To study the resolution improvement of endocrine diseases in primary care using communication and information technology (IT). Reduce number of inappropriate appointments to specialist care visits. Direct line establishment of communication between primary care and specialist care and provide quick and useful advices to GPs.
Materials and methodsThe GP establishes appointments for patients who need a visit with the specialist of endocrinology without physical presence. The queries are recorded in the medical share history of each patient. If a person requires a visit, the specialist care makes an appointment himself. A descriptive analysis was made based on virtual visits during 2008–2010, using the electronic medical history of patients from 6 GP centers. Adequacy of first visits (according to agreed protocols) between 2007 and 2009 was compared.
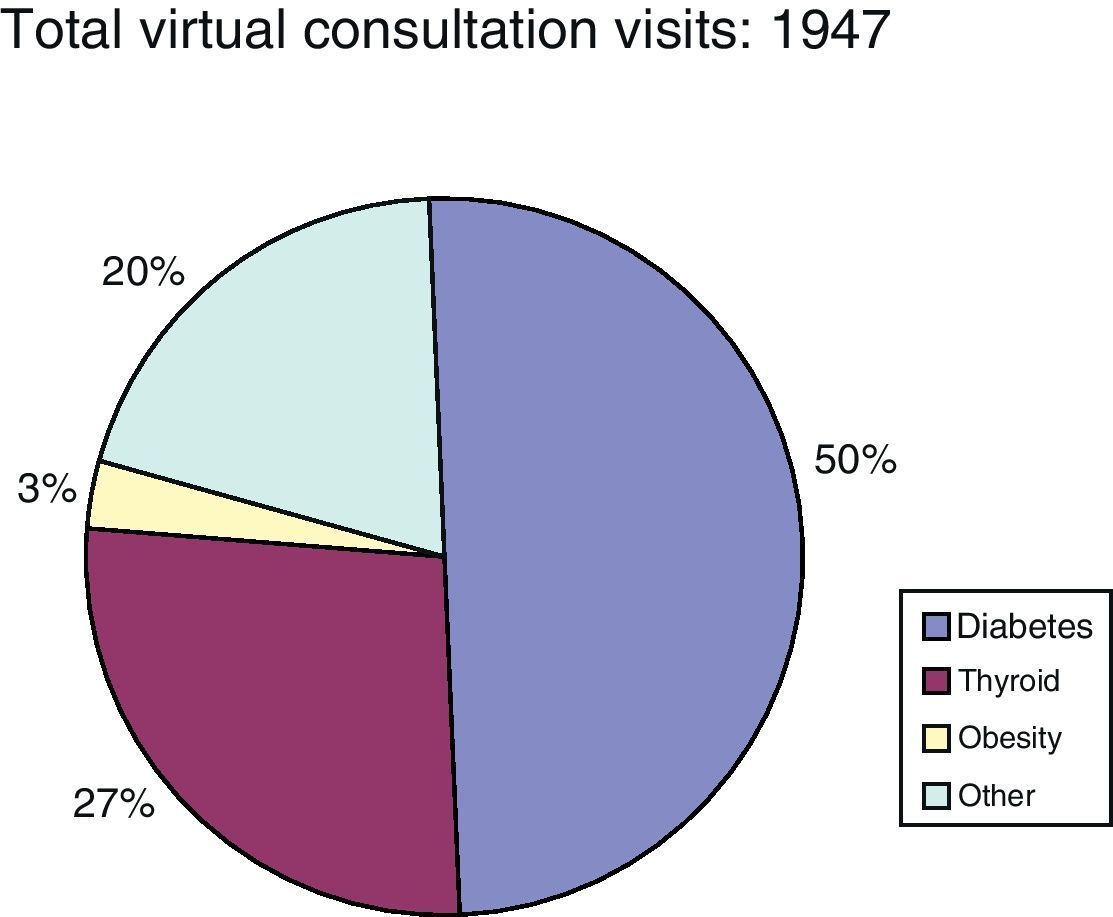
ResultsTotal number of online queries: 1705. Pathology: thyroid 35%, diabetes 50%, obesity 4% and others 11%. The most common virtual queries were the thyroid dysfunctions in 2008 and diabetes in 2010. Diabetes increased from 25.5% to 66%. In 2007 there were 25% of inappropriate first visit which were reduced to 10% in 2009. 88% of queries were resolved virtually.
