This paper is a summary of the Spanish Federation of Nutrition, Food and Dietetics Associations (FESNAD) and the Spanish Association for the Study of Obesity (SEEDO) consensus document on the role of diet in prevention and treatment of overweight and obesity.
To prepare this document, and in order to achieve the maximum evidence level possible, a systematic review was made of all medical literature published between January 1, 1996 and January 31, 2011 (15 years). The obtained findings were cataloged by evidence level following the Scottish Intercollegiate Guidelines Network system, and recommendations were produced based on data collected.
As a result, 65 evidences and 31 recommendations applicable to obese adults without any other pathological process were produced.
Evidences and resulting recommendations are provided, and the most significant findings are discussed.
This consensus document is intended to provide healthcare professionals with a reference tool that may help them design dietary strategies for prevention and treatment of overweight and obesity.
El presente trabajo es un resumen del Documento de Consenso de la Federación Española de Sociedades de Nutrición, Alimentación y Dietética (FESNAD) y la Sociedad Española para el Estudio de la Obesidad (SEEDO) sobre el papel de la dieta en la prevención y el tratamiento de la obesidad y el sobrepeso.
Para la realización de dicho consenso, y buscando la mayor evidencia posible, se ha efectuado una revisión sistemática de los datos de la literatura médica desde el 1 de enero de 1996 al 31 de enero de 2011 (15 años). Se catalogaron los hallazgos obtenidos según grados de evidencia, siguiendo el sistema del Scottish Intercollegiate Guidelines Network, y en base a las mismas se establecieron unas recomendaciones.
Como resultado se han elaborado 65 evidencias y 31 recomendaciones que son de aplicación a sujetos adultos que, salvo la obesidad, no presenten otras patologías.
Se exponen todas las evidencias y recomendaciones resultantes y se aporta un comentario sobre los hallazgos más significativos.
Se pretende que el presente consenso pueda servir de referente a los profesionales de la salud en su labor de diseñar estrategias nutricionales de prevención o tratamiento de la obesidad y el sobrepeso.
The most recently published data concerning the prevalence of obesity and overweight in Spain1 are truly alarming both because of absolute values and because of their increase as compared to prior data.2 In this situation, and irrespective of institutional public health measures, it is healthcare professionals who are responsible for implementing measures aimed both at preventing obesity and at treating people who already have this problem.
It is obvious that obesity prevention and treatment should take into account the multiple factors which contribute to the occurrence of this condition. However, although all potential measures should be considered, diet is the mainstay for both prevention and treatment.
Because of the multiple nutritional approaches proposed for the management of excess weight, the Spanish Federation of Nutrition, Food and Dietetics Association (FESNAD) and the Spanish Association for the Study of Obesity (SEEDO) decided to undertake a joint effort to clarify the role of the different nutritional factors in both the prevention and treatment of obesity and overweight. A FESNAD-SEEDO consensus document which contains evidence-based nutritional recommendations to serve as a tool for healthcare professionals in the design of strategies for prevention or treatment regimens for obesity or overweight has been prepared for this purpose.
The full version of this consensus has previously been published,3–6 and this paper therefore provides a summary of the consensus and a discussion of its results by the authors.
Materials and methodsThe methods used in preparing this consensus have previously been reported.4 In short, it may be stated that in order to design the following recommendations, a review was made of the scientific literature covering the areas of general interest for the consensus which was published between January 1, 1996 and December 31, 2011. In agreement with the proposal by the National Health System,7 the criteria for the use of sources of information were based on the Medline database, which was used to collect systematic reviews and individual studies. Subsequently, other databases were consulted.
