Inflammatory pseudotumor (IPT), also called plasma cell granuloma, is a rare benign lesion of uncertain origin.1 IPT most commonly affects the lungs, followed by the liver and spleen, although this lesion may occur in almost any location.2 The etiology of IPT remains unknown but is believed to be the result of chronic inflammation caused by long lasting aggression. This process can be asymptomatic2 or associated with a spectrum of nonspecific symptoms.
No imaging technique has been established as the standard for the diagnosis of IPT. However, there is some literature evidence on the advantage of 18F-fluorodeoxyglucose positron-emission tomography (18FDG-PET) in the diagnosis of this usually otherwise elusive lesion.
We present a 39-year-old man who presented to our center with a past history of intermittent fever (up to 39°C), chills, fatigue and generalized weakness associated with frequent episodes of diarrhea. He reported that over the past 9 months he had been admitted three times to his local hospital for evaluation. The main findings from these admissions were recurrent high erythrocyte sedimentation rate, elevated serum C-reactive protein levels and serum liver enzyme levels slightly over the reference range. Cell blood count was normal. Serologic tests for brucella, salmonella, Q fever, HIV, hepatitis B and C viruses were negative. Testing for syphilis, antibodies to toxoplasma (immunoglobulins IgG and IgM), varicella – zoster virus, and cytomegalovirus (CMV) antigen were also negative. The results of antibodies to coxsackie (IgM) and echovirus (IgM) were positive. Image studies including chest and abdominal computed tomography scan, whole-body magnetic resonance imaging (MRI) and abdominal ultrasound were normal with the exception of a 13.4-cm splenomegaly. The suspicion of an infectious process led to the recurrent use of blind therapy with broad-spectrum antibiotics that temporarily resolved his fevers and had an uneven effect on his generalized non-specific symptoms. The patient was repeatedly discharged with the diagnosis of fever of unknown origin (FUO) and no treatment was given.
