiginous morphology. In T2-weighted sequences, the sign of a double peripheral line where a hypointense line meets a hyperintense inner margin is identified.
A study reported that 100% of patients with multifocal osteonecrosis had femoral head involvement, which was bilateral in 98% of cases.12 Therefore, the hips should be assessed in patients with multifocal involvement.
Treatment for bone infarcts ranges from analgesia and exercise to surgical decompression of the nucleus or bone cementation/graft to prevent bone collapse. Patients should be followed up for two years to monitor the adjacent joint and to perform total joint replacement if needed.
Please cite this article as: Ibáñez D, Martín MD, Rubio RÁ, Muel C. Osteonecrosis multifocal en el tratamiento corticoideo prolongado secundario a panhipopituitarismo: a propósito de un caso. Endocrinol Nutr. 2013;60:416–418.