A pituitary abscess is a rare but serious intrasellar infection. It was first described by Simonds in 1914 and since then, only about 100 cases have been reported in the English speaking literature.1,2 Most patients develop symptoms and signs of meningitis or pituitary neoplasm. Indeed, the predominant clinical features of pituitary abscesses resemble those of pituitary adenomas and they are usually accompanied by either endocrinological disturbances or symptoms related to a mass effect.
Syndrome of inadequate antidiuretic hormone secretion (SIADH) is not an uncommon complaint in association with neurological disorders, although very few cases of SIADH have been reported in association with a pituitary mass. Here, we describe the unusual case of a patient with a pituitary abscess that manifested severe hyponatremia, with no signs or symptoms of local or systemic infection.
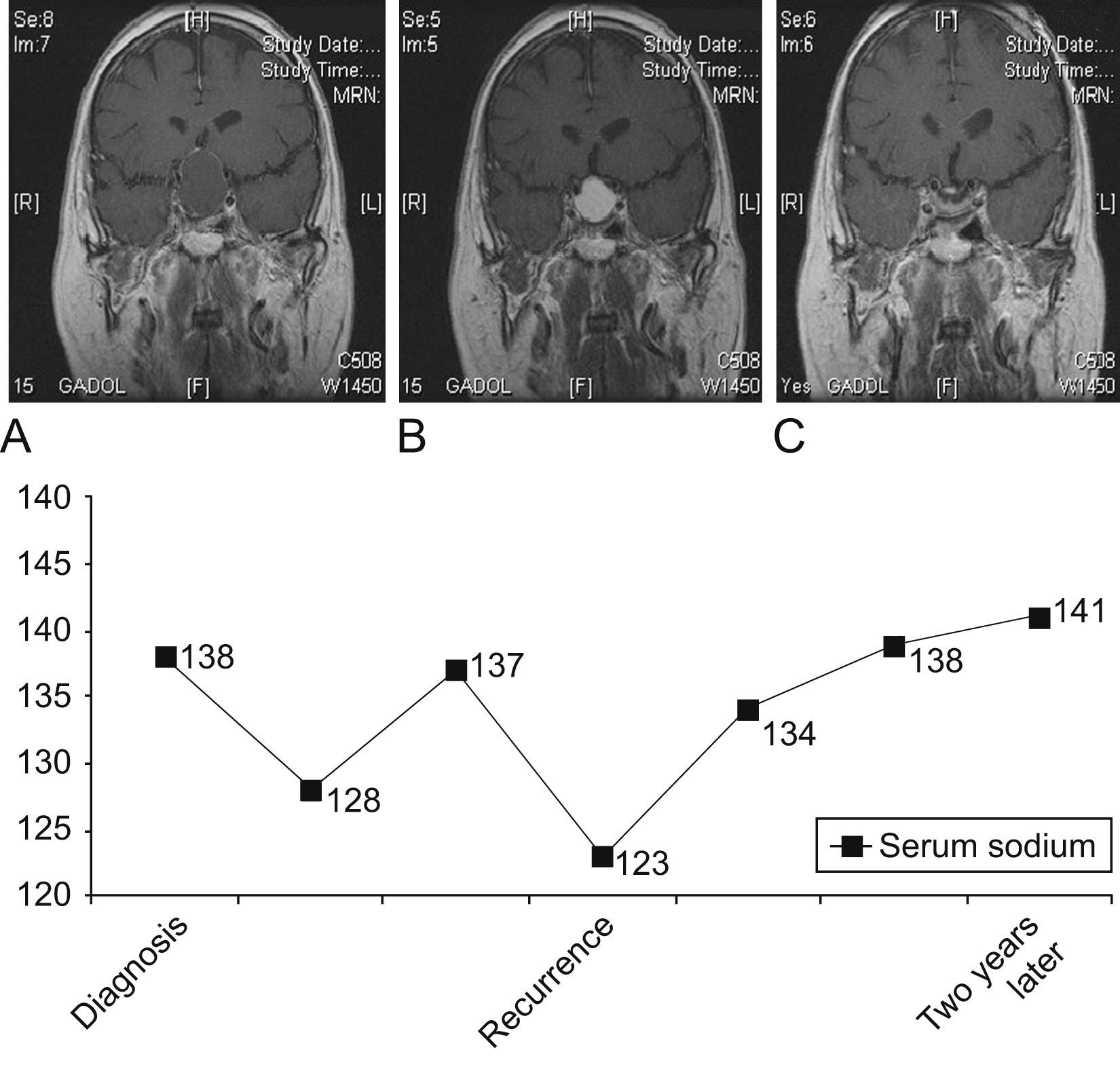
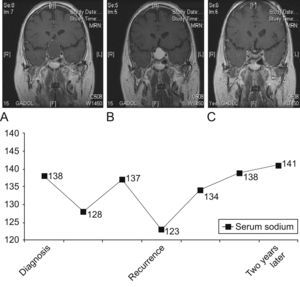
Case report: A 53 year-old man was admitted to our hospital complaining of extreme weakness, right frontal headache and photophobia. He also complained of having suffered recurrent headaches, anorexia, asthenia, bradypsychia and erectile dysfunction over the previous months. For the past 5 years he had been following treatment with glibenclamide and statins for type 2 diabetes and hypercholesterolemia, respectively, and he had achieved good glycaemic control. When examined clinically he was not thirsty and showed no signs of oedema or dehydration. He presented signs of hypopituitarism, with dry skin, scant axillary and pubic hair, and small and soft testes. His temperature was 36.1°C and he showed no signs or symptoms of local or systemic infection. However, bilateral temporal quadrantanopsia was found on ophthalmologic examination and in biochemical assays he had a serum sodium concentration of 128mEq/L and urinary sodium of 45mEq/L. Endocrine tests at admission revealed the following levels in the serum: cortisol, 1.6μg/dL; prolactin (PRL), 0.6ng/dL; follitropin (FSH), 0.16mU/mL; thyrotropin (TSH), 0.45uU/mL; and free thyroxine (FT4), 0.40ng/mL. Magnetic resonance imaging (MRI) of the pituitary identified a 3cm intrasellar mass that extended