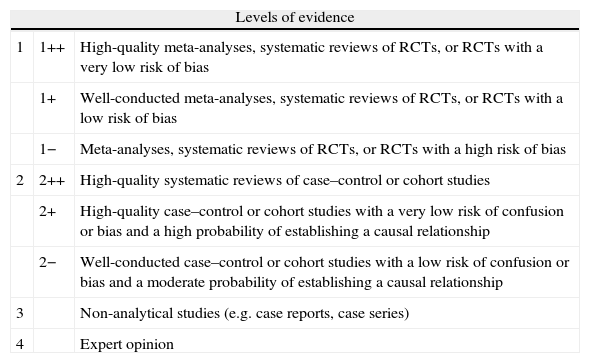
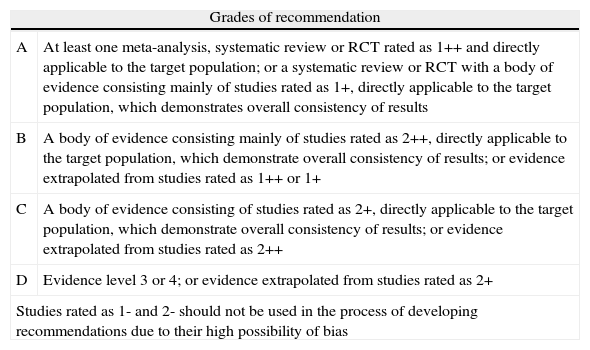
Based on the conclusions reached after this review, the evidence was classified and recommendations were made according to the method proposed in 2008 by the European Association for the Study of Obesity,8 which is a simplified version of the system advocated by the Scottish Intercollegiate Guidelines Network (SIGN)9 (Tables 1 and 2).
Levels of evidence.
| Levels of evidence | ||
| 1 | 1++ | High-quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias |
| 1+ | Well-conducted meta-analyses, systematic reviews of RCTs, or RCTs with a low risk of bias | |
| 1− | Meta-analyses, systematic reviews of RCTs, or RCTs with a high risk of bias | |
| 2 | 2++ | High-quality systematic reviews of case–control or cohort studies |
| 2+ | High-quality case–control or cohort studies with a very low risk of confusion or bias and a high probability of establishing a causal relationship | |
| 2− | Well-conducted case–control or cohort studies with a low risk of confusion or bias and a moderate probability of establishing a causal relationship | |
| 3 | Non-analytical studies (e.g. case reports, case series) | |
| 4 | Expert opinion | |
RCT: randomized, controlled trial.
Grades of recommendation.9
| Grades of recommendation | |
| A | At least one meta-analysis, systematic review or RCT rated as 1++ and directly applicable to the target population; or a systematic review or RCT with a body of evidence consisting mainly of studies rated as 1+, directly applicable to the target population, which demonstrates overall consistency of results |
| B | A body of evidence consisting mainly of studies rated as 2++, directly applicable to the target population, which demonstrate overall consistency of results; or evidence extrapolated from studies rated as 1++ or 1+ |
| C | A body of evidence consisting of studies rated as 2+, directly applicable to the target population, which demonstrate overall consistency of results; or evidence extrapolated from studies rated as 2++ |
| D | Evidence level 3 or 4; or evidence extrapolated from studies rated as 2+ |
| Studies rated as 1- and 2- should not be used in the process of developing recommendations due to their high possibility of bias | |
RCT: randomized, controlled trial.
Because of preparation criteria, the resulting document only applies to that part of the adult population (excluding pregnant and lactating women) which, apart from obesity, had neither malnutrition nor chronic diseases.
Finally, it should be noted that the representatives of the different societies cited in the list of authors reached a consensus on the views expressed in this document, which therefore represents the position of all of them.
ResultsA detailed rationale for the evidence obtained and the resulting recommendations has previously been published.3,5,6 This section lists all the evidence gathered after the review of the literature data, as well as evidence-based recommendations by the authors.
Diet for prevention of obesityEnergy balance and body weightEnergy densityEvidence1. High energy density dietary patterns may lead to weight increase in adults (level 1+ evidence).
Recommendations1. Weight increase may be prevented by diets containing food items with low energy density (grade A recommendation).
Energy balance and obesogenic environmentEvidence2. A lack of supermarkets offering fruit and vegetables or the location of such supermarkets at a long distance, particularly from human settlements with disadvantaged socioeconomic levels, are factors which condition a higher mean body mass index (BMI) in the population (level 1+ evidence).
