To report the prevalence of impaired fasting glucose (IFG), undiagnosed and diagnosed diabetes, and their association to occupational categories in a representative sample of working population in Spain.
Materials and methodsA cross-sectional study of workers who attended routine medical check-ups from January 2007 to December 2007. A structured questionnaire was completed, and physical examinations and routine serum biochemical tests were performed. IFG was defined as fasting glucose levels ranging from 100 to 125mg/dl with no diagnosis of T1DM or T2DM; T1DM was defined as previous diagnosis of T1DM; and T2DM as previous diagnosis of T2DM, treatment with oral antidiabetic drugs or insulin or fasting glucose levels ≥126mg/dl, according to ADA criteria.
ResultsOf the 371,997 participants (median age 35 [interquartile range 29–44] years), 72.4% were male. Raw prevalence rates (95% CI) of IFG, undiagnosed (UKDM), and previously known type 2 (KDM2) and type 1 (KDM1) diabetes were 10.4% (10.3–10.5%), 1.3% (1.2–1.3%), 1.1% (1.1–1.2%), and 0.3% (0.3–0.3%), respectively. With the exception of KDM1, prevalence of these conditions increased with age and was greater among manual/blue-collar workers (12.1%, 1.5%, 1.3% and 0.3%, respectively) as compared to non-manual/white-collar workers (7.3%, 0.8%, 0.8% and 0.3%, respectively). Age- and sex-adjusted prevalence rates of IFG, UKDM and KDM2 were 13.1%, 2.0% and 2.4%, respectively.
DiscussionIn this sample of Spanish working population, impaired glycemic profiles were common. Prevalence rates of IFG and T2DM were high among blue-collar workers (except for T1DM). These data emphasize the need for earlier structured preventive schemes.
Describir la prevalencia de glucemia alterada en ayunas (GAA), diabetes no diagnosticada y diabetes, y su asociación con categorías profesionales en una muestra representativa de población trabajadora en España.
Material y métodosEstudio transversal en trabajadores que realizaron revisión médica entre enero y diciembre de 2007. Se realizó exploración física, análisis de sangre y se utilizó un cuestionario estructurado. Se definió GAA como glucosa en ayunas 100-125mg/dl sin diagnóstico de diabetes tipo 1 (DM1) o diabetes tipo 2 (DM2); DM1 como diagnóstico previo de DM1; y DM2, según criterios ADA, como diagnóstico previo de DM2, tratamiento con antidiabéticos orales o insulina, glucosa en ayunas≥126mg/dl.
ResultadosDe los 371.997 participantes (mediana de edad 35 [rango intercuartílico 29-44] años), el 72,4% eran varones. La prevalencia (IC 95%) de GAA, diabetes no diagnosticada y DM2 y DM1 conocidas previamente fue del 10,4% (10,3-10,5%); 1,3% (1,2-1,3%); 1,1% (1,1-1,2%) y 0,3% (0,3-0,3%), respectivamente. Excepto para DM1, la prevalencia aumentó con la edad y fue mayor en trabajadores manuales (12,1; 1,5; 1,3; y 0,3% respectivamente) que en trabajadores no manuales (7,3; 0,8; 0,8; y 0,3% respectivamente). La prevalencia de GAA, diabetes no diagnosticada y DM2 ajustada por edad y sexo fue del 13,1, 2,0 y 2,4% respectivamente.
ConclusionesEn esta muestra de población trabajadora en España, las alteraciones del perfil glucémico fueron frecuentes. En trabajadores manuales (excepto en DM1) las prevalencias de GAA y DM2 fueron mayores. Estos datos resaltan la necesidad de programas preventivos de intervención más temprana.
Intricate and heterogeneous, social, healthcare and cultural circumstances underlie the past and projected steady increase in the prevalence of type 2 diabetes.1 The increasingly younger age of affected individuals demands effective screening and management strategies.1,2 Determining population patterns of diabetes and prediabetes can help to refine preventive interventions.
The first robust national estimate of the prevalence of diabetes and prediabetes in Spain was published recently, revealing a worryingly high age-and sex-adjusted prevalence of diabetes mellitus (undiagnosed plus diagnosed) of 13.8%.3 These data suggest a potential increase in diabetes prevalence in the years to come, stressing the need for effective nationwide programs to prevent progression to diabetes, promotion of healthy eating habits and increasing physical activity among young people.