to both cavernous sinuses and to the optic chiasm, and it was of low-intensity in T1 weighted sequences and high-intensity in T2 weighting (Figure 1A). As a result, a pituitary adenoma was diagnosed. Mild hyponatremia persisted after replacement therapy with hydrocortisone and levothyroxine, and the patients’ fluid intake needed to be restricted until he underwent transsphenoidal surgery (Figure 1). Histopathological examination of the resected tissue revealed a necrotic material from which aerobic and anaerobic cultures were negative. After surgery, the patient recovered from the ophtalmoplegia but his hypopituitarism persisted and as such, replacement therapy was continued. Two months later, the patient again complained of severe headache, nausea and decreased visual acuity. A cranial MRI showed a 2.5cm heterogeneous intrasellar mass that was hypointense on T1 and hyperintense on T2 weighting (Figure 1B). Initial laboratory studies while on treatment with 60mg/day hydrocortisone and 100μg/day thyroxine revealed serum sodium concentrations of 123mEq/L, glucose concentrations of 151mg/dL, potassium concentrations of 4.2mEq/L, and a plasma osmolality of 265mOsm/Kg. Urine sodium excretion was 80mEq/L and his urine osmolality was 310mOsm/kg. Inappropriate antidiuresis secondary to pituitary lesion was diagnosed and daily fluid intake was restricted to 1500ml. The patients’ serum sodium concentrations gradually normalized within 3 days and with restricted fluid intake they remained stable thereafter. He then underwent a second transsphenoidal intervention to remove the pituitary mass and the pathological diagnosis was of a non-specific inflammatory reaction and necrotic material. Aerobic and anaerobic cultures were again negative. A diagnosis of recurrent pituitary abscess was made and the patient was treated intravenously with ceftriaxone and metronidazol. After surgery, the patient sodium balance normalized and he did not need any further restriction of fluids. After a follow-up of two years, the patient continues with persistent hypopituitarism that is controlled by replacement therapy and his water balance is normal. No pituitary lesions having been observed subsequently on MRI (Figure 1C).