Recommendations2. Strategies to promote food availability and access to healthy food, especially fruit and vegetables, should be devised in order to create a favorable environment in which mean population BMI can be maintained (grade A recommendation).
Energy balance: Eating outEvidence3. The habitual intake of fast food (more than once weekly) may contribute to an increase in energy intake and to weight gain and obesity (level 1+ evidence).
Recommendations3. The restriction of the habitual intake (more than once weekly) of fast food may prevent the weight gain due to this factor (grade A recommendation).
Energy balance: Size of portionsEvidence4. Offering bigger portions of food increases energy intake (level 2++ evidence).
Recommendations4. Offering smaller portions restricts energy intake (grade B recommendation).
Energy balance: BreakfastEvidence5. Research into the relationship between going without breakfast in adults and the risk of overweight and obesity is controversial and inconsistent.
Energy balance: SnacksEvidence6. Research suggesting that the intake of snacks is associated with weight increase is controversial and inconsistent.
Energy balance: FrequencyEvidence7. Research analyzing the relationship between meal frequency and body weight changes is inconsistent.
Feeding patterns and body weightMediterranean dietEvidence8. While the results available are inconsistent, studies suggest a potential role for the Mediterranean diet (MedDiet) in the prevention of overweight and obesity (level 2−evidence).
9. The available evidence suggests that increased adherence to MedDiet could prevent an increase in abdominal circumference (level 2+ evidence).
Recommendations5. Increased MedDiet adherence could prevent overweight and obesity and prevent an increase in abdominal circumference (grade C recommendation).
Vegetarian dietsEvidence10. Vegetarian diets are associated in healthy adults with a lower BMI (level 2+ evidence).
Recommendations6. The intake of vegetarian diets could lead to a smaller weight gain over time in healthy adults (grade C recommendation).
Nutrients and body weightCarbohydratesEvidence11. Diets with a higher content of complex carbohydrates (≥50% of total energy intake, approximately) are associated with lower BMI in healthy adults (level 2+ evidence).
12. The evidence of an association between the physical characteristics of carbohydrates (liquid or solid), energy intake, and body weight is controversial.
13. There is insufficient evidence to show that the glycemic index (GI) and glycemic load (GL) of the diet are associated with an increased body weight in adults with no disease.
Recommendations7. Diets for healthy adults aimed at preventing weight gain should contain a significant proportion of complex carbohydrates (50% or more of the total energy intake approximately) (grade C recommendation).
LipidsEvidence14. Fat intake after adjustment for energy intake is not associated with weight gain in healthy adults (level 2+ evidence).
15. Research into the relationship between the intake of saturated fatty acids in healthy adults and the risk of obesity provides conflicting results.
16. The intake of monounsaturated fatty acids has not been associated with weight gain in healthy adults (level 2+ evidence).
17. The intake of polyunsaturated fatty acids has not been associated with weight gain in healthy adults (level 2+ evidence).
18. The evidence relating to the intake of omega-3 fatty acids and their impact on weight change or the prevention of excess weight in adults is insufficient to allow any recommendations to be made.
19. The limited epidemiological studies available show a consistent relationship as regards the role of trans fatty acids in weight gain and abdominal fat increase (level 2−evidence).
Recommendations8. To prevent weight gain in healthy adults, control of total energy intake is more important than control of total fat intake (grade C recommendation).
ProteinEvidence20. The evidence relating to total protein intake and its impact on weight change or prevention of excess weight in adults is insufficient to allow any recommendations to be made.
21. The evidence relating to animal protein intake and its impact on weight change or prevention of excess weight in adults is insufficient to allow any recommendations to be made.
22. The evidence relating to vegetable protein intake and its impact on weight change or the prevention of excess weight in adults is insufficient to allow any recommendations to be made.
23. Regarding the intake of vegetable proteins (soya) and its impact on weight change, there is no evidence available that would justify the making of any recommendations concerning weight gain prevention in adults.
Vitamins and mineralsEvidence24. The available evidence suggests that calcium supplementation is not associated with a lower weight gain (level 1+ evidence).
