Prevalence of malignancy among cytologies with atypia of undetermined significance (Bethesda category III) is variable, ranging from 5% to 37% in the different studies. There is thus no agreement on whether FNA should be repeated or surgery should be performed in these cases. The aim of this paper was to analyze the risk of malignancy in order to establish the most adequate clinical approach.
Material and methodsWe analyzed 431 thyroid cytologies performed at our hospital since the introduction of Bethesda System (from January 2011 to September 2014), of which 32 (7.1%) were labeled as category III. The second FNA, when performed, and the histological results after surgery were reviewed.
ResultsTwenty-three patients (82.1%) underwent thyroidectomy, while repeat FNA was performed in the remaining 5 patients (17.9%). Cytology was reported as benign (category ii) in 3 (60%) and as unsatisfactory (category i) in 2 (40%), who underwent thyroidectomy. Thirteen of the 25 (52%) surgical thyroid specimens showed no malignancy, while differentiated thyroid carcinomas were found in 12 (48%): papillary cancer in 10 (83.3%), follicular cancer in 1 (8.3%), and papillary cancer with follicular areas in 1 (8.3%). The risk of malignancy of Bethesda category III in our patients was 42.9–48.0%.
ConclusionWe recommend thyroidectomy for all patients with cytological Bethesda category III.
La atipia de significado incierto o lesión folicular de significado incierto (categoríaiii del sistema de Bethesda, 2007) tiene una prevalencia de malignidad variable en los distintos estudios (5–37%), y por tal motivo no existe en la actualidad un consenso sobre el manejo adecuado de este resultado: repetir PAAF o cirugía. El objetivo del siguiente trabajo es analizar el riesgo de malignidad en nuestro medio de dichos nódulos para determinar la actitud clínica más adecuada.
Material y métodosDesde la implantación del sistema Bethesda en el Hospital Xeral de Vigo (enero de 2011) hasta septiembre de 2014 se analizaron 431 citologías, de las cuales el 7,1% (32/430) fueron etiquetadas de categoría III.
Se revisó el resultado de la segunda citología cuando se repitió la PAAF y el resultado histológico posquirúrgico de los operados.
ResultadosEn 23 (82,1%) pacientes se indicó la realización de una tiroidectomía y en los 5 restantes (17,9%), la repetición de la PAAF. La citología resultó benigna (categoría II) en 3 de ellos (60%) e insatisfactoria (categoría i) en 2 (40%).
De los 25 pacientes tiroidectomizados, incluidos los 2 operados tras el resultado de la segunda PAAF, las piezas quirúrgicas de 13 (52%) fueron benignas y las de otros 12 (48%) demostraron un carcinoma diferenciado de tiroides: 10 (83,3%) con cáncer papilar de tiroides, uno (8,3%) con cáncer folicular de tiroides y uno (8,3%) con cáncer papilar con áreas de patrón folicular.
En nuestros pacientes el riesgo de malignidad de las citologías calificadas como categoría III está entre el 42,9 y el 48%.
ConclusiónRecomendamos que todos los pacientes con citologías categoría III de Bethesda se sometan a tiroidectomía.
The estimated annual incidence of thyroid nodule in Spain is 0.1%. The essential procedure for thyroid nodule assessment is fine-needle aspiration (FNA), which allows for identifying as benign 60–70% of nodules and avoids unnecessary surgery.1–3
For the procedure to be cost-effective, the cytological report should be associated to a specific recommendation for clinical management.2,4 The Bethesda System for Reporting Thyroid Cytopathology (2007) unifies the terminology and morphological criteria for thyroid nodules and standardizes FNA results into six categories.2 Category III (atypia of undetermined significance or follicular lesion of undetermined significance) includes cytologies with features that are insufficient to suspect malignancy but prevent their classification as benign. Although conceived as a last resource stratum, which should not represent more than 7% of all cytological reports,3,5 its prevalence has increased since this consensus was implemented6.
Prevalence of malignancy associated to this category varies according to different studies,4,5 which has caused controversy as to the adequate management of this cytological diagnosis. The Bethesda system, assuming a 5–15% prevalence of malignancy, recommends a repeat FNA in 2–3 months and surgery in the event of two consecutive results of atypia2; the American Thyroid Association (ATA) recommends surgery if Hürtle cells are found, and 18FDG-PET in all other cases7; the American Association of Clinical Endocrinologists, the Associazione Medici Endocrinologi, and the European Thyroid Association (AACE/AME/ETA) group Bethesda categories III and IV in the same level and recommend surgery in most cases.8
A recent report estimates a risk of malignancy ranging from 26% and 37% in category III cytologies, similar to that shown in category IV cytologies (15–30%). If this prevalence is confirmed, surgery would be advised in all cases.