Investigating health risks in workers may be of particular interest as they constitute a large, mostly young and “healthy” population, with a high preventive potential.4 For its detection and treatment, it is necessary to take advantage of all appropriate occasions where the subject is in contact with the health system. In this context, programs to identify and control risk factors in the workplace can be more efficient than those conducted in conventional health centers.4
This research is part of the ICARIA study (Ibermutuamur CArdiovascular RIsk Assessment)5–7 that aims to detect, stratify and prevent cardiovascular risk in workers affiliated to Ibermutuamur Prevention Society. This Society is specifically focused on preventing diseases and accidents by monitoring and promoting the health of workers through routine annual medical check-ups being in Spain very frequent and even mandatory (in certain productive activities) for the employer to offer the workers access to this occupational health service.
Lack of physical activity and unhealthy diet have been identified as factors contributing to the development of obesity, diabetes and cardiovascular disease (CVD).8 Likewise, a close relationship between obesity and type 2 diabetes mellitus is well known,9–11 that relationship is particularly of interest in this population due to the high and increasing prevalence of obesity and overweight in the Spanish working population especially in male blue-collar workers.11 Thus, young and middle-aged people in their active working years are at increased risk of diabetes and its related complications, with major implications both for work productivity and for overall public health and public finances.12
An inverse relationship exists between social position and incidence of diabetes.8 Workers in lower employment grades have reported higher incidence of diabetes than those in higher employment grades. However, little is known about the relationship of occupational categories and the prevalence of impaired fasting glucose (IFG).
Bearing those two facts in mind the aim of the study was to describe the prevalence of IFG, and undiagnosed diabetes, diabetes and the association with occupational categories in a nationwide sample of the Spanish working population.
Materials and methodsThis was a cross-sectional study of 375,571 workers, 72.3% male (M), median age 35 (P25=29; P75=44) years. All subjects underwent a routine medical check-up from January 2007 to December 2007 by Ibermutuamur Prevention Society. A structured questionnaire, physical examination and standard serum biochemical analysis were performed. Blood samples were analyzed in central laboratories (95% of the samples in Madrid, Murcia, and Alicante) and in sub-contracted laboratories in Oviedo, Palma de Mallorca, Palencia, Tenerife, and Zamora (the remaining 5%). The Spanish Society of Clinical Biochemistry and Molecular Pathology's (SEQC) quality control recommendations were followed. The variation coefficient for the main serum analyses was within the range accepted by the SEQC.
The specific occupation of workers was coded according to the 1994 Spanish National Classification of Occupations.13 Workers were classified as non-manual (white-collar) and manual workers (blue-collar), as previously described. IFG was defined as a fasting glucose level between 100 and 125mg/dl, without T1DM or T2DM diagnosis;14 T1DM was defined as the presence of a previous diagnosis of T1DM; and T2DM was defined as the presence of previous T2DM diagnosis or antidiabetic treatment or fasting glucose level ≥126mg/dl.14
Participants were considered to have diagnosed diabetes if the physician performing the check-up could verify that the participant had received such a diagnosis (not self-reported) in the past (known type 1 [KDM1] or type 2 [KDM2] diabetes, excluding gestational diabetes).
Adult Treatment Panel III (2001)15 and European Society of Cardiology (2003)16 criteria were used to classify patients with dyslipidemia and hypertension (systolic BP ≥140mmHg and/or diastolic BP ≥90mmHg), respectively. Additionally, all participants who were taking antihypertensive medication or who had a prior diagnosis of hypertension were classified as hypertensive.
Data analyses were performed in SAS (SAS Institute Inc., Cary, United States). Data from categorical variables are given as percentages with 95% confidence intervals (95% CI). The data from 3574 check-ups (1%) were incomplete and were not analyzed. Data from continuous variables are given as means±standard deviations (SD). Figures were rounded to the first decimal place. Comparison of categorical variables was carried out using the X2 test and the Cochran–Armitage test was used for the analysis of trends. Continuous variables were compared using one-way analysis of variance. In addition, three multiple logistic regression models were used to explore factors associated with the diagnosis of type 2 diabetes, unknown diabetes and impaired fasting glucose, including as explanatory variables socio-demographic data (gender; age in years, categorized into five groups: <30, 30–39, 40–49, 50–59 and >60 years; and BMI in kg/m2, categorized into five levels and rounded to one decimal place: <18.5 or low weight, 18.5–24.9 or normal weight, 25–29.9 or overweight, 30–39.9 or obesity, and >40 or morbid obesity) and the cardiovascular risk factors evaluated at medical check-ups. The significance level was set at α=0.01.