25. The available evidence suggests that combined calcium and vitamin D supplementation induces no clinically relevant improvements in body weight control in postmenopausal women (level 1+ evidence).
26. The evidence for the role of vitamin D alone in preventing weight gain in healthy adults is controversial and does not allow for any conclusions to be drawn.
Dietary fiberEvidence27. A high fiber intake in the setting of a diet rich in food of vegetable origin is associated with a better body weight control in healthy adults (level 2++ evidence).
Recommendations9. An increased intake of fiber from food of vegetable origin may prevent weight gain in healthy adults (grade B recommendation).
WaterEvidence28. The evidence relating to water consumption and its impact on weight change or the prevention of excess weight in healthy adults is insufficient to allow any recommendations to be made.
EthanolEvidence29. Studies report conflicting and inconsistent observations, although some evidence suggests a certain association between high ethanol consumption and weight gain (level 2−evidence).
Recommendations10. Limiting high ethanol consumption could prevent weight gain due to this factor (grade D recommendation).
Food and body weightFruit and vegetablesEvidence30. A high intake of fruit and vegetables is associated with a smaller weight increase in adults in the long term (level 2+ evidence).
Recommendations11. Dietary prevention of weight increase may be modulated by diets with a high content of fruit and vegetables (grade C recommendation).
Whole grain cerealsEvidence31. A high intake of whole grain cereals is associated with lower BMI (level 2+ evidence).
Recommendations12. It is recommended that, to prevent weight gain, diets should contain a significant amount of whole grain cereal (grade C recommendation).
SugarsEvidence32. The evidence for the relationship of the intake of free or total sugars (except in sugar-sweetened drinks) to body weight gain is controversial.
Sugar-sweetened drinksEvidence33. Frequent intake of sugar-sweetened drinks is associated with higher BMI (level 2+ evidence).
Recommendations13. A restricted intake of sugar-sweetened drinks may lead to a smaller weight gain over time (grade A recommendation).
Olive oilEvidence34. The intake of olive oil does not appear to be associated with a significant risk of weight gain in healthy adults (level 2−evidence).
NutsEvidence35. The addition of nuts to the usual diet is not associated with body weight increase (level 2+ evidence).
Recommendations14. The moderate intake of nuts has advantages regarding the prevention of chronic diseases without compromising the risk of weight gain (grade C recommendation).
Other: MeatEvidence36. A high intake of meat and processed meat products may increase weight gain and abdominal circumference (level 2+ evidence).
Recommendations15. Restricting a high intake of meat and meat products may prevent weight gain due to this factor (grade C recommendation).
Diet for the treatment of obesityBalanced low-calorie diet: Feeding patternsEvidence37. Energy reduction in the diet by 500–1000kcal daily may result in a weight loss ranging from 0.4 to 1kg/week, equivalent to an 8% weight loss in an average time of 6 months (level 1+ evidence).
38. Several measures, such as a decrease in portion size or energy density of the diet, may facilitate compliance with a low-calorie diet and weight loss in patients with obesity (level 3 evidence).
Recommendations16. An energy deficit of 500–1000kcal daily as compared to the energy requirements of adult obese patients is sufficient to induce an 8% weight loss in the first 6 months of treatment (grade A recommendation).
17. In dietary treatment, decreases in portion size and/or energy density of the diet are strategic measures which are effective in reducing weight in obese patients (grade D recommendation).
Diet composition:Diets modifying fat vs carbohydratesEvidence39. As compared to a low-fat diet (LFD), a low-carbohydrate diet (LCHD) achieves a greater weight loss in the short term (6 months) (level 1++ evidence).
40. In the long term (one year or longer), a LCHD is associated with a weight loss similar to that achieved with a low-fat diet (LFD) (level 1+ evidence).
41. In the long term (one year or longer), a LCHD results in a greater increase in high density lipoprotein (HDL) and a greater decrease in triglycerides as compared to a diet low in saturated fat (level 1+ evidence).
42. In the long term (one year or longer), a diet low in saturated fat results in a greater decrease in low density lipoprotein (LDL) as compared to a LCHD (level 2+ evidence).