ConclusionsThere was an increase in the capacity of case resolution in primary care with decrease of inappropriate first visits from primary care to specialist care. Teamwork between hospital and primary care was encouraged. The access of training in endocrine pathology among GP was improved.
Mejorar la resolución de las enfermedades endocrinológicas en Atención Primaria utilizando las nuevas tecnologías de la información (TI). Disminuir las visitas inadecuadas en Atención Especializada. Establecer un sistema de comunicación directo y asesorar a los médicos de familia de forma rápida y efectiva.
Material y métodosMediante una agenda especial, el médico de familia programa a los pacientes que quieren consultar al endocrinólogo sin presencia física. Las consultas son contestadas en la historia clínica compartida. Si el paciente consultado precisa una visita, el especialista lo cita en su agenda. Descripción de las consultas virtuales realizadas durante los años 2008, 2009 y 2010 utilizando la historia clínica informatizada por los médicos de familia de 6 centros. Comparación de la adecuación de las primeras visitas derivadas al especialista (según protocolos pactados) del año 2007 con el 2009.
ResultadosTotal de consultas virtuales: 1.705. Tipo de enfermedades: tiroides un 35%, diabetes un 50%, obesidad un 4% y otras un 11%. En el año 2008 las consultas más frecuentes eran enfermedad tiroidea y en el año 2010 diabetes, que pasó del 25,5 al 66%. En el año 2007 había un 25% de primeras visitas inadecuadas y en el año 2009 un 10%. El 88% de las consultas fueron resueltas virtualmente.
ConclusionesAumento de la resolución de los casos en Atención Primaria. Disminución de las primeras visitas derivadas inadecuadamente en Atención Especializada. Incentivación del trabajo en equipo entre Atención Primaria y Atención Especializada favoreciendo la continuidad asistencial. Asignación más racional de los recursos existentes. Mejora en el acceso a la formación en anatomía patológica endocrina entre los médicos de familia.
One of the most interesting changes which has occurred in Spain in recent years in the framework of health care reform has been the change in the relationship between specialized care (SC) and primary care (PC). Healthcare professionals are altering their working methods, and there is currently a trend to potentiate relations between the different professionals within healthcare areas. PC should not work without close support from SC, and a search for alternative means of communication is therefore mandatory.1,2
The health care reforms which began in Spain in the 1980s ended with SC reform in the 1990s. The integration of specialists working at primary care centers into the reference hospitals represented an advance that improved the coordination of the different care levels and, thus, patient access to these different levels.
Our hospital pioneered this model in Catalonia. In 1987, it launched a pilot project to integrate its medical specialties.3
Endocrinology is a medical specialty responsible for the care of highly prevalent diseases. Diabetes mellitus and the other chronic diseases associated with it (abdominal obesity, high blood pressure, and dyslipidemia) increase cardiovascular mortality. Thyroid diseases (hypothyroidism and hyperthyroidism, goiter, thyroid cancer, etc.) are also very common and cause frequent visits to endocrinologists. These are therefore suitable diseases for comprehensive care at all healthcare levels, the coordination of which is essential for an efficient approach.
Using the opportunity provided by new information technologies (ITs) and the computerization of clinical records, we set out to develop a new type of relationship between SC and PC using virtual consultation. The objectives were as follows:
- -
To improve the resolution of endocrine diseases in PC
- -
To decrease inadequate visits to SC
- -
To establish a direct communication system between PC and SC
- -
To provide rapid and effective advice to family physicians.
The geographic area where the study was conducted is the primary care subdivision (PCS) of Baix Llobregat Litoral, located in the province of Barcelona, only a few kilometers from the city of Barcelona. It is a suburban area, and its towns have populations ranging from 30,000 to 50,000 inhabitants. The total population covered is 180,000 inhabitants, and there are six healthcare centers (basic health area [BHA]) located in the towns of Begues, San Climent, Gavà, Catelldefels, and Viladecans. The populations assigned to these BHAs and their demographic characteristics are similar. SC is provided at Hospital de Viladecans by two endocrinologists.
