Adrenal cyst is an uncommon condition, but its incidence is increasing with the widespread use of imaging techniques. Preoperative diagnosis is difficult, and treatment is highly controversial.
We report the case of a 38-year-old male with an unremarkable history referred from the emergency room to the endocrinology outpatient clinic for a 5-cm adrenal mass. The patient complained of having had pain in the right hypochondrium for the previous three weeks. This pain was constant, radiating from the back, and was unrelated to food intake. The patient attended the emergency room because of pain persistence. Initial laboratory test results were normal, and a physical examination revealed pain in the right hypochondrium on deep palpation. Abdominal ultrasound was performed to rule out biliary disease. Ultrasound examination showed a 5.2cm×3.8cm thick-walled, cystic mass in the right adrenal gland (Fig. 1).
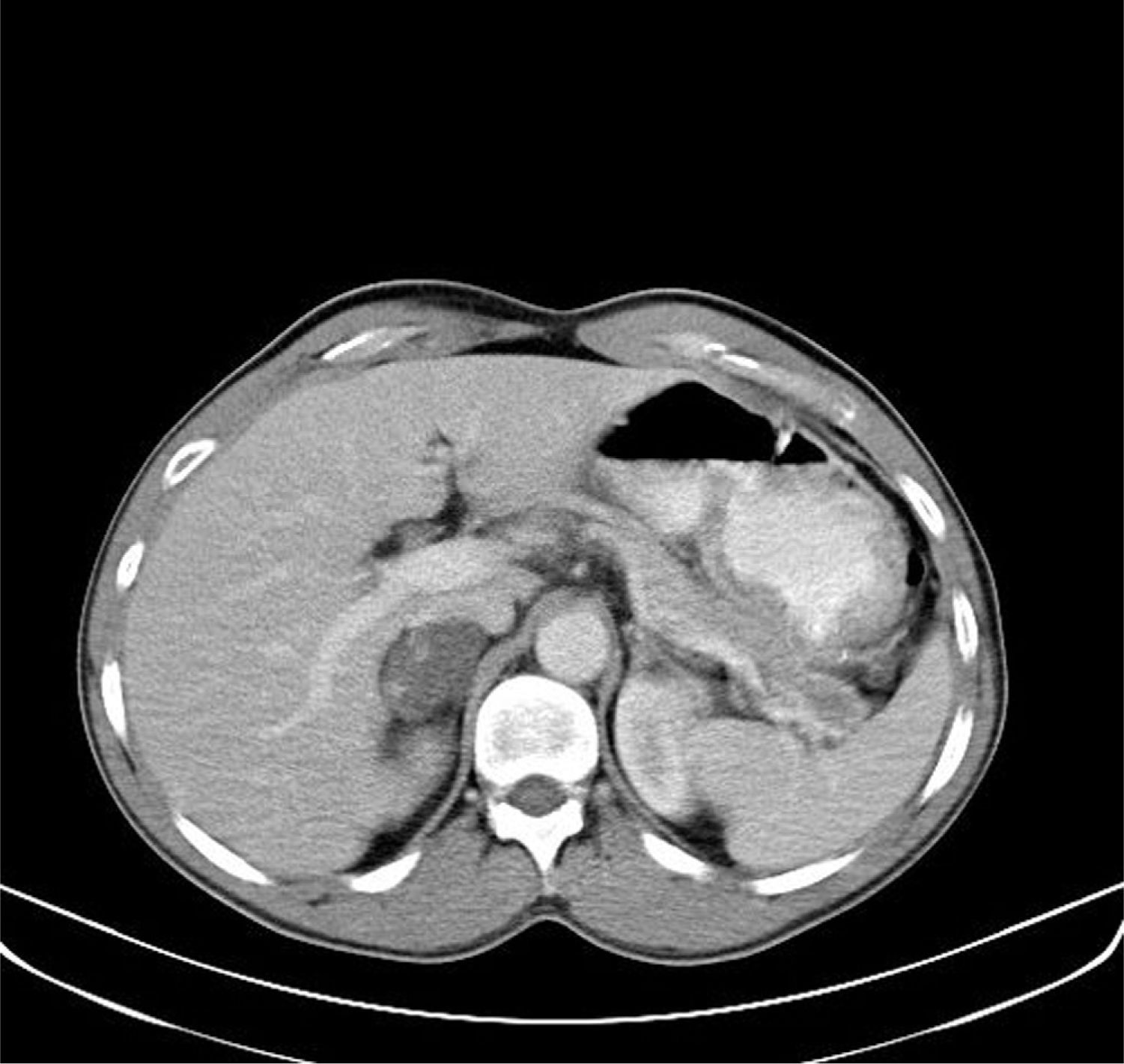
The patient reported no palpitations, headache, or weight changes. Lumbar pain was the only significant symptom. Weight was 68kg, and body mass index 21kg/m2. Blood pressure at the clinic was 130/75mmHg. No Cushingoid traits were found. Laboratory tests requested included catecholamine, metanephrine, vanillylmandelic acid, and 24-h urine cortisol levels. Test results included: norepinephrine 20.7μg/24h (12.1–85.5), epinephrine <3μg/24h (1.7–22.4), dopamine 215.9μg/24h (0–498), metanephrines 152μg/24h (0–341), normetanephrines 308μg/24h (0–444), and free urinary cortisol 70.7μg/24h, all of them within the normal range. The plasma cortisol level was 25.1μg/dL, dehydroepiandrosterone sulfate level 1.6μg/mL (0.9–4.3), and total testosterone level 8.52ng/mL. Suppression after nocturnal administration of dexamethasone 1mg (23h) was also performed, and a plasma cortisol level of 0.7μg/dL was found. A CT scan showed a high density cystic mass with 5-cm wall thickenings in the right adrenal gland showing an increased uptake (Fig. 2). Although this was a non-functioning lesion, surgery was decided upon because of tumor size and doubts concerning its etiology.
