Many reports have supported the relationship between high preoperative TSH levels and risk of thyroid cancer in nodular thyroid disease (NTD).
ObjectivesWe investigated whether TSH levels are related to the risk of differentiated thyroid carcinoma (DTC) in patients who have undergone total thyroidectomy for NTD. The relationship between TSH and size of malignant nodule was investigated. Finally, we assessed whether TSH levels are related to DTC and presence of additional benign nodules.
Patients and methodsA retrospective study of 980 patients was conducted. Variables included age at diagnosis, TSH level, nodule size, gender, final histology (benign versus DTC), and type of malignancy.
ResultsMalignancy was present in 261 (26.6%) patients. These patients had higher median TSH levels as compared to those with no malignancy (1.61mU/L (0.9–2.5) versus 0.9mU/L (0.3–1.6); p-value<0.001). TSH was higher in patients with DTC in whom the largest nodule was malignant than in patients in whom the largest nodule was benign (1.80mU/L (1.1–2.6) versus 1.38mU/L (0.7–2.1) respectively; p-value=0.025). A significant correlation was seen between malignant nodule size and TSH level, but not between TSH levels and size of the largest benign nodule.
ConclusionsOur study supported an association between preoperative TSH levels and risk of DTC in patients with NTD. There was also a direct relationship between malignant nodule size and TSH levels. By contrast, no relationship was found between the size of benign nodules and TSH levels.
Un gran número de artículos han confirmado la relación entre los niveles elevados de TSH preoperatoria y el riesgo de cáncer de tiroides en la enfermedad nodular tiroidea (ENT).
ObjetivosAnalizamos si los valores de TSH preoperatoria se relacionan con el riesgo de cáncer diferenciado de tiroides (CDT) en pacientes tiroidectomizados por ENT. Además, investigamos la relación entre TSH y el tamaño del nódulo maligno. Finalmente, valoramos si la TSH se relaciona con la presencia de CDT y con la presencia de nódulos benignos adicionales.
Pacientes y métodosSe estudiaron retrospectivamente 980 pacientes. Las variables consideradas fueron: edad al diagnóstico, sexo, valor de TSH, tamaño del nódulo, histología definitiva y tipo de CDT.
ResultadosEn 261 (26,6%) casos el diagnóstico fue de CDT. Estos pacientes tenían niveles más elevados de TSH que los pacientes con histología benigna (mediana de 1,61 mU/l [0,9-2,5] versus 0,9 mU/l [0,3-1,6]; p<0,001). La TSH fue más elevada en pacientes con CDT en los que el nódulo dominante fue maligno en relación con los que el nódulo dominante fue benigno (1,80 mU/l [1,1-2,6] versus 1,38 mU/l [0,7-2,1], p=0,025). Hubo una correlación significativa entre el tamaño del nódulo maligno y la TSH, pero no entre la TSH y el tamaño del nódulo benigno dominante.
ConclusionesConfirmamos la asociación entre los niveles preoperatorios de TSH y el riesgo de CDT en la ENT. Describimos una relación directa entre el tamaño del nódulo maligno y los valores de TSH. Esta relación no se confirma para el tamaño de los nódulos benignos adicionales.
It has recently been reported that a higher preoperative TSH concentration is associated with an increased risk of differentiated thyroid carcinoma (DTC) in patients with nodular thyroid disease (NTD). Since the publication of Boelaert et al.1 in 2006, the relationship between TSH and risk of DTC has been confirmed in several papers, a review and a systematic review and meta-analysis.2,3 McLeod et al.3 have calculated that the likelihood of DTC is three times greater for a subject with a serum TSH level of 4mU/L than for a subject with a serum TSH level of 0mU/L. The correlation of TSH with DTC risk has recently been verified for pediatric patients as well.4 Moreover, TSH levels have also been associated with a more advanced stage of DTC.5–7 It has therefore been proposed that serum TSH measurement could be used to help to predict the likelihood of thyroid cancer in patients with NTD.