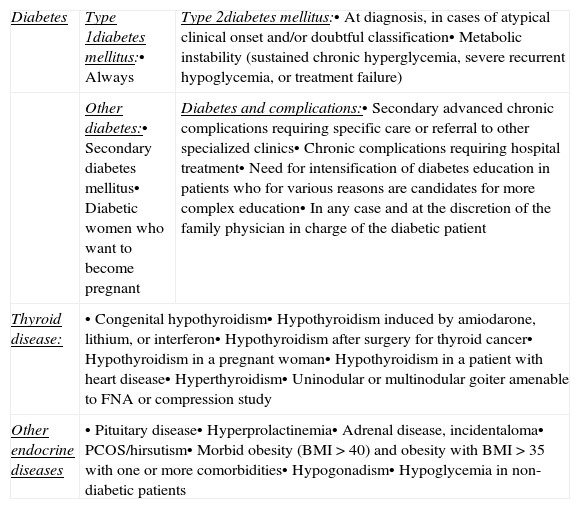
Because of the demand for SC consultation, an observational study was performed in 2007 for six months to verify the suitability of the first visits referred to our department. The diseases that would be referred to the endocrinologist had previously been agreed upon (Table 1).
Criteria for endocrinologist referral agreed with primary care.
| Diabetes | Type 1diabetes mellitus:• Always | Type 2diabetes mellitus:• At diagnosis, in cases of atypical clinical onset and/or doubtful classification• Metabolic instability (sustained chronic hyperglycemia, severe recurrent hypoglycemia, or treatment failure) |
| Other diabetes:• Secondary diabetes mellitus• Diabetic women who want to become pregnant | Diabetes and complications:• Secondary advanced chronic complications requiring specific care or referral to other specialized clinics• Chronic complications requiring hospital treatment• Need for intensification of diabetes education in patients who for various reasons are candidates for more complex education• In any case and at the discretion of the family physician in charge of the diabetic patient | |
| Thyroid disease: | • Congenital hypothyroidism• Hypothyroidism induced by amiodarone, lithium, or interferon• Hypothyroidism after surgery for thyroid cancer• Hypothyroidism in a pregnant woman• Hypothyroidism in a patient with heart disease• Hyperthyroidism• Uninodular or multinodular goiter amenable to FNA or compression study | |
| Other endocrine diseases | • Pituitary disease• Hyperprolactinemia• Adrenal disease, incidentaloma• PCOS/hirsutism• Morbid obesity (BMI>40) and obesity with BMI>35 with one or more comorbidities• Hypogonadism• Hypoglycemia in non-diabetic patients | |
Virtual consultation was started in 2008 using the following procedure: the specialist has a datebook in the software used by BHAs (e-CAP) where the family physician includes the patients who want to consult the endocrinologist without a personal visit. All consultations are answered in the clinical history, where the specialist's opinion is recorded. If the patient needs assessment in person, the specialist makes an appointment for him/her in his/her datebook. The family physician then makes another appointment for the patient in the telephone visit section to notify the patient. At the BHA of Castelldefels El Castell, by a decision agreed with center management, no family physician may make a direct referral to the endocrinologist without prior virtual consultation, and the specialist him/herself decides if the visit is needed.
