It is currently postulated that not all obese individuals have to be considered as pathological subjects. From 10% to 20% of obese people studied do not show the metabolic changes common in obese patients. The term “healthy obese” has been coined to refer to these patients and differentiate them from the larger and more common group of pathological obese subjects. However, the definition of “healthy obese” is not clear. Use of “healthy obese” as a synonym for obese without metabolic complications is risky. Clinical markers such as insulin resistance are used to identify this pathology. It is not clear that healthy obese subjects have lower morbidity and mortality than pathologically obese patients. According to some authors, healthy obese would represent an early stage in evolution toward pathological obesity. There is no agreement as to the need to treat healthy obese subjects.
Se postula actualmente que no todos los obesos tienen que considerarse como individuos patológicos. Entre un 10 y un 20% de los obesos estudiados no tienen las alteraciones metabólicas habituales en este tipo de pacientes. Se acuña el término de «obeso sano» para denominar a estos y diferenciarlos del colectivo más amplio y común de obesos patológicos. A pesar de todo, no está bien acotada la definición de «obeso sano». Utilizar «obeso sano» como sinónimo de obeso sin complicaciones metabólicas es arriesgado. Se utilizan marcadores clínicos como la resistencia insulínica para identificar esta enfermedad. No está claro que el obeso sano tenga una menor morbimortalidad que el obeso patológico. Según algunos autores, el obeso sano sería un estadio inicial hacia la evolución al estado de obesidad patológica. No hay unanimidad en la necesidad o no de tratar al obeso sano.
Obesity usually coexists with diseases such as type 2 diabetes mellitus; several types of hyperlipidemia (IIa, IIb, and IV); hyperuricemia and gout; high blood pressure; coronary artery disease; stroke; or some types of neoplasm. Obesity is similarly related to insulin resistance, a metabolic state acting as a metabolic link between most of the abovementioned diseases. However, not all obese people have metabolic changes. A small proportion of obese subjects, 10–20%, have no insulin resistance, carbohydrate metabolism disorders, or any of the risk factors so frequently associated with obesity. It is in these cases where one may wonder if there are healthy obese subjects. Is obesity a disease per se when the obese person has as only indicator a body mass index (BMI) greater than 30kg/m2? This question has not been adequately clarified, and it must be emphasized that there is not only one type of obesity. It is fully accepted that predominantly abdominal fat involves more risk than gluteal fat.1,2
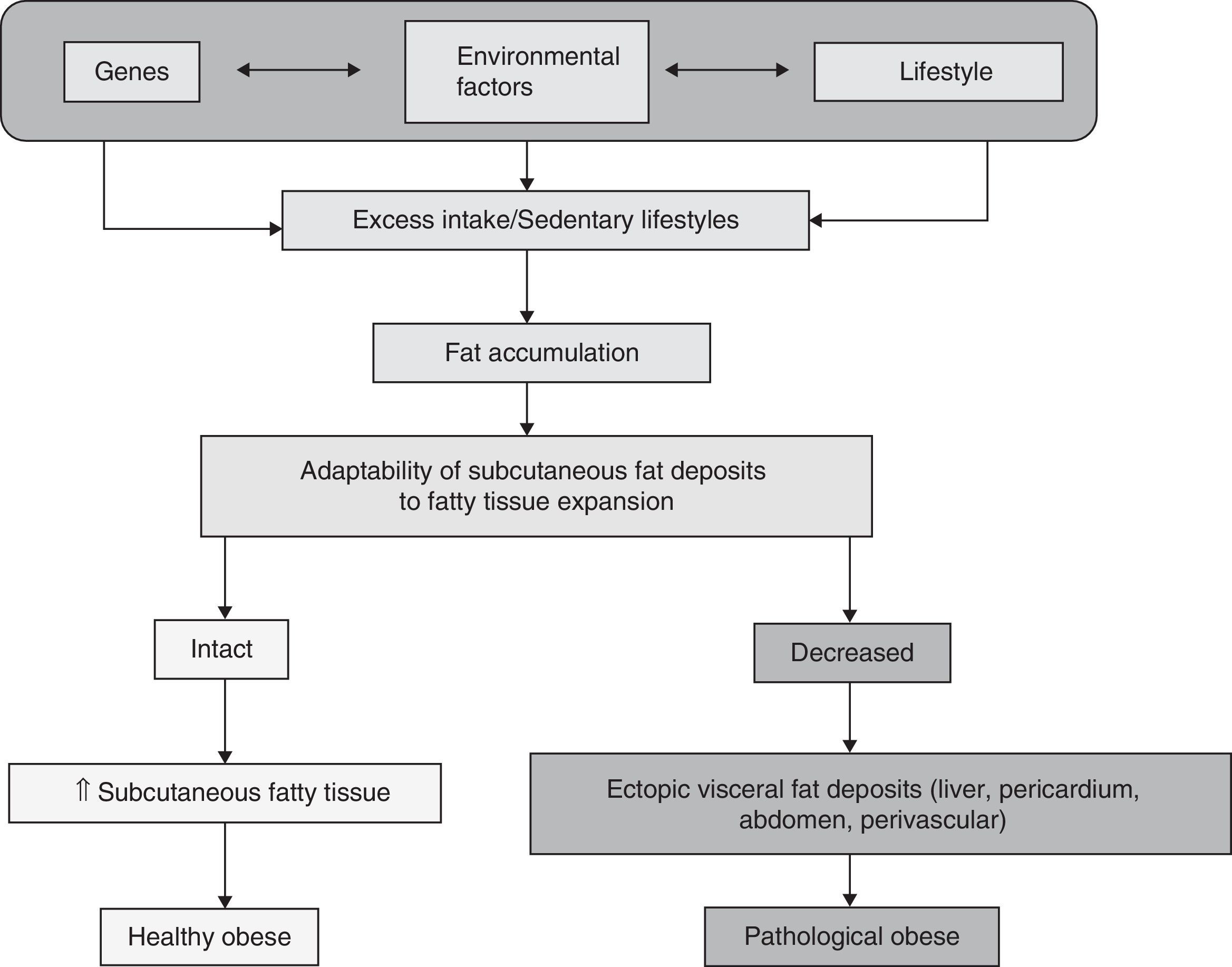
Definition of healthy obeseHealthy obese subjects may be defined as individuals with BMI >30kg/m2 who have no insulin resistance. The healthy obese represent a subpopulation consisting of approximately 10–25% of all obese subjects according to some studies.3 An Italian study reported a 27.5% prevalence of obese subjects without complications, irrespective of the degree and duration of obesity,4 while other studies reported a rate up to 30%.5 These obese subjects had no diabetes or high blood pressure, and their prevalence of insulin resistance was relatively low, according to the European Group for the Study on Insulin Resistance.6 This concept of “healthy obese person” therefore refers to subjects with BMI values higher than 30kg/m2 but no insulin resistance or any other added risk factor. Other authors define healthy obese people as “metabolically healthy obese” or, according to the Anglo-Saxon term, metabolically healthy but obese (MHO).7 Using the term insulin-sensitive obese for healthy obese subjects as opposed to insulin-resistant obese for pathological obese individuals, the difference lies, according to Blüer,3 in that healthy obese are able to accumulate excess fat in subcutaneous adipose tissue, expanding or increasing this tissue as needed, while in pathological obese subjects, subcutaneous fat deposits do not expand sufficiently and fat accumulates in other parts of the