Nodular thyroid disease is a common condition in our clinical practice, and fine needle aspiration biopsy (FNAB) is the diagnostic procedure of choice. Its main limitation is the number of non-diagnostic samples. Since the Bethesda criteria were implemented in 2007 (a consensus document on the morphologic criteria and diagnostic terminology for interpretation of thyroid cytological samples), a higher prevalence of non-diagnostic FNAB was shown. In addition to the standard technique, we decided to collect and centrifuge the material remaining in puncture needles by washing them in a ThinPrep® solution, and to assess the increase in the diagnostic yield of FNAB after this change.
Patients and methodsSystematic sampling of 168 patients who underwent FNAB at the Nutrition and Endocrinology Department of the Xeral-Cies Hospital (Vigo, Spain) from January 2010 to November 2011 was done. Patients were classified into 2 groups: 75 patients in whom the residual material in the needle was not collected (non-washing group) and 93 patients in whom the material was collected (washing-group). All FNABs were performed by the same endocrinologist. Data are shown as percentage (±standard error) for ordinal variables or as mean (±standard deviation) for quantitative variables. A Chi-square test was used for statistical analysis of comparisons between percentages, and a Student's t-test for comparisons between quantitative variables. A value of p<0.05 was considered statistically significant.
ResultsNo significant differences were found between the groups in age, sex, plasma TSH levels or nodule size. The rate of non-diagnostic FNABs was 44% (±0.06) in the non-washing group and 17.2% (±0.04%) in the washing group, with a significant difference (p<0.01).
DiscussionCollection and subsequent processing of the residual material in the needle after FNAB significantly decreased the prevalence of non-diagnostic punctures in our patients. Collection of the residual material in the needle in this way is strongly recommended.
La enfermedad nodular tiroidea es un proceso frecuente en nuestra práctica clínica y la punción-aspiración con aguja fina (PAAF) es la técnica diagnóstica de elección. Su mayor limitación es la prevalencia de muestras no diagnósticas. Desde la implantación en 2007 de los criterios de Bethesda (documento de consenso sobre los criterios morfológicos y la terminología diagnóstica en la interpretación de las extensiones citológicas de tiroides) se demostró en nuestro servicio una mayor prevalencia de PAAF no diagnósticas. Decidimos añadir a la técnica habitual la recogida y el centrifugado del material remanente en las agujas de punción mediante lavado en una solución ThinPrep® y evaluar el aumento de la rentabilidad diagnóstica de la PAAF tras este cambio.
Pacientes y métodosMuestreo sistemático de 168 pacientes a los que se realizó una PAAF en el Servicio de Endocrinología y Nutrición del Hospital Xeral-Cíes de Vigo desde enero de 2010 hasta noviembre de 2011, que se clasificaron en 2 grupos: 75 pacientes en los que no se recogió el material remanente en la aguja de punción (grupo sin lavado) y 93 pacientes en los que sí se recogió dicho material (grupo con lavado). Todas las punciones fueron realizadas por el mismo endocrinólogo. Los datos se presentan como porcentaje del total (± error estándar) en el caso de variables ordinales o como media (± desviación estándar) en el caso de las cuantitativas. El análisis estadístico de las comparaciones entre porcentajes se hizo usando el test de ji al cuadrado y el de las comparaciones entre variables cuantitativas con la t de Student. Se consideraron significativas las diferencias con una probabilidad de error inferior a 0,05.
ResultadosNo encontramos diferencias significativas en la edad de los pacientes, el sexo, la concentración plasmática de TSH o el tamaño de los nódulos al comparar ambos grupos. El porcentaje de PAAF no diagnósticas en el grupo de pacientes sin lavado fue de 44% (± 0,06) y en el grupo con lavado de 17,2% (± 0,04). La diferencia entre ambos porcentajes fue significativa con p<0,01.
DiscusiónLa recogida y posterior procesado del remanente de la aguja con la que se realiza una PAAF redujo de forma muy significativa la prevalencia de punciones no diagnósticas en nuestros pacientes. Recomendamos que se recoja de esta forma el material remanente en la aguja en todas las PAAF de tiroides.