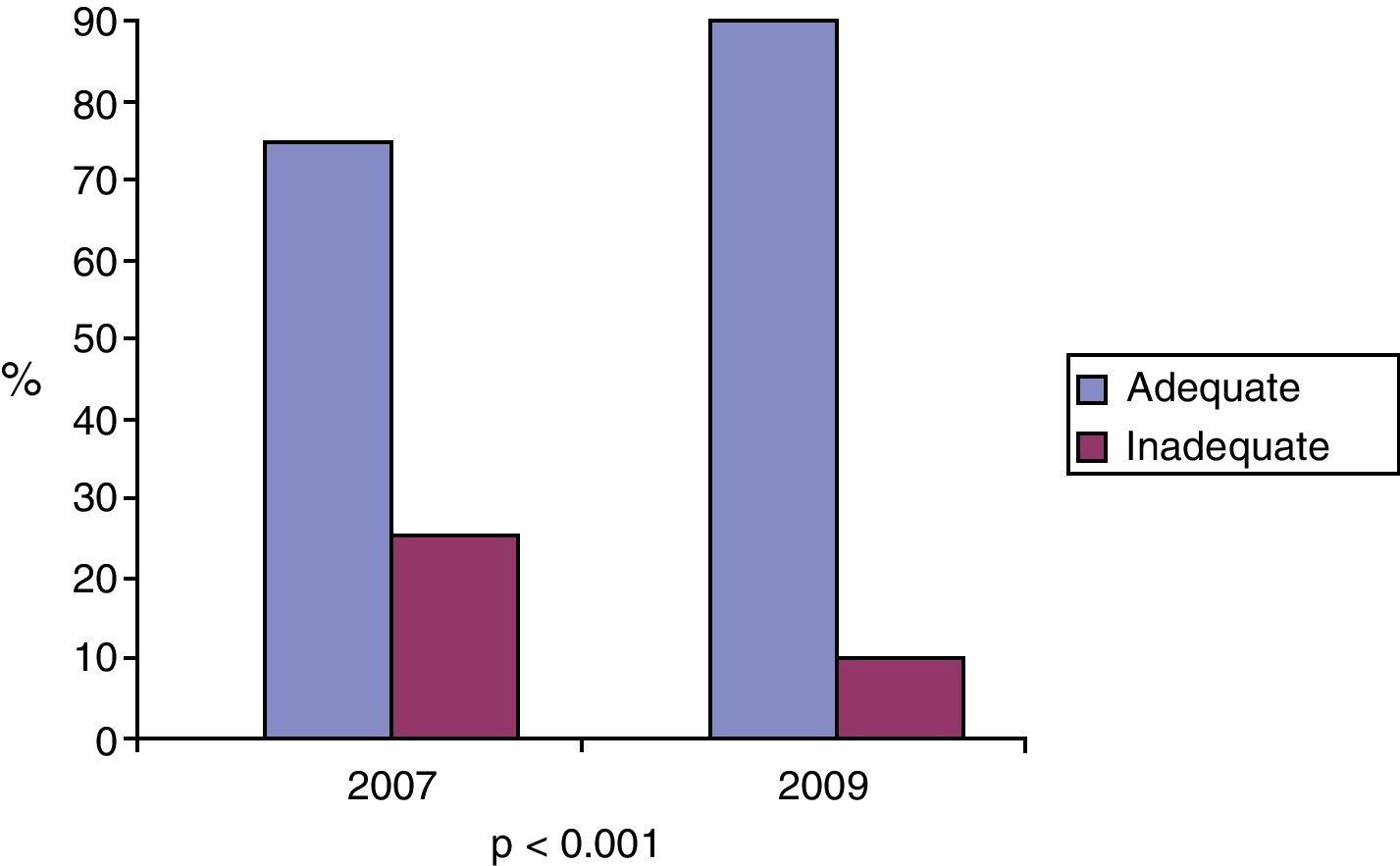
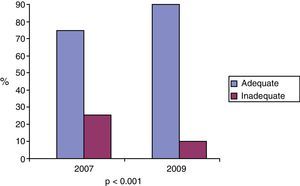
A comparison was made of the suitability of the first visits referred to endocrinology during a six months period in 2007 and the same six months of 2009, 1 year after the implementation of virtual consultation, and qualitative variables were compared using a Chi-square test.
A descriptive analysis of virtual consultations made during 2008, 2009, and 2010 was performed.
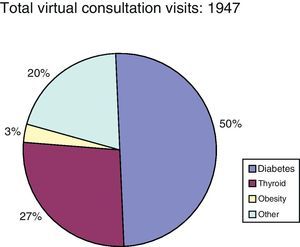
ResultsAmong the 1947 virtual consultations to SC made by PC in 2008, 2009, and 2010, 50% were for a disease related to diabetes, 27% for thyroid disease, 19.6% for endocrine disease (adrenal incidentaloma, hirsutism, hyperprolactinemia, etc.), and 3.6% for obesity (Fig. 1).