body. These are the so-called ectopic deposits, located in the liver, pericardium, mesenteries, etc. and forming so-called visceral fat. This fat is closely related to cardiovascular risk factors such as diabetes, high blood pressure, non-alcoholic fatty liver disease, hyperlipidemia and their common soil, insulin resistance,8 which constitute metabolic syndrome (MS) according to the recently agreed definition.9 It is also related to complications derived from these cardiovascular risk factors such as myocardial ischemia and infarction, cerebral ischemia and hemorrhagic events, etc. This potential for expansion when fat deposits occur differentiates healthy from pathological obese subjects (Fig. 1).
Clinical markersInsulin resistance may be considered as the best clinical marker of metabolic involvement in both healthy and pathological obese. Some studies suggest that an obese subject with no insulin resistance is a healthy obese.10 In some reports, inflammation has been reported to be a potential marker of the difference between healthy and pathological obese subjects.11 In this regard, an inflammatory marker such as C-reactive protein has been reported to be helpful for the identification of healthy obese as is done in MS.12 A biologically different population group in which a higher than normal weight does not represent an increase in metabolic risk is thus identified.13–15 It has also been noted that, in some healthy obese, weight loss induction may have unexpected effects such as increased parasympathetic cardiac tone, decreased systolic and diastolic blood pressure, and altered cortisol levels.16,17 Adiponectin represents another useful clinical maker in obesity. High adiponectin levels are associated with the healthy obese phenotype with no insulin resistance, in the same way as they are associated with a low risk of infarction in men.18 The role of ghrelin as an obesity marker and its relationship to healthy obese has also been studied. Ghrelin is a 28-amino acid peptide secreted in the stomach mainly by endocrine cells.19,20 It is directly involved in energy homeostasis, but its function in this is unknown. Plasma ghrelin levels increase when BMI decreases or weight loss occurs, and decrease when weight increases. Plasma ghrelin levels increase before meals and rapidly decrease after intake, and may be related to sensations of hunger and satiety respectively. The role of ghrelin in the pathophysiology of obesity is not sufficiently clear, and no differences have been shown in ghrelin levels between healthy and pathological obese subjects, nor are such levels related to increases or decreases in cardiovascular diseases.21
Other authors report as markers of normality in the healthy obese parameters such as the homeostasis model assessment (HOMA) index of insulin sensitivity, which should be less than 2.6 in the Spanish population,22 or less than 1.95 in other series.23 Circulating lipid levels should be as follows: triglycerides, less than 1.7mmol/L (150mg/dL); total cholesterol, less than 5.2mmol/L (200mg/dL); low density lipoprotein cholesterol (LDL-C), less than 2.6mmol/L (100mg/dL); and high density lipoprotein cholesterol (HDL-C), more than 1.1mmol/L (45mg/dL).7
Morbidity and mortalityIt has been questioned whether healthy obese subjects have the same morbidity and mortality as people with normal weight. Some six-year studies suggest that healthy obese subjects have a lower incidence of cardiovascular events than subjects of normal weight but insulin-resistant,24 while other studies do not consider obesity without MS to be a benign condition, but rather a condition associated with the presence of markers of subclinical cardiovascular damage.25 There have been no prospective studies following the natural history of healthy obesity. It is not known whether a subject who is considered a healthy obese at any given time may eventually become a pathological obese and develop the comorbidities inherent in obesity.26–28 According to this evaluation, healthy obesity is a stage prior to the development of comorbidities, rather than a different type of obesity where these metabolic changes do not occur. However, not all healthy obese become pathological obese.