43. Low-carbohydrate diets cause more adverse effects than LFDs (level 2++ evidence).
44. The very long-term mortality of LCHDs may be increased if the fat is from animal sources (level 3 evidence).
Recommendations18. Decreasing the proportion of carbohydrates and increasing the proportion of fat is not useful for enhancing the effect of diet on weight loss (grade A recommendation).
19. LFDs are effective in controlling LDL cholesterol in obese subjects, while levels of HDL cholesterol and triglycerides are better controlled by LCHDs (grade B recommendation).
20. Low-carbohydrate diets should not contain a high percentage of animal fats (grade D recommendation).
Diets modifying the type of carbohydratesFiber-enriched dietsEvidence45. There are no adequate data available which show the role of diet enriched with fiber or whole grain cereals on weight loss.
46. Glucomannan supplements added to the diet may have a modest effect through a satiety mechanism, promoting weight loss (level 1+ evidence).
47. Fiber supplements other than glucomannan added to the diet may minimally contribute to weight loss (level 2+ evidence).
48. The management of obesity with a diet enriched or supplemented with glucomannan, plantago ovata, and β-glucans decreases LDL cholesterol levels in obese patients (level 1+ evidence).
Recommendations21. In the management of obesity, fiber supplements (mainly glucomannan) may increase the efficacy of the diet for weight loss (grade C recommendation).
22. Obese subjects with lipid changes may benefit from the prescription of diets enriched with fiber or fiber supplements (mainly glucomannan) (grade B recommendation).
Diets with low glycemic indexEvidence49. Changes in GI or GL of diet have no persistent effect on weight loss in the management of obesity (level 1+ evidence).
50. There are no adequate data available which show the role of diets with low GI or GL on the maintenance of weight lost after a low-calorie diet.
Recommendations23. A decrease in GI and GL cannot be recommended as a specific strategy for the dietary management of obesity (grade A recommendation).
High-protein dietsEvidence51. High-protein diets may induce in the short term (less than 6 months) a greater weight loss than a carbohydrate-rich conventional diet (level 2+ evidence).
52. High-protein diets do not induce in the long term (more than 12 months) a greater weight loss than a carbohydrate-rich conventional diet (level 1+ evidence).
53. There are currently no adequate data which establish the efficacy of high-protein diets for the maintenance of weight lost after an initial weight loss with other types of diet.
54. High-protein diets promote the preservation of lean mass better than carbohydrate-rich diets (level 2+ evidence).
55. In the very long term, high-protein diets may increase the risk of total and cardiovascular mortality, particularly when the protein is from animal sources (level 2+ evidence).
Recommendations24. For the management of obesity, changes in the proportion of protein in the diet are not recommended (grade A recommendation).
25. To guarantee lean mass maintenance or increase during a low-calorie diet, it is effective to increase dietary protein content above 1.05g/kg (grade B recommendation).
26. If a high-protein diet is prescribed, the provision of animal protein should be restricted to the prevention of an increased risk of mortality in the long term (grade C recommendation).
Meal replacement dietsEvidence56. The use of commercial preparations as substitutes for one or more meals may facilitate adequate compliance with a low-calorie diet, thus promoting both weight loss and the maintenance of weight lost (level 1 evidence).
57. This beneficial effect is greater when they are used in the setting of structured treatments including exercise schemes, education, and changes in dietary behavior (level 3 evidence).
58. No clinically significant adverse effects associated with the use of meal substitutes in the setting of low-calorie diets have been reported (level 3 evidence).
Recommendations27. The replacement of some meals by meal substitutes in the setting of low-calorie diets may be helpful for weight loss and the maintenance of weight loss in obese and overweight adults (grade D recommendation).
Very low-calorie dietsEvidence59. In the short term (less than 3 months), very low-calorie diets (VLCDs) (400–800kcal/day) induce a greater weight loss than diets with a low-calorie content (>800kcal/day) (level 1+ evidence).
60. In the long term (longer than one year), these diets do not induce a greater weight loss than low-calorie diets (level 1+ evidence).