The purpose of this study was to assess the risk of malignancy of thyroid nodules classified as category III according to the Bethesda system.
Patients and methodsA review was conducted for all thyroid cytologies performed at the Complexo Hospitalario Universitario de Vigo from January 2011 (when the Bethesda system was implemented at the hospital) to September 2014, selecting those labeled as atypia of undetermined significance (category III). Pending results of a procedure (repeat FNA or surgery) at the time of analysis were excluded.
Variables collected from each patient included age, sex, nodule size, ultrasonographic characteristics, histological confirmation, and waiting time until surgery or repeat FNA. Age, sex, and ultrasonographic criteria for malignancy (hypoechogenicity, microcalcifications, irregular margins, increased intranodal vascularization, and absent halo) were compared between benign lesions and thyroid carcinoma.
Results are given in the text as mean±standard deviation. Comparisons were made using SPSS version 17 statistical software, performing a Student's t test for quantitative variables and a Chi-square test for qualitative variables (significant p<0.05).
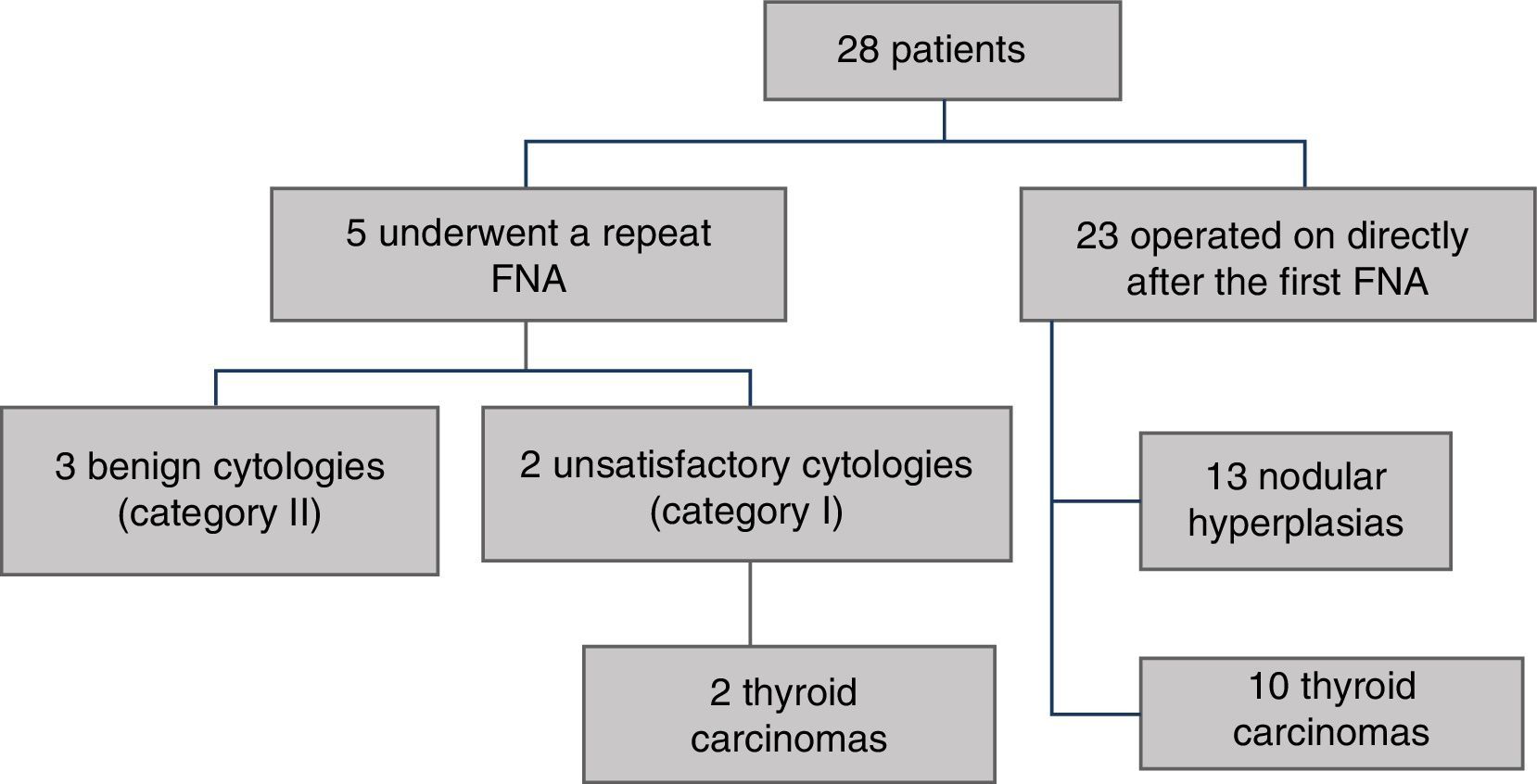
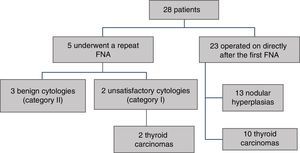
ResultsDuring the study period, the cytologies of 32 patients (7.1% of all FNAs performed) were classified as category III. At the time of this study, complete data were available for 28 of these patients (Fig. 1); mean age was 56±14 years, and 23 (82.1%) were female. Mean size of biopsied nodules was 2.4±1.1cm.