Upon admission to our center, the patient reported recurrent fever but no other complaints. On physical examination his blood pressure was 120/85mm Hg. He appeared healthy and was apyretic. His neck was supple, without palpable thyroid abnormalities. Examination of the lymph nodes, heart, lungs, abdomen, and extremities was unremarkable.
At our center, the results of liver-function tests were normal; the albumin level was 4.2g per deciliter. The white-cell count was 9100 per cubic millimeter, with 81% neutrophils, 12% lymphocytes, 5% monocytes, and 1% eosinophils. The hematocrit was 40.4%, with a normal mean corpuscular volume. The platelet count was 389,000 per cubic millimeter. Peripheral blood red cells were normal. Anti-double stranded DNA antibody was negative.
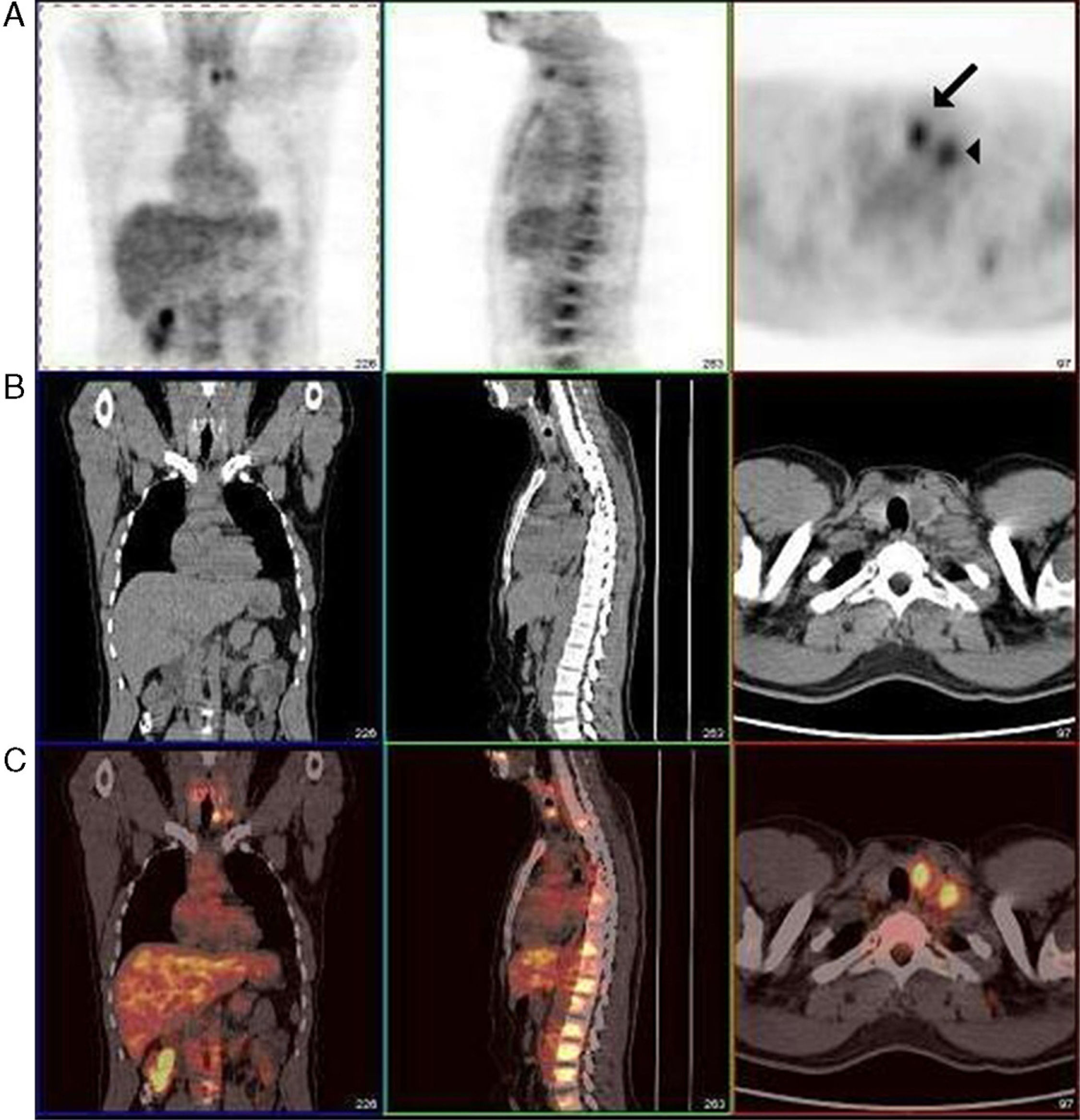
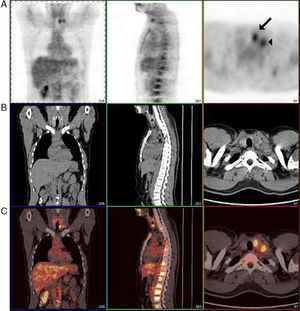
A whole-body CT scan revealed no structural alterations. As part of the diagnostic workup to determine the origin of his fever, the patient underwent whole-body 18F-FDG-PET. Imaging showed 18F-FDG avidity in a focal lesion measuring approximately 2-cm in his left thyroid lobe (SUVmax=4.1), consistent with a thyroid nodule. A second marked tracer uptake was individualized in area IV of his left neck (SUVmax=3.7), suggesting a normal lymph node (Fig. 1).
Positron-emission tomographic (PET) studies with 18F-fluorodeoxyglucose. Line A (left to right) coronal, saggital (neck, chest and upper abdomen) and transversal (at neck level) PET views. An increased tracer uptake is seen in the left thyroid lobe (SUVmax 4.1) and in a cervical left lymph node (SUVmax 3.7), indicated by an arrow (thyroid) and an arrow head (lymph node). Line B. (left to right) CT images from the same anatomical areas. Thyroid nodule is a 2-cm mass. Line C. Merged images of A and B. These lesions were eventually classified as papillary thyroid cancer and inflammatory pseudotumor.