61. In patients with liver steatosis and increased surgical risk undergoing bariatric surgery, the use of VLCDs before surgery may decrease surgical risk (level 1+ evidence).
62. There are currently no adequate data available to establish whether in the immediate postoperative period after bariatric surgery, VLCD with commercial products contributes to the achievement of an adequate protein intake by the patient.
63. VLCDs involve a greater risk of adverse effects as compared to low-calorie diets (level 1−evidence).
64. The currently available evidence does not allow it to be stated that VLCDs are associated with a greater lean versus fat mass loss as compared to less restrictive low-calorie diets.
Recommendations28. VLCDs may be used to manage patients with obesity based on a specific clinical indication and with close medical monitoring (grade D recommendation).
29. VLCDs should not be used in patients who do not meet the established indications and requirements (grade A recommendation).
30. The use of VLCDs may be warranted before bariatric surgery in patients with liver steatosis and increased surgical risk, under medical monitoring and with the potential adverse effects that may occur being taken into consideration (grade B recommendation).
31. The use of VLCDs with commercial products may be warranted in the immediate postoperative period after bariatric surgery as a contribution to the achievement of an adequate protein intake by the patient (grade D recommendation).
Mediterranean dietEvidence65. There is no adequate scientific evidence to suggest that MedDiet, under isocaloric conditions, results in a greater weight loss than other types of diet in the treatment of obesity.
DiscussionAs may be seen, 65 pieces of evidence and 31 recommendations were obtained after the review of the literature data. The evidence obtained may be categorized into three types:
- -
Those where the element analyzed has been shown to be helpful in achieving the objective (the prevention and treatment of obesity and overweight).
- -
Those in which the element has been shown to be ineffective.
- -
Those in which insufficient or conflicting data are available and no conclusions regarding the effectiveness or ineffectiveness of the concerned element can be drawn.
When scientific evidence in nutrition and diet therapy is examined, it should not be forgotten that clinical research in nutrition has unique characteristics that differentiate it from the traditional clinical trial which assesses the efficacy of a drug. In the latter case, where homogeneous groups of patients who receive different treatments (drugs, placebo) are compared, treatment compliance rarely represents a significant problem. Studies of this type usually provide reliable data that usually agree with those from other studies. By contrast, in clinical trials comparing different types of diet or feeding schemes, patient adherence to treatment is much more difficult to achieve. Patients often gradually move away from the prescribed dietary regimens during the course of the study. This has been demonstrated in many studies where the analysis of dietary intake during the study often shows that patients move away from the dietary goals initially established for each group. As a result, the dietary characteristics of the different groups become more similar at the end of the study and it is more difficult to find significant differences between them. This is the reason for the lack of conclusive findings in many studies or for the conflicting results reported by theoretically similar trials.
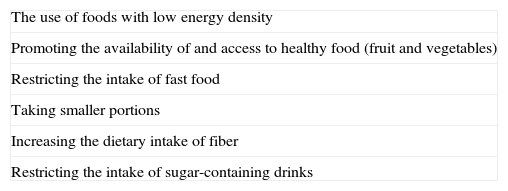
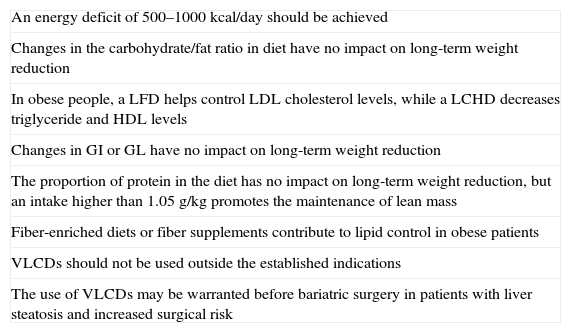
Despite such difficulties, high-level evidence has been obtained and essential recommendations have been made for a number of factors. Among the recommendations which are based on strong evidence (grade A and B recommendations), a distinction may be made between those referring to prevention (Table 3) and those related to treatment (Table 4).