Nodular thyroid disease occurs in 4–7% of the overall adult population.1,2 The procedure of choice for cytological diagnosis of this condition is fine needle aspiration (FNA). Three to six nodule punctures are performed with a 22–25G needle, followed by gentle aspiration, and the resulting material is smeared onto glass slides.3 FNA allows for selecting patients amenable to thyroidectomy and for planning the surgical procedure.4
The Bethesda criteria, implemented in 2007, are a set of guidelines for the morphological criteria and diagnostic terms to be used for interpreting thyroid cytological smears.5 These criteria require the presence in the smear of at least six groups of follicular cells of 10 or more cells each, and classify the sample into one of six categories: benign, atypia of undetermined significance, follicular neoplasm, suspicious for malignancy, malignant, and nondiagnostic. The prevalence of nondiagnostic samples is the main limitation of FNA. Such prevalence ranged from 15% to 20%3,6–8 in series analyzed before the implementation of the Bethesda criteria.
Thyroid FNA has been performed at our department since January 2009, when an endocrinologist experienced in this procedure joined our hospital. Twelve months later, an analysis of results showed a high prevalence of nondiagnostic FNA. It was therefore decided, in agreement with the pathology department, to complete the procedure by collecting the material remaining in puncture needles by washing them in a ThinPrep® solution. This study assesses the increase in diagnostic yield of FNA after this change.
Patients and methodsA systematic sampling was made of all patients undergoing FNA at the department of endocrinology and nutrition of Xeral-Cíes Hospital in Vigo from January 2010 to November 2011. The resulting sample of 168 patients was divided into two groups, 75 patients from whom material remaining in the puncture needle was not collected (group without washing) and 93 patients from whom this material was collected (group with washing).
All punctures were performed by the same endocrinologist experienced in the procedure. FNA was performed with the patient lying supine and with the neck extended. Povidone iodine solution (Betadine®) was applied onto the skin overlying the nodule, which was punctured with a 22G needle coupled to a 20mL syringe held by a Cameco® plunger, and gentle aspiration was applied once the tip reached the desired position until fluid material was seen in the needle cap. The material was smeared onto two slides, and water-soluble fixative (Cytofix® aerosol) was applied to one of them at a distance of 20cm. This process was repeated from three to six times, depending on the amount of material.
In patients from the group with washing, in addition to the described process, the material remaining in the needles was rinsed in 20mL of ThinPrep® solution (Cytyc Corporation).9–12
At the pathology department, non-fixed smears were left to dry in the air and were stained using the Romanowsky method (DIFF-QUICK®). Fixed smears were stained with the Papanicolaou technique,13,14 and needle washing fluid was prepared by a process including homogenization, dispersion, filtering, and the transfer of cells to a slide, followed by cell staining using the Papanicolaou technique. Each sample was assigned to one of the six categories of the Bethesda classification, which allowed for separating patients with non-diagnostic cytology from the rest (those classified in the other five categories).
Data are given as percentage of the total (±standard error) for ordinal variables, or a mean (±standard deviation) for quantitative variables. Statistical analysis of comparisons between percentages was performed using a Chi-square test, while a Student's t-test was used to analyze comparisons between quantitative variables. Differences with a value of p<0.05 were considered statistically significant.
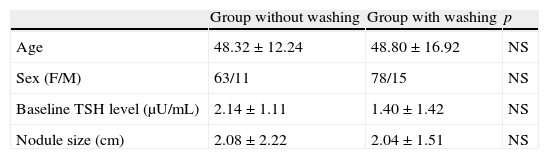
ResultsTable 1 shows the characteristics of study patients. No significant differences were found in patient age, proportion of males and females, plasma TSH levels, or nodule size between the groups with and without needle washing.
Baseline characteristics of the two patient groups undergoing fine needle aspiration.
| Group without washing | Group with washing | p | |
| Age | 48.32±12.24 | 48.80±16.92 | NS |
| Sex (F/M) | 63/11 | 78/15 | NS |
| Baseline TSH level (μU/mL) | 2.14±1.11 | 1.40±1.42 | NS |
| Nodule size (cm) | 2.08±2.22 | 2.04±1.51 | NS |
NS, not significant.
Sex figures are absolute values. Mean±standard deviation for all other variables.