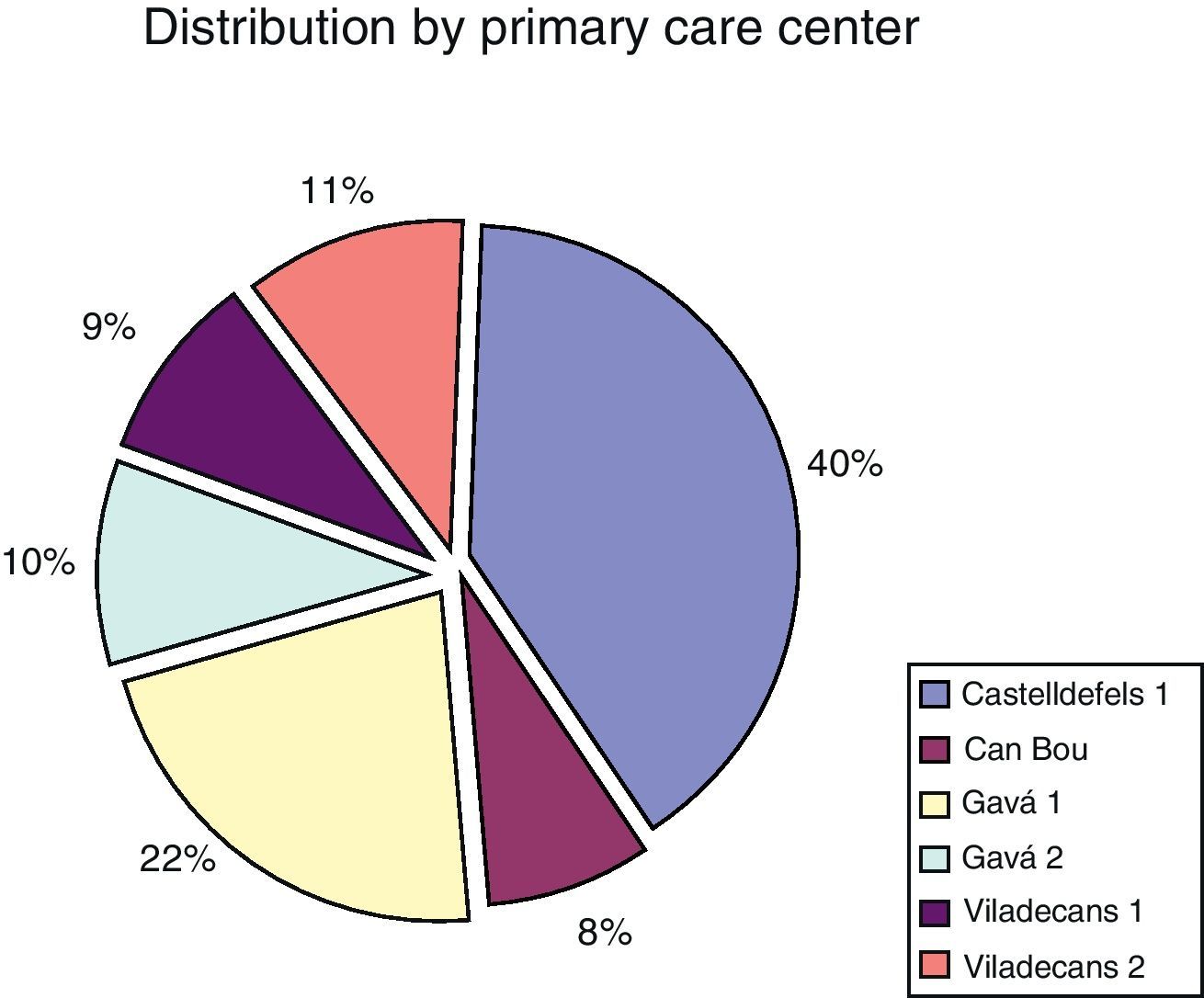
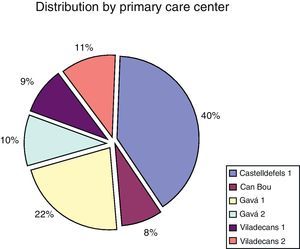
By origin (depending on BHA), 40% of virtual consultations were from the Castelldefels primary care center and 10% from each of the other centers, except for the Gavà center, with 20% of consultations (Fig. 2).