The 2012 update of the Spanish Population Registry17 was used to calculate the age- and sex-adjusted prevalence of diabetes (UKDM+KDM2) for the Spanish general population.
The study was approved by Ibermutuamur's Scientific Ethics Committee. Data were treated confidentially in accordance with current Spanish legislation on data protection. All participants provided a written consent for the utilization of their personal data for the purposes of the Ibermutuamur CArdiovascular RIsk Assessment (ICARIA) project, which included the current research. The study respected the principles of the Declaration of Helsinki.
ResultsOf the 371,997 participants analyzed, 72.4% were men, median age was 35 (interquartile range 29–44) years and 62.5% were aged ≤39 years.
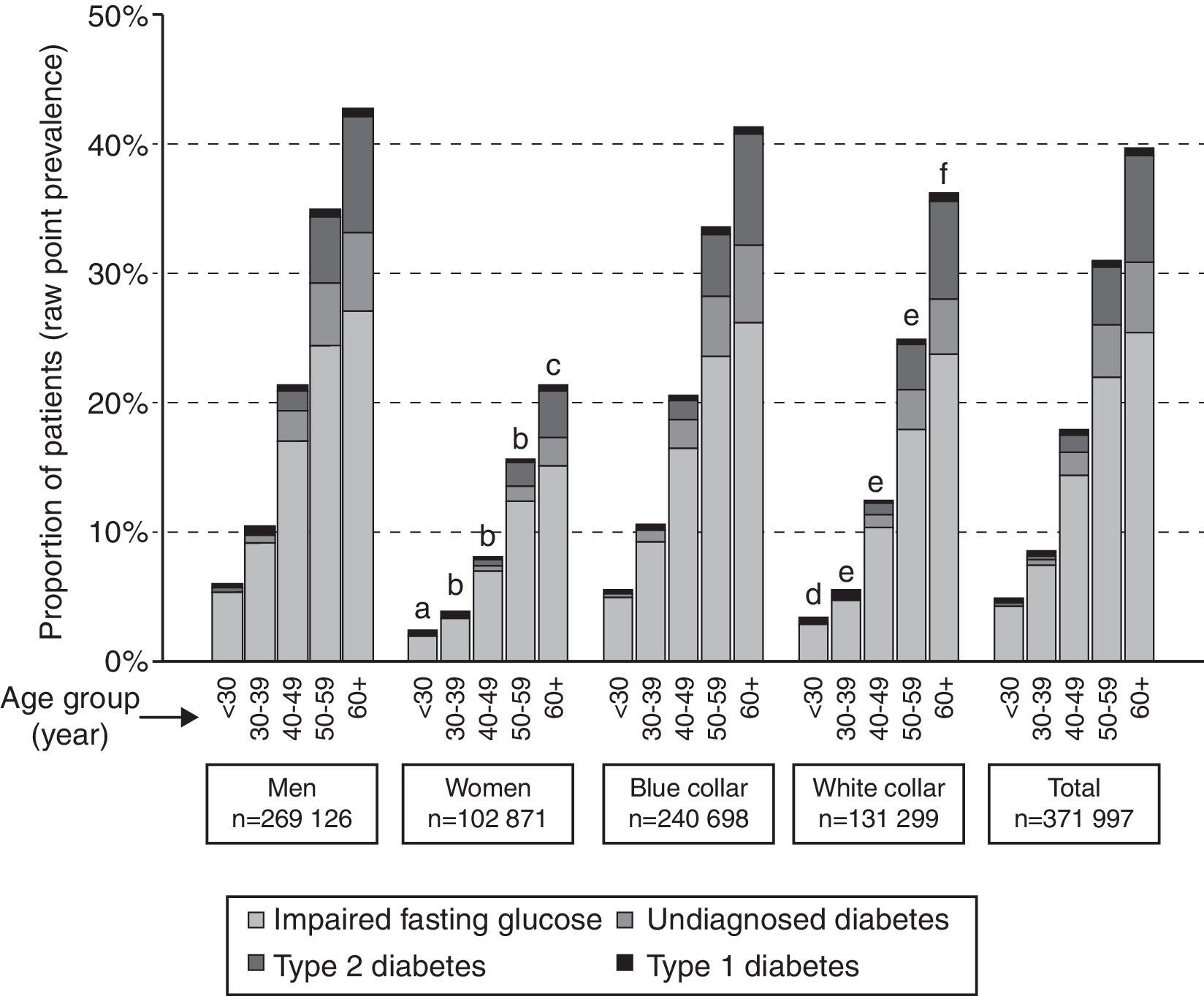
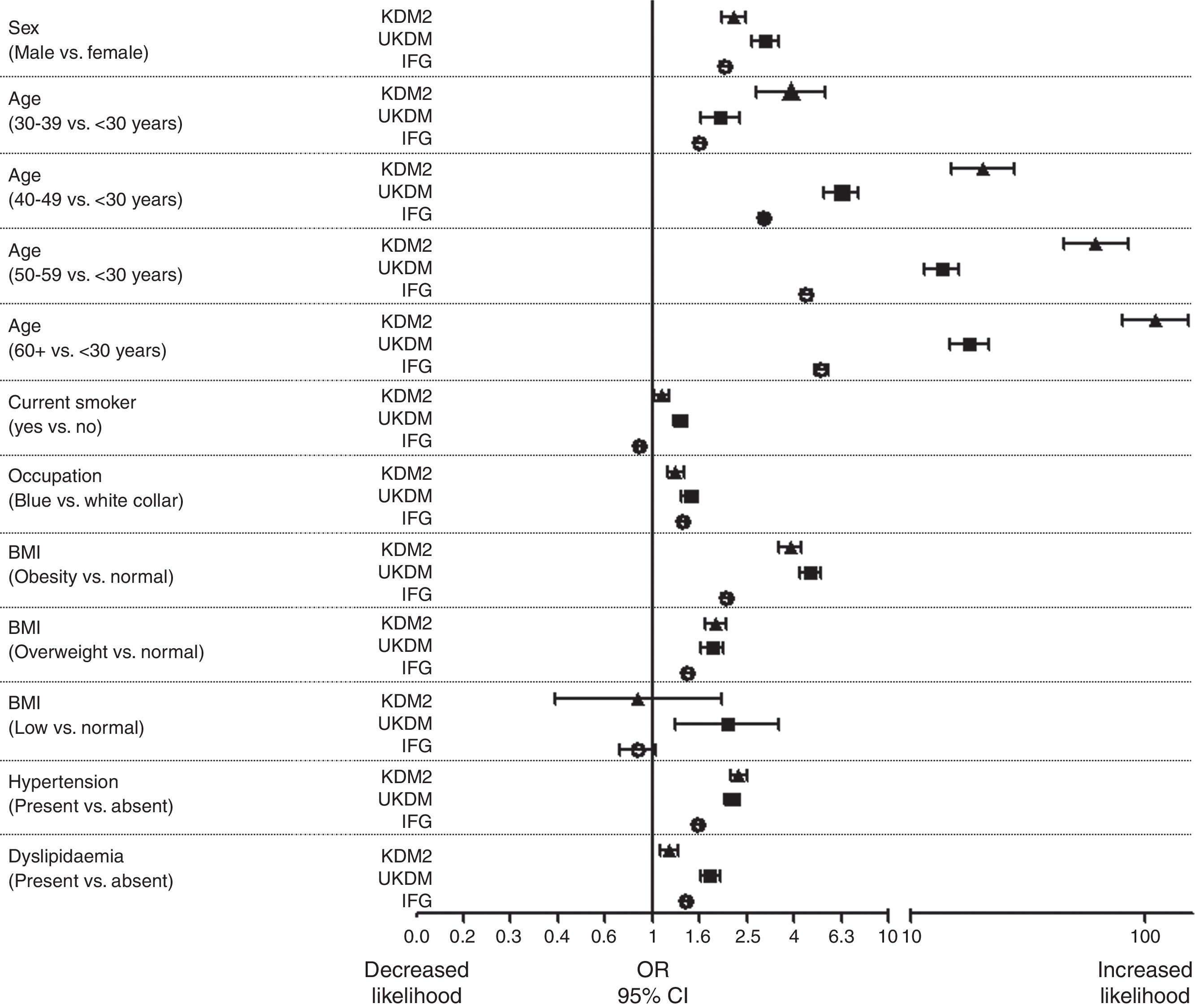
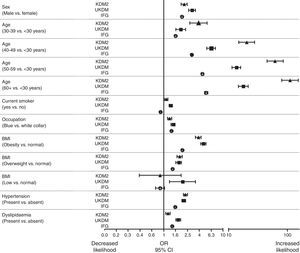