Most important recommendations (grade A and grade B) for the prevention of obesity and overweight through diet.
| The use of foods with low energy density |
| Promoting the availability of and access to healthy food (fruit and vegetables) |
| Restricting the intake of fast food |
| Taking smaller portions |
| Increasing the dietary intake of fiber |
| Restricting the intake of sugar-containing drinks |
Most important recommendations (grade A and grade B) for the treatment of obesity and overweight through diet.
| An energy deficit of 500–1000kcal/day should be achieved |
| Changes in the carbohydrate/fat ratio in diet have no impact on long-term weight reduction |
| In obese people, a LFD helps control LDL cholesterol levels, while a LCHD decreases triglyceride and HDL levels |
| Changes in GI or GL have no impact on long-term weight reduction |
| The proportion of protein in the diet has no impact on long-term weight reduction, but an intake higher than 1.05g/kg promotes the maintenance of lean mass |
| Fiber-enriched diets or fiber supplements contribute to lipid control in obese patients |
| VLCDs should not be used outside the established indications |
| The use of VLCDs may be warranted before bariatric surgery in patients with liver steatosis and increased surgical risk |
GL: glycemic load; LFD: low-fat diet; LCHD: low-carbohydrate diet; VLCDs: very low calorie diets; GI: glycemic index.
As regards prevention, the strongest evidence was related to a decrease in total energy provision, either directly (portion size and energy density) or indirectly (intake of fiber and fruit and vegetables by a potential satiety mechanism or fast food restriction with a probable decrease in energy density).
The level of evidence for MedDiet, vegetarian diets, the restriction of total energy or ethanol, and the consumption of fruit and vegetables is inadequate, and further studies with improved designs are needed to obtain more solid evidence.
As regards treatment, the traditional concept of global energy reduction already recommended by the 2004 guidelines of the Spanish Association of Endocrinology and Nutrition10 or the 2007 guidelines of the Spanish Association for the Study of Obesity11 continues to be fully applicable and soundly based. By contrast, other alternatives related to a modification of the proportions of the different components in the diet or their characteristics have become popular in recent decades but have not been shown to be effective in the long term. It is true that a greater weight loss has been seen with diets containing higher proportions of fat or protein than the traditional diet, which explains the success of these nutritional approaches which are used in some popular diets. However, the long-term ineffectiveness of these diets militates against their use for the treatment of a chronic condition such as obesity. Moreover, in addition to this lack of efficacy, there are data suggesting an increased mortality in the very long term with diets rich in animal fat or protein.
Overall, these findings agree with both the traditional recommendations by the World Health Organization (WHO)12 and the North American Association for the Study of Obesity (NAOS) (Strategy for Nutrition, Physical Activity, and Prevention of Obesity)13 and the most recent recommendations in the 2010 Dietary Guidelines for Americans.14 In Europe, the European Association for the Study of Obesity (EASO) reports similar conclusions in its 2008 Clinical Practice Guidelines.15
The review conducted also allowed us to confirm the positive role of fiber in excess weight control. The strongest evidence refers to its preventive effect, but data supporting a positive effect in treatment, as well as its contribution to lipid control in obese subjects with hyperlipidemia, were also found.
VLCDs achieve a greater weight loss in the short term as compared to a conventional low-calorie diet. However, they have shown no greater long-term efficacy and are associated with a higher risk of adverse effects. They are therefore only recommended for specific indications and under close medical monitoring. The use of VLCDs may be warranted before bariatric surgery in order to decrease the surgical risk in patients with liver steatosis. The WHO in 200712 and EASO in 200814 both warned of the short-lived effect of this type of diet and the need for reserving it for very specific patients.
When deciding treatment, weight maintenance is as important as the initial weight loss achieved. We all know that any obese subject who follows a diet achieves an initial weight loss relatively easily, but that the recovery of lost weight is an inexorable outcome in most subjects who initially lose weight, and is the most common reason for the long-term failure of treatment for obesity. With regard to this very important aspect, no conclusive data could be found in the literature as to whether modifications in the proportions of the different components of diet or in their characteristics might have an impact on this objective.