Coronal T1-weighted magnetic resonance imaging (MRI) of the brain showing a low-intensity 3cm intrasellar lesion that extended into both the cavernous sinuses and the optic chiasm. The marginal ring-like contrast enhancement is indicative of an abscess capsule (Figure 1A). Coronal T1 MRI with gadolinium 2 months later showing a 2.5cm heterogeneous intrasellar mass that is hypointense on T1 weighting (Figure 1B), and a similar image after a two year follow-up period with no pituitary lesions (Figure 1C). Serum sodium concentrations are shown at the initial presentation, upon the recurrence of the pituitary abscess, and after a two year follow-up period (mEq/L).
Discussion: Pituitary abscess is a rare but serious intrasellar infection. The clinical features are usually similar to those of other pituitary masses, as they usually develop with either endocrinological disturbances and/or symptoms related to the mass effect. The most common clinical symptoms and signs at presentation are headache (87%), visual disturbances (68%), anterior pituitary dysfunction (30–50%), and occasional reports of diabetes insipidus.2 Only rarely are symptoms and/or signs of meningitis evident.2 Although imaging studies are sometimes useful to diagnose this condition, modern methods (CT and MRI) have only been able to preoperatively diagnose 24% of the cases reported.3,4 The typical MRI findings associated with pituitary abscesses are of a low-intense lesion in T1 weighted sequences and one of high-intensity in T2 sequences. While this profile suggests the accumulation of liquid, they may also be seen with necrotic adenomas. The most specific radiological finding is a marginal ring-like enhancement of contrast, suggesting the formation of an abscess capsule, as was evident in this patient. Except for cases where meningitis or adjacent sinus infection coexist, the origin of the infection is usually not found. Indeed, in most cases a microbiological diagnosis is not reached as more than 50 per cent of the cultures from the pituitary abscesses are reported to be sterile.2 This was indeed the case here, as the origin of the infection remained elusive and no growth was seen in the cultures.
To reach a diagnosis of SIADH patients must be clinically euvolemic, with normal adrenal and thyroid function.5 In our patient, hyponatremia and hypoosmolality was associated with elevated urinary osmolality, in the absence of any history of other disorders or drug ingestion related to SIADH.6 Although when initially diagnosed, adrenal and thyroid deficiencies coexisted, hyponatremia persisted after normalization of these deficiencies with replacement therapy. In addition, water restriction therapy normalized the patient serum sodium concentrations. In fact, the hypoosmolar hyponatremia was not only found at the initial presentation but also, it was associated with the recurrence of the pituitary abscess. During this evaluation period his thyroid and adrenal functions normalized.
Although SIADH is the most frequent cause of hyponatremia,2 there are no previous reports in the literature describing a relationship between SIADH and pituitary abscess. Very few cases of SIADH have been reported in association with pituitary masses,and only five cases have been reported in association with pituitary tumours.7–11 Although the mechanism underlying arginine vasopressin (AVP) secretion in these pituitary masses remains unknown, the intrasellar abscess in our patient pushed the pituitary stalk and posterior pituitary upwards, as shown in the MRI, and this dislocation could provoke the inappropriate secretion of AVP. The large pituitary mass and/or local infection may have provoked mechanical irritation of the AVP-producing cells in the supraoptic and paraventricular nuclei of the hypothalamus, a pathogenic mechanism that might have provoked SIADH in this patient7. Indeed, transsphenoidal removal of the abscess corrected the SIADH on both occasions. This rapid remission of SIADH in our patient when the abscess was removed on both occasions could reflect the influence of mechanical irritation of the AVP-producing cells in the hypothalamus and/or the pituitary.
The SIADH syndrome has also been described in 3 cases of symptomatic pituitary metastases.12 Ectopic AVP secretion by the primary tumour was confirmed in 1 case, whereas the underlying mechanism remained obscure in the other 2.13,14
We have come across a number of subjects with large pituitary tumours that occupy the sella turcica, yet severe hyponatremia independent of any dysfunction of pituitary adrenal axis is infrequent. This may be because the duration of hyponatremia is usually limited and mild, and diagnosing SIADH is sometimes difficult. In our case, the rapid recurrence of the clinical situation was the key to the diagnosis. The case presented here indicates that SIADH may be more frequently associated with underlying pituitary masses than expected, and masses such as pituitary abscesses should not be overlooked and they should be adequately dealt with.
This work was supported by grants to Mónica Marazuela from FISS 07/1119, and Fundación de la Mutua Madrileña.