The raw (95% CI) prevalences of IFG, UKDM, KDM2 and KDM1 were 10.4% (95% CI 10.3–10.5%), 1.3% (95% CI 1.2–1.3%), 1.1% (95% CI 1.1–1.2%) and 0.3% (95% CI 0.3–0.3%), respectively. With the exception of that for KDM1, prevalences increased with age (Fig. 1). The prevalences of IFG and diabetes (UKDM+KDM2) adjusted by age and sex were 13.1% and 4.4% (2.0%+2.4%), respectively. Additionally, IFG (12.1% vs 7.3%), UKDM (1.5% vs 0.8%) and KDM2 (1.3% vs 0.8%) were more prevalent among blue-collar workers than among white-collar workers and prevalence of KDM1 was similar in blue-collar and white-collar workers (0.3% vs 0.3%), especially at young ages, and UKDM and KDM2 were more prevalent among men than among women (Fig. 1). Multivariate logistic regression analyses showed that male gender, increasing age, being a blue-collar worker, being overweight/obese, presenting with hypertension and presenting with dyslipidemia were all associated with a greater likelihood of IFG, UKDM or KDM2 (Fig. 2).
Prevalence of glucose metabolism disorders according to sex, age and occupational categories. a: p<0.001 vs males except for type 2 diabetes (p<0.05) and type 1 diabetes (NS); b: p<0.001 vs males for all categories; c: p<0.001 except for type 1 diabetes; d: p<0.001 vs blue collar except for type 2 diabetes (p<0.01) and type 1 diabetes (NS); e: p<0.001 vs blue collar except for type 1 diabetes; f: p<0.001 vs blue collar only for undiagnosed diabetes.
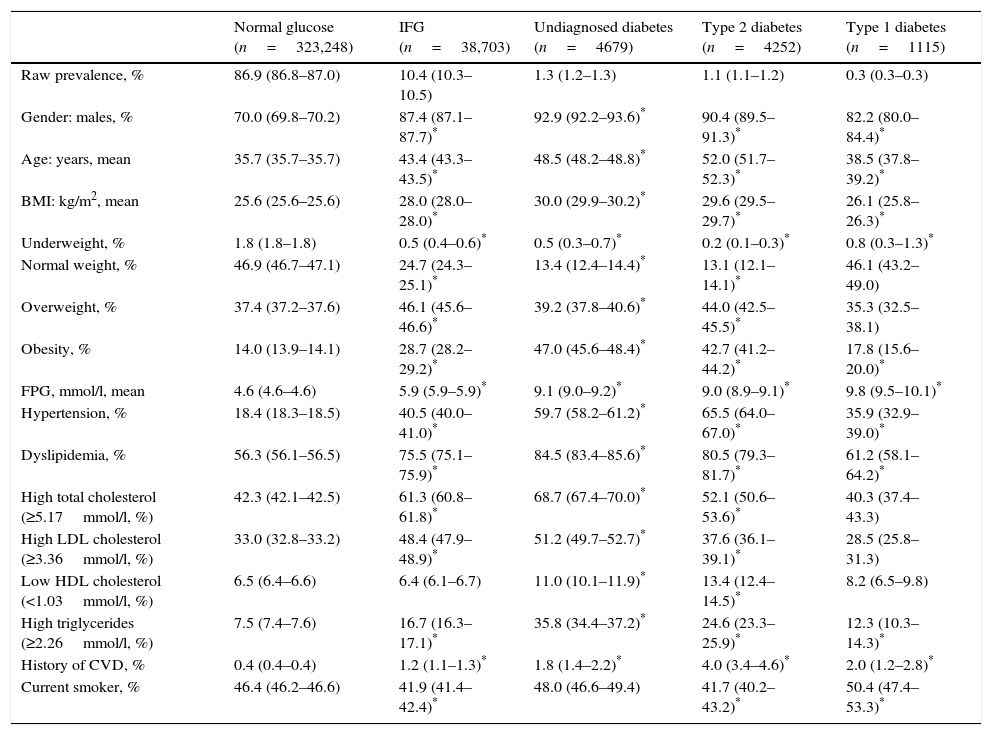
Table 1 presents the clinical characteristics and the status of several metabolic indicators related to cardiovascular risk for the study groups. Overweight/obesity, dyslipidemia and hypertension were common in workers with IFG or KDM2. People with KDM1 had a risk profile intermediate between normoglycemic individuals and those with IFG, KDM2 or UKDM. Participants with UKDM, although younger, presented a cardiovascular risk profile that was similar or worse than that of participants with KDM2 (Table 1).