An uncomplicated right laparoscopic adrenalectomy was performed. A pathological study of the specimen revealed a 5cm×4cm×2cm mass, 21g in weight, with a smooth surface and mucinous content. Microscopic examination revealed a multiloculated lesion lined by a simple flat epithelium and with a serious content, with abundant blood vessels with calcifications and cholesterol crystals, consistent with an adrenal endothelial cyst.
The pain improved after surgery, and the patient has been symptom-free since then.
Adrenal cyst is an uncommon condition. Only 300 cases have been reported in the literature,1 the first of which was described in 1690 by the Viennese pathologist Greiselius.3 Adrenal cyst incidence ranges from 0.06% and 0.18% depending on the series.1 Most of them are incidentally diagnosed. It is more common in females (3:1) and in patients aged 40–60 years. They are usually unilateral and occur with the same frequency in both adrenal glands. Only 7% of adrenal cysts are malignant or potentially malignant, and only 0.2% are metastatic in origin. Several classifications of adrenal cysts are available, of which the most widely used is the Foster classification (1966), which divides the cysts into four types: endothelial cysts (45%), pseudocysts (39%), epithelial cysts (9%), and parasitic cysts (7%).3 Endothelial cysts are divided into lymphangiomatous cysts and cystic hemangiomas, and epithelial cysts are of an embryonal origin or cystic adenomas. By contrast, pseudocysts are not true cysts because they have no lining. They are most probably caused by bleeding in the adrenal gland with subsequent encapsulation. Finally, echinococcus is the parasite most commonly found in parasitic cysts.1 Although cysts do not usually cause symptoms, they may induce pain due to the compression of adjacent structures, particularly if they are big. Severe cases of hypovolemic shock due to bleeding inside the cyst2 or sepsis caused by infection of a pseudocyst3 have been reported.
No agreement exists about the management of adrenal masses. Surgery is clearly indicated when tumor size is >6cm, malignancy is suspected, or progressive growth or endocrine activity are found. When imaging tests suggest a benign, non-secreting cyst less than 4cm in size, watchful waiting is the most widely used approach. However, the therapeutic approach to masses with sizes ranging from 4 and 6cm is not clear.4
Radiographic findings may be very helpful in deciding adequate management. A cystic image with fluid contents and an attenuation coefficient similar to water containing calcifications (occurring in up to 15% of cases) may suggest an adrenal cyst. Rozenblit et al. classified non-functioning cystic adrenal masses into four types based on radiographic criteria. Uncomplicated cysts are homogeneous cysts less than 6cm in size and with a wall less than 3mm thick; for this variety, regular monitoring is recommended to detect changes in nature or size. Complicated cysts are those with high attenuation values or non-homogeneous, with walls thicker than 5mm or with central or peripheral thick calcifications. Surgery is recommended for these cysts. Cysts greater than 5–6cm in size with attenuation values higher than water or with wall thicknesses between 3 and 5cm are considered indeterminate cysts. For these, lesion puncture or conservative management may be indicated.5 Fine needle aspiration (FNA) may be helpful for classifying the type of adrenal cyst or for differentiating it from cysts with other origins (liver, etc.).6 FNA should never be performed for lesions suspected of being parasitic cysts or pheochromocytoma. According to Neri and Nance, this procedure may improve compression symptoms in some patients while avoiding surgical resection.6 However, other authors think that FNA has a very limited role for establishing lesion malignancy, and that only the pathological study of surgical specimens can provide a definitive diagnosis.7
In our patient, surgery was decided upon because the CT image suggested a malignant lesion. However, an endothelial cyst was found. Cyst removal was also associated with an improvement in the symptoms which had led the patient to seek medical help. Although they are not the most common etiology of incidental adrenal masses, these cysts should be considered in differential diagnosis and when treatment is being decided.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please, cite this article as: Egaña Zunzunegui N, et al. Quiste endotelial adrenal con imagen preoperatoria sospechosa de malignidad. Endocrinol Nutr. 2012;59(3):215–24.