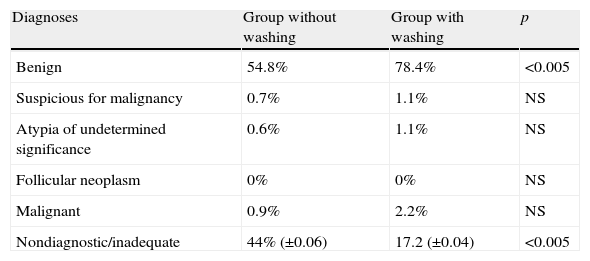
The proportions of nondiagnostic cytologies were 44% (±0.06) and 17.2% (±0.04) in the patient groups without and with needle washing, respectively. The difference between both percentages was significant (p<0.01).
As regards the distribution of cytological results in diagnostic FNA, in the group with no needle washing, 54.8% of the remaining cytologies were rated as benign, 0.7% as suspicious for malignancy, 0.6% as atypia of undetermined significance, and 0.9% as malignant. In the group with needle washing, 78.4% were rated as benign, 1.1% as suspicious for malignancy, 1.1% as atypia of undetermined significance, and 2.2% as malignant. The only significant differences were found between benign cytologies in both groups (Table 2).
Differences in distribution of cytological results of fine needle aspiration between the groups without and with needle washing.
| Diagnoses | Group without washing | Group with washing | p |
| Benign | 54.8% | 78.4% | <0.005 |
| Suspicious for malignancy | 0.7% | 1.1% | NS |
| Atypia of undetermined significance | 0.6% | 1.1% | NS |
| Follicular neoplasm | 0% | 0% | NS |
| Malignant | 0.9% | 2.2% | NS |
| Nondiagnostic/inadequate | 44% (±0.06) | 17.2 (±0.04) | <0.005 |
NS, not significant.
Given as percentage of the total. For both groups, data for nondiagnostic samples are given as percentage±standard error.
Our sample appears to be homogeneous. No differences were found in age, sex, plasma TSH levels, or nodule size between the two groups (Table 1). The diagnostic criteria and the pathologists who applied them did not change during the study, and all FNAs were performed by the same person. However, patients were not randomly assigned to the groups: all FNAs performed before a given date were included in one of the groups (with no needle washing), while those performed after that date were assigned to the other group (with needle washing). This represents a bias that may have conditioned the results. We suggest the conduct of further studies with random distribution of the sample.
The prevalence of nondiagnostic FNA in the group of patients without washing was markedly higher than that reported in the medical literature before 2007. In fact, this was the reason for the reported change in the procedure. The prevalence of nondiagnostic FNA has probably increased since implementation of the Bethesda criteria in pathology departments, because diagnostic categories are much more precise and better established than before, when an often abstract terminology was used for inadequate material.
We considered the possibility that the differences found actually resulted from the maturation of a technique newly implemented at our department. We think this is unlikely, because the person who implemented the procedure had already been performing it in the same way for more than a decade, and the pathologists of our hospital had been analyzing thyroid cytological samples long before the endocrinology department started to send them its samples. The possibility that the difference seen was due to differences in types of conditions cannot be dismissed. A study comparing the diagnoses made on slide smears to those made with washing of the material remaining in the needle would be appropriate.
The medical literature usually gives a similar description of the standard FNA procedure, excluding cytocentrifugation of the material remaining from needle washing in a ThinPrep® solution, a procedure which is very helpful for assessing cell nuclei and an alternative procedure for the detection of a greater number of cell groups, thus increasing the chance of making a diagnosis and classifying the sample into one of the categories recommended by the Bethesda criteria.
The collection and subsequent processing of the material remaining in the needle used to perform FNA decreased the prevalence of nondiagnostic punctures in our patients very significantly. Such prevalence is now similar to that reported for punctures prior to the implementation of the Bethesda criteria. In addition, the procedure described prevents contamination with blood from the sample (which is common in thyroid punctures) and allows for the performance of immunohistochemical techniques. We recommend that, in all thyroid FNAs, the material remaining in the needle be collected in this way.
Conflicts of interestThe authors state that they have no conflicts of interest.
Please cite this article as: Penín Álvarez M, et al. El lavado de la aguja aumenta la rentabilidad diagnóstica de la punción-aspiración con aguja fina de tiroides. Endocrinol Nutr. 2013;60:115–18.