Socio-demographic and clinical characteristics of the studied sample, including cardiovascular risk factors.
| Normal glucose (n=323,248) | IFG (n=38,703) | Undiagnosed diabetes (n=4679) | Type 2 diabetes (n=4252) | Type 1 diabetes (n=1115) | |
|---|---|---|---|---|---|
| Raw prevalence, % | 86.9 (86.8–87.0) | 10.4 (10.3–10.5) | 1.3 (1.2–1.3) | 1.1 (1.1–1.2) | 0.3 (0.3–0.3) |
| Gender: males, % | 70.0 (69.8–70.2) | 87.4 (87.1–87.7)* | 92.9 (92.2–93.6)* | 90.4 (89.5–91.3)* | 82.2 (80.0–84.4)* |
| Age: years, mean | 35.7 (35.7–35.7) | 43.4 (43.3–43.5)* | 48.5 (48.2–48.8)* | 52.0 (51.7–52.3)* | 38.5 (37.8–39.2)* |
| BMI: kg/m2, mean | 25.6 (25.6–25.6) | 28.0 (28.0–28.0)* | 30.0 (29.9–30.2)* | 29.6 (29.5–29.7)* | 26.1 (25.8–26.3)* |
| Underweight, % | 1.8 (1.8–1.8) | 0.5 (0.4–0.6)* | 0.5 (0.3–0.7)* | 0.2 (0.1–0.3)* | 0.8 (0.3–1.3)* |
| Normal weight, % | 46.9 (46.7–47.1) | 24.7 (24.3–25.1)* | 13.4 (12.4–14.4)* | 13.1 (12.1–14.1)* | 46.1 (43.2–49.0) |
| Overweight, % | 37.4 (37.2–37.6) | 46.1 (45.6–46.6)* | 39.2 (37.8–40.6)* | 44.0 (42.5–45.5)* | 35.3 (32.5–38.1) |
| Obesity, % | 14.0 (13.9–14.1) | 28.7 (28.2–29.2)* | 47.0 (45.6–48.4)* | 42.7 (41.2–44.2)* | 17.8 (15.6–20.0)* |
| FPG, mmol/l, mean | 4.6 (4.6–4.6) | 5.9 (5.9–5.9)* | 9.1 (9.0–9.2)* | 9.0 (8.9–9.1)* | 9.8 (9.5–10.1)* |
| Hypertension, % | 18.4 (18.3–18.5) | 40.5 (40.0–41.0)* | 59.7 (58.2–61.2)* | 65.5 (64.0–67.0)* | 35.9 (32.9–39.0)* |
| Dyslipidemia, % | 56.3 (56.1–56.5) | 75.5 (75.1–75.9)* | 84.5 (83.4–85.6)* | 80.5 (79.3–81.7)* | 61.2 (58.1–64.2)* |
| High total cholesterol (≥5.17mmol/l, %) | 42.3 (42.1–42.5) | 61.3 (60.8–61.8)* | 68.7 (67.4–70.0)* | 52.1 (50.6–53.6)* | 40.3 (37.4–43.3) |
| High LDL cholesterol (≥3.36mmol/l, %) | 33.0 (32.8–33.2) | 48.4 (47.9–48.9)* | 51.2 (49.7–52.7)* | 37.6 (36.1–39.1)* | 28.5 (25.8–31.3) |
| Low HDL cholesterol (<1.03mmol/l, %) | 6.5 (6.4–6.6) | 6.4 (6.1–6.7) | 11.0 (10.1–11.9)* | 13.4 (12.4–14.5)* | 8.2 (6.5–9.8) |
| High triglycerides (≥2.26mmol/l, %) | 7.5 (7.4–7.6) | 16.7 (16.3–17.1)* | 35.8 (34.4–37.2)* | 24.6 (23.3–25.9)* | 12.3 (10.3–14.3)* |
| History of CVD, % | 0.4 (0.4–0.4) | 1.2 (1.1–1.3)* | 1.8 (1.4–2.2)* | 4.0 (3.4–4.6)* | 2.0 (1.2–2.8)* |
| Current smoker, % | 46.4 (46.2–46.6) | 41.9 (41.4–42.4)* | 48.0 (46.6–49.4) | 41.7 (40.2–43.2)* | 50.4 (47.4–53.3)* |
*p<0.05 vs normal glucose.