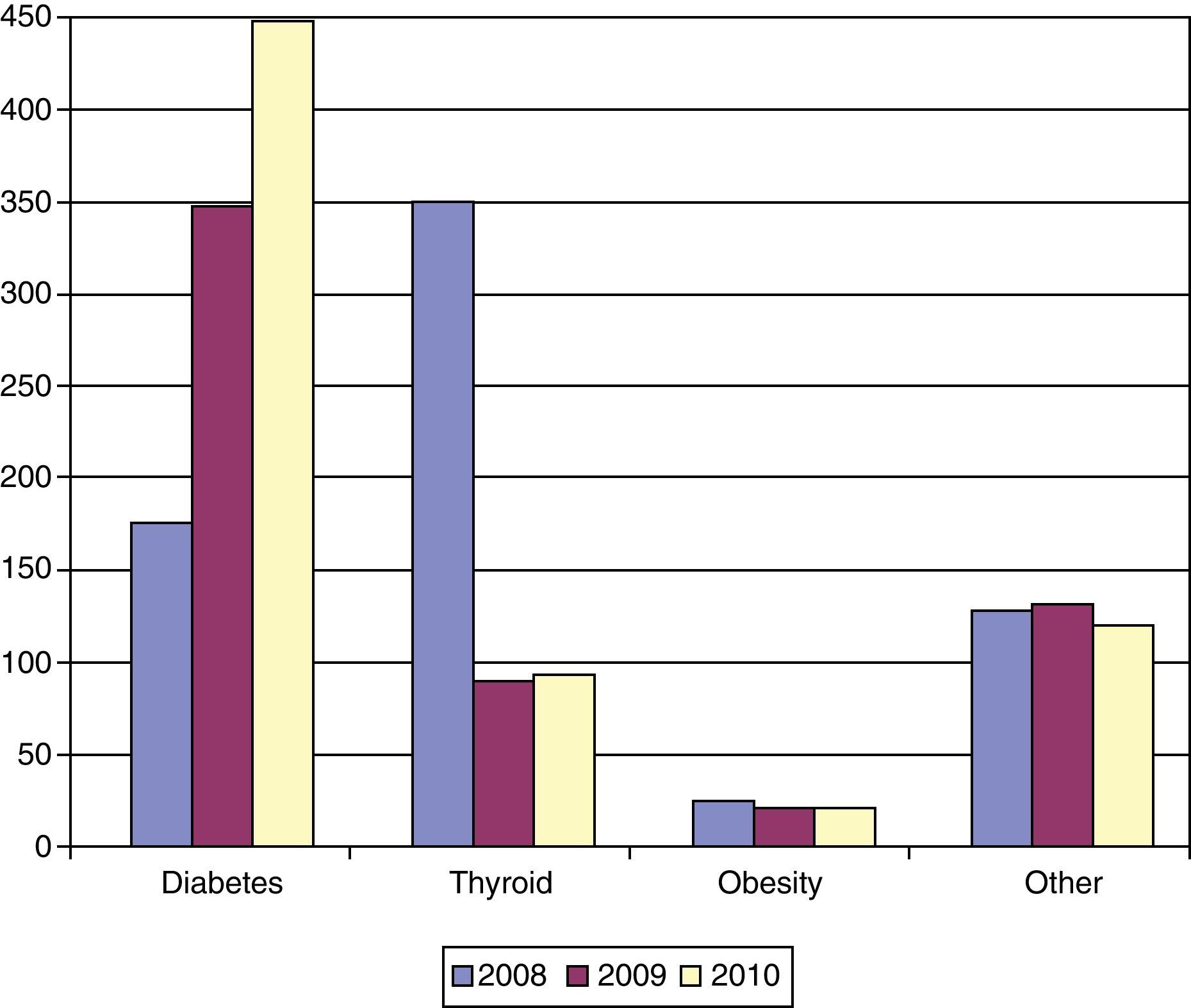
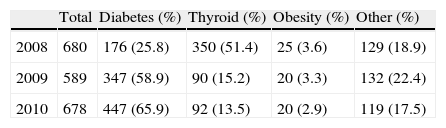
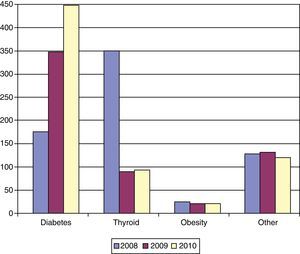
An analysis of the diseases leading to consultation in the 3 years showed a marked increase in consultations for diabetes (from 25.8% to 66%), a decrease in consultations for thyroid disease (from 51% to 13%), and stabilization for all other diseases (Table 2 and Fig. 3).