These findings warranted a neck ultrasound-guided Fine Needle Aspiration (FNA), which showed three lesions: First, a hypoechogenic, hypervascular 2cm×2cm nodule with microcalcifications on the left thyroid lobe; second, a 0.4cm nodule with peripheral calcifications on the right thyroid lobe; and third, a 2.2cm cervical lymph node. The thyroid nodules had features consistent with malignancy. The two bigger lesions corresponded to FDG-PET positive lesions. FNA biopsy of the two thyroid nodules provided cytological evidence suggestive of papillary thyroid carcinoma (PTC) whereas lymph node cytological features displayed no abnormal features.
Total thyroidectomy with central and left compartment (including levels II–V) lymph node neck dissection were performed. Macroscopically there was a left solitary well-circumscribed nodule of 1.5cm in size, associated with a small nodule of 0.1cm in the right lobe. Microscopically, the typical features of PTC were observed. Five out of five central compartment lymph nodes were positive for metastasis of PTC whereas all 20 removed lymph nodes from areas II, III and V were negative. However, histologic examination of the largest lymph node (2.5cm) revealed a non-suspected lesion in which the normal architecture was partially effaced. It had a marked sclerosis/hyalinization of the lymph node parenchyma. In foci, the fibrotic bands were seen in flowing bundles with prominent concentric arrangement and a whorling/storiform pattern in places. Interspersed between the fibrotic bands was a polymorphic infiltrate composed of lymphocytes, plasma cells, eosinophils and plasmatic cells. Immunohistochemistry was performed using a standard avidin–biotin–peroxidase complex technique. Primary antibodies used included S-100 protein, epithelial membrane antigen, CD-1A, CD-21, CD-68 and lysozyme. Only CD-68 and lysozyme showed positive staining reaction of macrophages present diffusely in the lymph nodes. All these features were consistent with the diagnosis of IPT. This lymph node corresponded to the lesion with focal uptake in PET, where FNA was normal.
All clinical complaints, including the intermittent fevers disappeared after the removal of the IPT. After surgery, the patient underwent radioiodine treatment. Neither the thyroid carcinoma nor the IPT have reappeared after seven years of follow-up.
IPTs have been described in lymph nodes1,2 and thyroid glands,3,4 among other organs. To the best of our knowledge, this is the first case that describes an association between PTC and IPT. Although the etiology of IPT remains unknown, the case we describe supports the hypothesis that a long-term aggression,2 such as the presence of a carcinoma, may be the cause for the development of IPT. Nevertheless, we have no definitive evidence of this relationship.
The case we describe demonstrates several aspects of FDG-PET that make it an outstanding diagnostic tool. First, CT and MRI have traditionally disclosed cervical IPT. In the present case, the images provided by FDG-PET discovered not only an elusive cervical IPT, but an occult PTC as well. This coincidental finding has not been described previously. Second, in the case we present FDG-PET has been able to distinguish IPT from other pathologic lymphadenopathies, thus being much more specific than CT and MRI. Third, PTC is usually asymptomatic,5 and FDG-PET antedated the diagnosis. Fourth, evidence supporting the pre-eminent role of FDG-PET in the diagnosis of FUO is increasing steadily. In the present case FDG-PET revealed the origin of FUO after 9 months of burdensome testing by image and biochemical studies, including three hospital admissions. And finally, by localizing sites of active inflammation, FDG-PET may guide the selection of a biopsy site. As for the diagnosis of PTCs, although FDG-PET has replaced conventional nuclear medicine techniques at many other tumor sites, it still only has a complementary role in the assessment of this neoplasia. The risk of malignancy of thyroid incidentalomas detected by FDG-PET is around 15–40%, therefore it is an indication for Fine Needle Aspiration biopsy.
In summary, the case we report is especially original because FDG-PET was used to discover the cause of FUO: a previously elusive IPT. Therefore, we suggest that FDG-PET represents a key diagnostic tool in the differential diagnosis of FUO.