The potential existence of another option as a non-pathological condition is determined by the fact that visceral fat levels are lower in healthy as compared to pathological obese. Abdominal fat is responsible for most metabolic complications in the pathological obese. Two obesity phenotypes are traditionally described based on fat distribution: a predominantly visceral obesity (also called central or android obesity) or a predominantly gluteal or gynoid obesity.29 In some obese subjects, adiponectin levels, which usually increase as BMI increases, are similar to those of normal weight subjects and could be related to the healthy obese phenotype.18 This fat distribution involves less cardiovascular risk than central obesity.24 This suggests that some subjects with gynoid obesity could be healthy obese.30 On the other hand, it is not clear that healthy obese subjects are able to maintain high insulin sensitivity throughout their lives.
Management of healthy obeseThis differentiation between healthy and pathological obese is of special interest when planning treatment. Pathological obese subjects will undoubtedly benefit from a program of diet and exercise aimed at decreasing BMI. Decreased weight is associated with a clear reduction in cardiovascular risk factors in pathological obese subjects, but it is not so clear that the same occurs in the healthy obese.31 Healthy obese subjects have no metabolic changes, so that weight loss will not have any additional effects. They may have musculoskeletal benefits, but no metabolic changes will occur as there is no metabolic impairment.
Once the existence, with whatever reservations, of healthy obese subjects has been recognized, the next stage should be to consider whether or not to treat them. If no pathological condition exists, why should they be treated?32 Is weight loss required in healthy obese subjects by the mere fact that they are not within the “normal” weight percentiles? They might achieve musculoskeletal benefits from weight loss, but their metabolic profile, which is otherwise within normal parameters, would not improve. The same would occur in a person with a normal weight who lost 1–2kg, but we would not even consider this possibility in this case because we consider him/her healthy. No clear answers to these questions are available. As not all authors agree on the existence of healthy obese subjects,25 there is not likely to be agreement regarding treatment any time soon. However, because of the multiple changes associated with obesity even when the cardiometabolic profile is normal, including sleep obstructive apnea syndrome,33 musculoskeletal changes, the increased risk of developing certain tumors (although some studies suggest that healthy obese have no greater incidence than insulin-resistant obese),4,34 reproductive abnormalities or changes in body self-image and the psychological dysfunctions which result from them, the treatment of these subjects with a healthy obese pattern is warranted.5
ConclusionsThe concept of the insulin-sensitive obese subject still requires further clarification, and agreement needs to be reached on its definition. As mentioned, there is no consensus on the definition of metabolic normality, although it revolves around the presence or absence of MS.35 If several years have been needed to reach a consensus on the clinical definition of MS,9 the same may occur with the definition of healthy obese and its recognition as an independent clinical condition.
Based on these studies and observations, we can state that not all obese subjects have metabolic disease, such as usually occurs in the obese who, in addition, normally have concomitant cardiometabolic risk factors. Despite this finding, the existence of an independent clinical condition that defines obese subjects with no insulin resistance is not yet generally agreed upon by all authors. If this condition were to be accepted as such, there would be a number of clinical markers available for identifying it in standard practice: insulin resistance (which would be part of the definition of healthy obesity), levels of ghrelin, maybe an adipokine (adiponectin), C-reactive protein, or the absence of the different cardiovascular risk factors most common in obesity. It is postulated that the clinical condition of healthy obesity is only an intermediate step toward the establishment of pathological obesity with all its common changes. If healthy obesity existed as a metabolically normal condition, it would be associated with non-metabolic conditions such as musculoskeletal problems and psychological changes in self-esteem or the perception of self-image that question the “normality” of this condition. In any case, it is not clear even here whether healthy obese subjects would benefit from specific treatment and whether this would therefore be needed.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Griera Borrás JL, Contreras Gilbert J. ¿Existe el obeso sano? Endocrinol Nutr. 2014;61:47–51.