Consultations by type of disease in 2008, 2009, and 2010 in absolute numbers and percentages.
| Total | Diabetes (%) | Thyroid (%) | Obesity (%) | Other (%) | |
| 2008 | 680 | 176 (25.8) | 350 (51.4) | 25 (3.6) | 129 (18.9) |
| 2009 | 589 | 347 (58.9) | 90 (15.2) | 20 (3.3) | 132 (22.4) |
| 2010 | 678 | 447 (65.9) | 92 (13.5) | 20 (2.9) | 119 (17.5) |
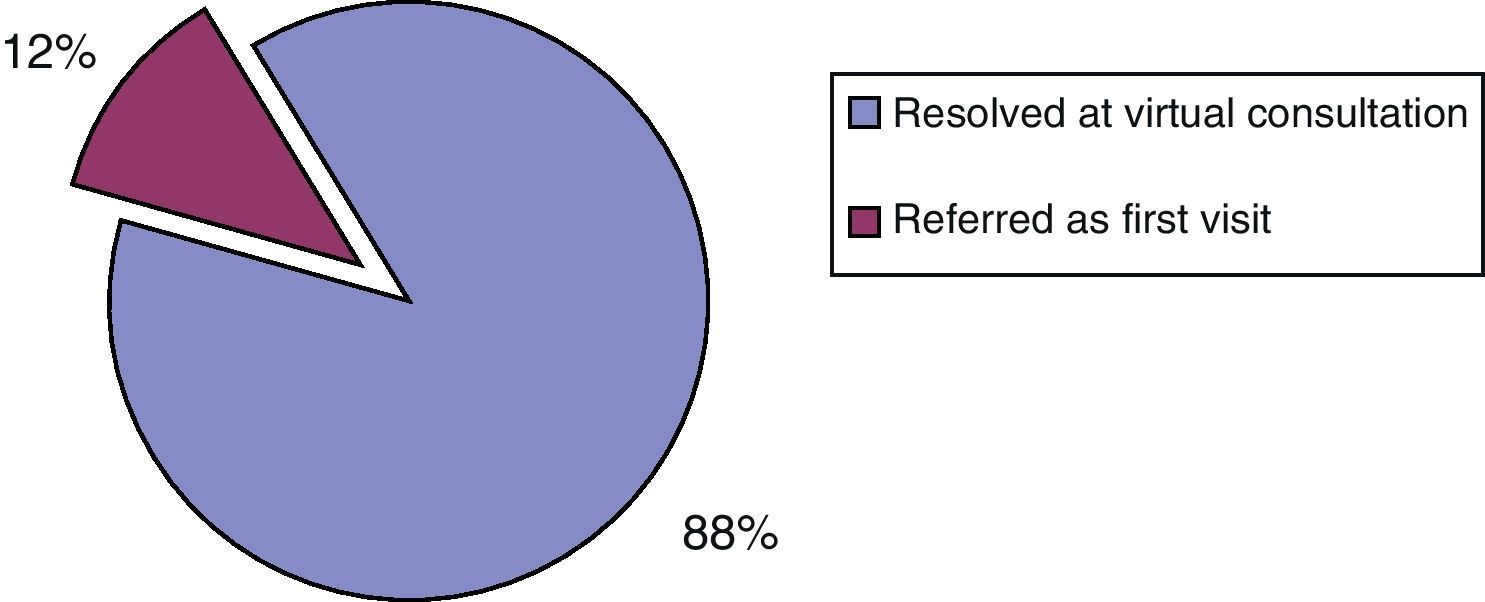
The results of the analysis of the suitability of the first visits referred to the endocrinologist were as follows: in 2007, 25% inadequate visits, according to previously agreed protocols, had been referred to SC, while in 2009, after the implementation of virtual consultation, inadequately referred visits had decreased to 10%. The difference was statistically significant (p<0.001) (Fig. 4).