Values are either means (for age, BMI and glycemia) or percentages. Values in paretheses are 95% CI. FPG: fasting plasma glucose, IFG: impaired fasting glycemia or fasting plasma glucose level ≥5.6 but <6.9mmol/l, CVD: cardiovascular disease, low weight: BMI <18.5kg/m2, normal weight: BMI=18.5–24.9kg/m2, overweight: BMI=25–29.9kg/m2, obesity: BMI ≥30kg/m2, hypertension: systolic blood pressure ≥140mmHg and/or diastolic blood pressure ≥90mmHg, or on antihypertensive medication.
The results of the present cross-sectional study show that prevalence rates of impaired fasting glucose, type 1 and 2 diabetes by occupational categories in a nationwide sample of Spanish working population were greater among blue-collar than among white-collar workers especially at older ages, and UKDM and KDM2 were more prevalent among men than among women. Lower socio-economic status and differences in diet and leisure time physical activities could help explain the higher prevalence of IFG and diabetes among blue-collar compared with white-collar workers.18 Many other factors may also influence the relationship between type of occupation and diabetes. For example, occupational imbalances among American whites were lower than in this study, and we previously found that the prevalence of metabolic syndrome was higher in blue-collar than in white-collar workers only among females.6
In this sample of active workers, the raw prevalence of IFG (10.4%) was higher than the overall mean Spanish estimate of IFG prevalence (3.4%),3 and age- and sex-adjusted mean prevalences of UKDM and KDM2 were lower (2.0% and 2.4%, respectively) than the corresponding population age- and sex-adjusted mean estimates in Spain (6.0% and 7.8%, respectively).3
Higher prevalences of IFG and diabetes in men than in women have been also described in other studies.3,7 These studies have shown that these differences decline beyond the retirement age. Specific factors relating to working women, such as younger age or a better cultural or socio-economic background than those of working men, might contribute to this sex imbalance.18
To explain these differences, we can propose at least three factors. One is the relatively low mean age of the present sample. The reduction in the differential between type 2 diabetes prevalences in the sample of this study and the general Spanish population after adjusting for age goes some way to support this hypothesis. Second, the socio-economic status of our sample may be higher than that of the general population, in which the rate of unemployment is 8.6%.19 Marginal groups and individuals with adverse social factors, who may be at increased risk for diabetes,18,20 are underrepresented in the working population. Conversely, when estimates of prevalence are made using health system facilities, a selection bias may arise in favor of unemployed and older individuals. These facts may have epidemiological implications because the working population might yield prevalence estimates somewhat different from those of population-based studies, as suggested by prior reports from the ICARIA project5 and our findings. Third, design limitations may play a role. Abnormal FPG levels were not confirmed in repeated analyses, and there is no certainty that all participants respected the fasting periods. In this study as in others,20 only fasting glucose was used in defining the diagnosis of diabetes, while in the Spanish reference study oral glucose tolerance test was performed in more than 60% of the participants.3 For the diagnosis of diabetes and IFG we have used the ADA criteria,14 as performed in previous ICARIA studies.5–7
The ratio of UKDM to KDM2 in this study was greater than 1, higher than in other studies.21,22 Moreover, overweight/obesity, hypertension and dyslipidemia were more frequent in individuals with IFG, KDM2, and, notably, with UKDM, than in those with normal fasting glycemia. On the pragmatic side, given the suitability of IFG for screening purposes, this study suggests that including simple glycemic measures within the context of routine medical check-ups of active workers may constitute a suitable and straightforward approach to identifying a large proportion of candidate individuals for subsequent screening and prevention interventions.23
Such an approach would extend glycemic testing to a population who may otherwise be missed by clinic-based screening owing to their relatively infrequent contact with the healthcare system.24 Testing apparently unaffected individuals at increased risk of having diabetes when these individuals attend for health care for other reasons (sometimes called ‘opportunistic screening’) may be justified provided (1) the reasons for testing are adequately explained to the individual (2) the health system has the capacity for the clinical management of those who screen positive (3) methods with adequate sensitivity and specificity are available (4) the psycho-social needs of those who screen positive and those who screen negative can be met and (5) the health system can implement effective preventive strategies for those confirmed to be at high risk for the development of diabetes. Given the dynamic nature of this topic, policies for screening for type 2 diabetes must be reviewed from time to time as new evidence accumulates but in the meantime future research is needed to answer this question and probably our cohort study could give any preventive key clue.