Total thyroidectomy was recommended for 82.1% (23/28) of patients, and was performed within 15±11.3 weeks.
Five of the 28 patients (17.9%) were performed a repeat FNA in an average time of 24.2±12.8 weeks. The result reported was benign (category II) in three patients (60%) and unsatisfactory in two patients (40%). These last two patients underwent total thyroidectomy, which showed the presence of papillary thyroid cancer in both.
The criteria used for performing repeat FNA or for referral for surgery were not recorded for most patients. For seven patients only, thyroidectomy was reported to be performed for compression symptoms, intrathoracic projection of goiter, or patient preference.
Age of patients with histologically benign lesions was not significantly different from that of patients in whom malignancy was shown (50.1±14.4 vs 58.5±16.9, p=0.20). Proportion of females was similar in both groups (84.6% vs 83.3%, p=0.93), as was the presence of ultrasonographic signs of malignancy (69.2% vs 66.7%, p=0.89).
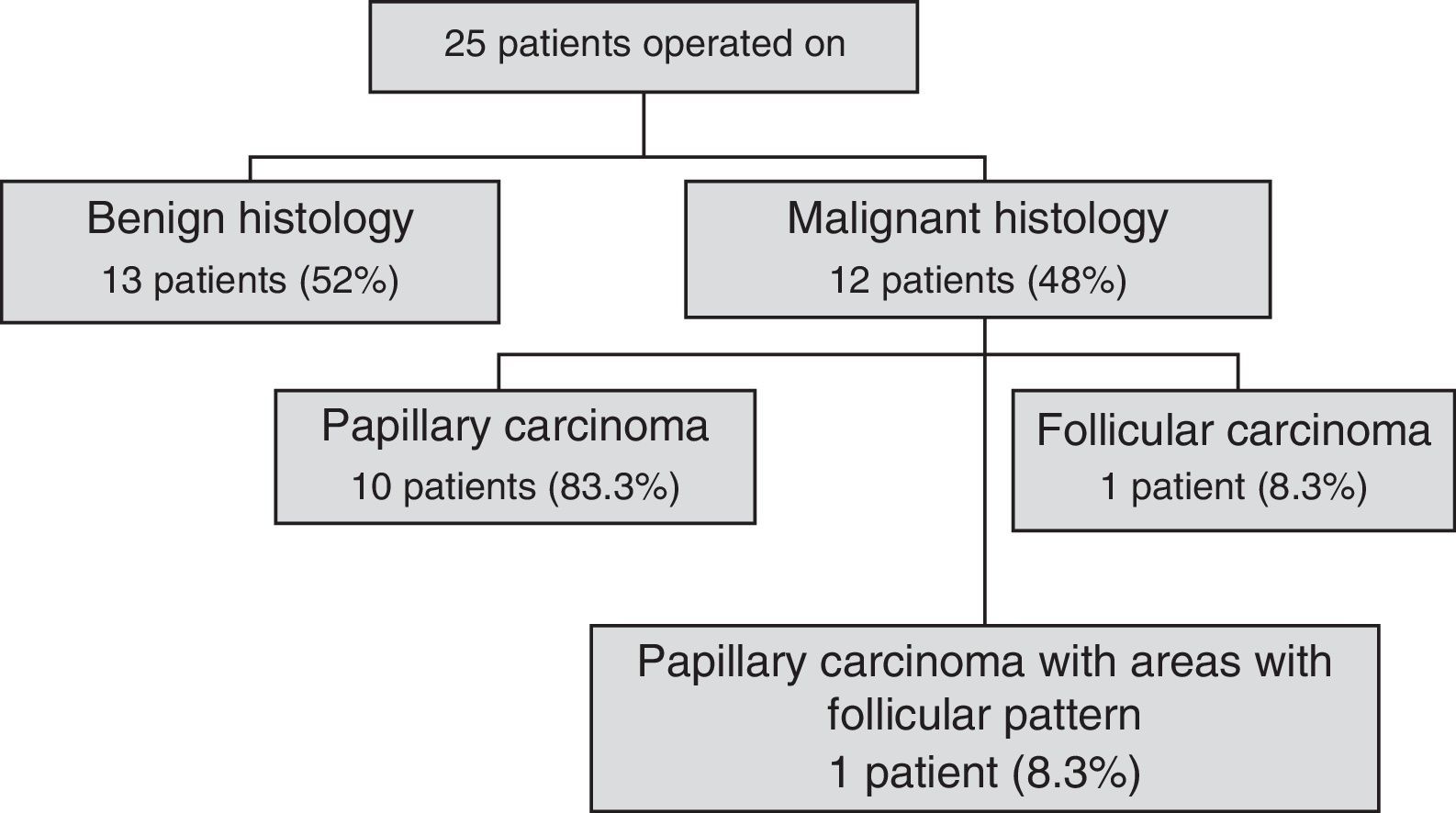
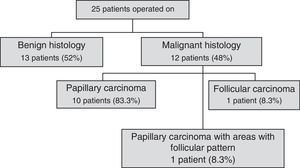
Pathological examination of surgical specimens from the 25 patients who underwent surgery (23 after the first FNA and two after the second FNA) showed the presence of thyroid carcinoma in 12 patients (Fig. 2) and absence of malignancy in the other 13 patients. Benign lesions were colloid goiter in 6 patients (46.1%), lymphocytic thyroiditis in 2 (15.4%), and nodular hyperplasia in 5 (38.5%). Thus, the lower and upper limits of the estimated risk of malignancy in our series were 42.9% (12/28) and 48% (12/25) respectively.
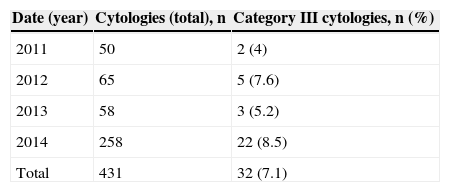
DiscussionA recent study6 showed a significant increase in reports of atypia of undetermined significance since the Bethesda criteria were devised. In our series, prevalence of such reports has increased with implementation of those criteria, but appears to be stable in the last three years. Mean prevalence is close to the proposed objective (Table 1).
The proportion of non-diagnostic cytologies at our hospital is 17.2±0.04%). Since 2010, we add to the standard puncture technique centrifugation of the material remaining in the needle by washing in a ThinPrep® solution. This has increased the diagnostic yield of our FNA procedure.9