In addition to the maintenance of weight loss, conclusive data are also lacking on other aspects. For example, there is no scientific evidence which supports the non-skipping of breakfast or the distribution of food intake, which are usually perceived as factors related to weight control. That is, there are still many aspects related to obesity prevention and treatment which need to be clarified, possibly because of the previously discussed methodological difficulties of studies of this type.
It may be expected that additional data allowing for the extension or modification of the recommendations agreed in this consensus will be available in the near future. Meanwhile, the authors of this consensus have attempted to provide all interested clinicians with a document that, based on the current scientific evidence, clarifies the value or ineffectiveness of different dietary measures for both the prevention and treatment of excess weight.
FundingThe consensus document summarized in this article was funded with the contribution of Nutrition & Santé/biManán according to the terms set down in the collaboration agreement jointly signed with FESNAD and SEEDO.
Conflict of interestThe authors state that they have no conflicts of interest.
The authors would like to acknowledge the Spanish Agency for Food Safety and Nutrition of the Ministry of Health, Social Policy and Equal Rights (AESAN) for its collaboration in the preparation of this document.
Coordinating writer: Manuel Gargallo Fernández (SEEDO).
Associate writers: Julio Basulto Marset (AEDN); Irene Bretón Lesmes (SEEN); Joan Quiles Izquierdo (SENC).
Coordination: Jordi Salas-Salvadó (FESNAD); Xavier Formiguera Sala (SEEDO).
Reviewers: Juan Manuel Ballesteros Arribas (AESAN); Miguel Ángel Martínez-González (Clínica Universitaria de Navarra); José María Ordovás Muñoz (Tufts University, Boston, USA); Miguel Ángel Rubio Herrera (Hospital Clínico Universitario de Madrid).
Chairman: Jordi Salas-Salvadó (SENPE).
Vice-chairwoman: María Dolores Romero de Ávila (ALCYTA).
Treasurer: Antonio Villarino Marín (SEDCA).
Secretary: Giuseppe Russolillo (AEDN).
Members: Rosaura Farré Rovira (SEN), Manuel Gargallo Fernández (SEEDO), Carlos Iglesias Rosado (SENBA), Herminia Lorenzo Benítez (ADENYD), José Manuel Moreno Villares (SEGHNP), Joan Quiles Izquierdo (SENC), Pilar Riobó Serván (SEEN).
Chairmen of the federated associations: Herminia Lorenzo Benítez (ADENYD), Giuseppe Russolillo (AEDN), María Dolores Romero de Ávila (ALCYTA), Antonio Villarino Marín (SEDCA), Xavier Formiguera Sala (SEEDO), Javier Salvador Rodríguez (SEEN), Luis Peña Quintana (SEGHNP), Rosaura Farré Rovira (SEN), Miguel Ángel Gassull Duró (SENBA), Javier Aranceta Bartrina (SENC), Abelardo García de Lorenzo (SENPE).
FESNAD (SPANISH Federation of Nutrition, Food and Dietetics Associations): ADENYD (Spanish Association of Nutrition and Dietetic Nurses); AEDN (Spanish Association of Dieticians and Nutritionists; ALCYTA (Spanish Association of Doctors and Graduates in Food Science and Technology); SEDCA (Spanish Association of Dietetics and Food Sciences); SEEN (Spanish Association of Endocrinology and Nutrition); SEEDO (Spanish Association for the Study of Obesity); SEGHNP (Spanish Association of Pediatric Gastroenterology, Hepatology and Nutrition); SEN (Spanish Association of Nutrition); SENBA (Spanish Association of Basic and Applied Nutrition); SENC (Spanish Association of Community Nutrition); SENPE (Spanish Association of Parenteral and Enteral Nutrition).
The members of the Consensus Group FESNAD-SEEDO are included in Appendix 1.
Please cite this article as: Gargallo Fernández M, et al. Resumen del consenso FESNAD-SEEDO: recomendaciones nutricionales basadas en la evidencia para la prevención y el tratamiento del sobrepeso y la obesidad en adultos. Endocrinol Nutr. 2012;59(7):429–37.