In our study, the prevalence of other cardiovascular risk factors, including obesity, hypertension, increased concentrations of LDL-C, decreased concentrations of HDL-C, and increased triglyceride concentrations, in subjects with KDM2, UKDM2 or IFG was higher than in subjects with normal glucose control. The United Kingdom Prospective Diabetes Study demonstrated that most of these factors, together with diabetes and smoking, are associated with an increased risk of coronary heart disease.25 Multifactorial interventions that target multiple risk factors in subjects with type 2 diabetes may substantially decrease the cardiovascular risk.26 Therefore, the occupational setting seems to be appropriate for detecting individuals at risk of cardiovascular events and, together with primary care health professionals, for implementing multifactorial interventions aimed at reducing this risk.
Among the study limitations, we should not forget that the working population is not totally representative of the general population as we have previously discussed; a majority of the study group were men; and repeated glycemic measurements were not available to confirm IFG and UKDM states. In addition, our study was based on information collected during routine medical check-ups, which is limited with respect to certain research objectives. For example, in this study we lacked information on, or the information was not sufficiently complete for, ethnicity, waist circumference, physical activity, dietary habits and a family history of specific diseases (e.g. cardiovascular disease, diabetes). Future studies in the working population should include this information. Moreover, measuring waist circumference and including simple questions on other risk factors, such as those included in the Finnish Diabetes Risk Score (FINDRISC), in the routine medical check-up are highly recommended for both investigative and preventive purposes. Among the strengths, the large sample size of our study has permitted us to provide current and reliable estimates of the prevalence of type 1 diabetes, which are scarce in the literature. However, only workers without sick leave (active workers) attend these medical check-ups and this may be a limiting factor to extrapolate to the whole working population. Thus, a selection bias in the sense of that described as the “healthy worker effect” cannot be discarded.23 If such selection bias was present an underestimation of prevalence rates should be expected. Nevertheless, the study allowed us to increase our knowledge about the majority collective of workers (those without a current illness which is needed for sickness absence) with the highest potential for prevention. On the contrary, the implications of healthy work bias for the differences between occupational groups are less evident, as the selection bias is supposed to affect both groups to the same extent.
In summary, this study contributes to the current knowledge of the prevalence of diabetes and prediabetes in Spain. It shows that the working population has a high prevalence of IFG and lower prevalence of diabetes than the general population and it characterizes the risk of diabetes with increasing age. Glycemic testing during routine medical check-ups could be a useful tool to uncover IFG and previously undiagnosed diabetes.27 Such efforts should pay particular attention to groups at highest risk of these conditions, namely men, blue-collar workers and those with cardiovascular risk factors.
Conflicts of interestAlbert Goday, Eva Calvo, Martha Cabrera and María Teresa García-Margallo declare no competing interests. Luis Alberto Vázquez and Jesús Reviriego are full time employees of Eli Lilly and Company.
The authors thank all the ICARIA Study Group (full list in Sánchez-Chaparro et al.5). We thank Dr. Jesús Villoria from Medicxact who provided medical writing services on behalf of Lilly Spain.