All patients in our sample attended the same hospital of a city. This bias makes it likely that the estimated malignancy risk that makes surgery advisable in our patients is different in other settings. We encourage other groups to analyze such risk in their practice.
The high inter- and intra-observer variability of category III could be the reason for erroneous categorization of some thyroid cytologies which others would classify as carcinomas, thus overestimating the risk of malignancy. However, this diagnosis is evenly distributed among the pathologists in our healthcare area who examine thyroid samples, and none of them appears to be more prone to make this diagnosis.
Our standard clinical practice (thyroidectomy) in patients with atypia of undetermined significance differs from that recommended by the Bethesda system, but is supported by the high malignancy rates found.
We think that the main reason favoring one approach or the other has been prior experience of the clinician with the concerned nodules. No clinical or radiographic differences between benign and malignant lesions supporting one or the other type of management were found either. In addition, our waiting time for surgery was similar to that recommended for repeat puncture.
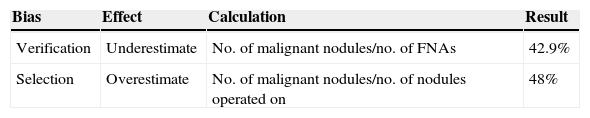
Estimation of malignancy risk is subject to two potential biases: verification bias—which underestimates risk—would occur if nodules in patients not undergoing surgery are assumed to be benign, while selection bias—which overestimates risk—would occur if only nodules subject to surgery are included in calculation6 (Table 2). We have calculated the lower and upper limits of the estimated risk of malignancy, and think that postoperative histological assessment of most cytologies decreases such biases. Even if the actual risk of malignancy corresponded to the lower limit of our calculation, it would be high enough as to advise thyroidectomy in all patients with cytologies reported as Bethesda category III.
ConclusionWe recommend thyroidectomy for all patients with a cytological report of Bethesda category III. Their high risk of malignancy advises against the recommendation of the Bethesda system.
FundingNo funding was received for this study.
Conflict of interestThe authors state that they have no conflicts of interest.
Please cite this article as: López Vázquez Y, Penín Álvarez M, San Miguel Fraile P, Barragáns Pérez M. Riesgo de malignidad de los nódulos tiroideos con atipia de significado incierto. Endocrinol Nutr. 2015;62:507–510.