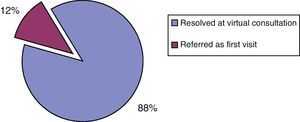
Of the total 1947 virtual consultations, 1713 (88%) were resolved, while a visit to the hospital was required in the remaining 234 (12%) (Fig. 5).
DiscussionDuring the past 14 years, several approaches have been used in our work setting in order to improve communication between PC and SC, including regular continuous training meetings with endocrinologists at healthcare centers. These meetings have included clinical sessions to discuss cases, joint preparation of diagnosis, monitoring, treatment, and referral protocols, and theoretical sessions to give information regarding the availability of new drugs or advances in endocrine diseases. Very special attention has been paid to protocols for defining which diseases were amenable to control and monitoring by family physicians and which should be referred to endocrinologists.
Despite these efforts, in 2007, because of the excessive waiting list for first visits to an endocrinologist, it was decided to analyze the reason and source of referral and whether or not it met the previously agreed referral protocols. The study showed that 25% of referrals were inadequate, what prompted us to search for a strategy to solve this problem.
Some work groups, such as the W. Ricart group in Girona, also aim at improvements in the coordination and integration of care levels and are currently analyzing their results.4
Based on experiences by other groups, in 2008 we started a program based on the virtual consultation system using shared clinical histories. There are reports on the use of telephone visit systems, electronic mail, mobile telephone messages,5,6 and other approaches related to new ICTs.5,7 To our knowledge, however, no publication has reported the results of a virtual consultation program between PC and SC such as the one discussed here. The use of a single computer system (using the same clinical histories) allows for these personal visits to be recorded as evaluable and measurable medical actions. In addition, when family physicians receive the answer, they are obliged to inform the patient of the specialist's advice. This increases their implication and also, indirectly, their understanding of this type of disease.
The significant decrease in first visits inadequately referred to the endocrinologist achieved is a good result. The 2007 analysis showed that 25% of first visits did not meet the referral protocols despite the fact that they had been agreed with family physicians and discussed in clinical sessions. In the 2009 analysis, only 10% of first visits were inadequate. The availability of virtual consultation has given to family physicians the possibility of a rapid and more efficient resolution of their diagnostic or treatment questions, thus avoiding many unnecessary referrals to a specialist and allowing for the more rational use of the available resources.
Virtual consultations for diabetes increased from 25.5% in 2008 to 66% in 2010. This may be due to multiple factors, but we think that it was due to the implementation in 2009 of the “care route for type 2 diabetes”.
In addition to being one of the most prevalent diseases in our specialty, diabetes is not only among the conditions requiring greater coordination and communication between care levels, but also a comprehensive multidisciplinary intervention that guarantees continued care.8–11 The “care routes” started in the PCS in cooperation with the hospital are defined as a comprehensive care process focused on the axes of training, coordination, and rapid and effective problem resolution. In diabetes, this has resulted in a greater involvement of the family physician in the care of patients with the disease, and the algorithm of the “route for type 2 diabetes” considers virtual consultation as an alternative resource to referral for clarifying doubtful diagnoses and treatments, and for resolving transient clinical decompensations.
In 2010, virtual consultation was already part of the routine work at our area, and resolved 88% of cases, thus increasing the resolution capacity of PC, as only 12% of cases reported required referral to a hospital for a personal visit to the endocrinologist.
To sum up, it may be stated that virtual consultation to the endocrinology department of the hospital increases problem resolution in PC, which in turn encourages team work between PC and SC and promotes continued care with a more rational assignment of the available resources. Moreover, it improves the access of family physicians to training in endocrine diseases and decreases the number of first visits inadequately referred to SC.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Oliva X, et al. Sistema de consultoría virtual entre la Atención Endocrinológica Especializada y la Atención Primaria. Endocrinol Nutr. 2013;60:4–9.