To date, it is not clear whether TSH is involved in the development or progression of this disease, or possibly both. Experimental data suggest that the TSH signaling pathway may predispose thyroid cells to BRAF-induced transformation.8 Alternatively, some studies have suggested that TSH is not likely to be involved in the de novo oncogenesis of papillary thyroid carcinoma (PTC) and that this hormone might play a role in the progression and growth of preexisting tumors.2,9 However, the existence of a possible relationship between tumor size and TSH level has not yet been determined. The few studies that have analyzed the association of TSH levels with papillary thyroid microcarcinomas (PTC with a diameter equal to or smaller than 10mm) have arrived to conflicting conclusions.6,9–13 Moreover, many patients with DTC have additional benign nodules in their thyroid, and the influence of those nodules on the TSH concentration has not yet been determined.
The present study has three objectives. We first wanted to investigate whether TSH is related to the risk for DTC in a large cohort of patients who have undergone total thyroidectomy for NTD. Second, we wanted to determine whether TSH is related to the size of DTCs in patients with the diagnosis of malignancy. Finally, we wanted to test whether TSH levels were related with DTC and/or with additional benign nodules.
Material and methodsThis is a retrospectively study. Between January 2006 and December 2012, 1696 patients without previous thyroid surgery underwent thyroidectomy. Thyroidectomy was prescribed for patients with malignant, suspicious, or repetitive indeterminate nodules according to fine needle aspiration biopsy (FNAB) results. Moreover, surgery was indicated for some forms of hyperthyroidism, benign disease with local symptoms or esthetic reasons. A total of 716 patients were excluded from the study for the following reasons: non-total thyroidectomy (n=483), Graves disease (n=27), Hashimoto disease (n=59), amiodarone-induced thyrotoxicosis (n=5), malignancy other than DTC in final histology (n=36), and incomplete data (n=106, lack of TSH values, no data about the nodule size, etc.). This resulted in a study population of 980 patients with total thyroidectomy for NTD. All patients had a solitary nodule or a multinodular goiter detected by clinical examination, ultrasound scan (US), or both. Preoperatively, an US confirmed NTD in all cases. A FNAB was performed for thyroid nodules>1cm and for nodules<1cm with suspicious US features. All patients had serum TSH levels measured within 1 year before surgery using an automated immunochemiluminescent assay (Immulite 2500; Siemens, Los Angeles, CA, USA). The normal range was 0.4–4.0mU/L. Total thyroidectomy was prescribed in all cases. Therefore, a diagnosis of DTC or benign thyroid disease was based on surgical pathologic results.
Statistical analysisData were summarized using the median (interquartile range) for continuous variables and the proportion or frequency for categorical variables. Continuous variables included the age at intervention, TSH level and nodule size. Categorical variables included gender, final histology (benign versus DTC), and type of malignancy (PTC, follicular thyroid carcinoma, or poorly differentiated thyroid carcinoma). The nodule size was evaluated as both a continuous variable and a categorical variable; thus, samples were either DTC with a diameter equal to or smaller than 10mm, or not. Patients with DTC and additional nodules were subdivided into two categories depending on whether the largest nodule was malignant or not. A chi-square test was used for the comparison of frequencies. A comparison between continuous variables was performed with the nonparametric Mann–Whitney-U-test or the Kruskall–Wallis test, when more than two groups were involved. A Conover–Inman post hoc test for multiple pairwise comparisons between groups was performed following a significant Kruskall–Wallis test. A Pearson correlation coefficient was calculated for the relationship between TSH levels and nodule size. A ROC analysis was performed for TSH levels and the presence of malignancy. p-Values≤0.05 were considered statistically significant.
ResultsThe final study cohort of 980 patients consisted of 815 (83.2%) females and 165 (16.8%) males with a median age of 57 (44–66) years. The final pathology data showed no evidence of malignancy in 719 (73.4%) patients, whereas DTCs were found in the remaining 261 (26.6%) cases. The neoplasm was incidentally discovered in 113 (43.3%) patients. We defined incidental diagnosis as DTC diagnosed at final histology in a patient in whom surgery was perfomed for a benign thyroid disease. The histological diagnoses for malignant cases were papillary thyroid carcinoma (n=228), follicular thyroid carcinoma (n=27) and poorly differentiated thyroid carcinoma (n=6). All malignant nodules less than 1cm were PTC, namely papillary thyroid microcarcinomas (PTMC). A total of 106 (45.9%) patients were classified as PTMC, whereas the remaining 155 (54.1%) were non-PTMC. The median age at the time of diagnosis was 59 years (47–67) in benign cases and 52 years (39–62) for patients with malignancies (p-value<0.001).
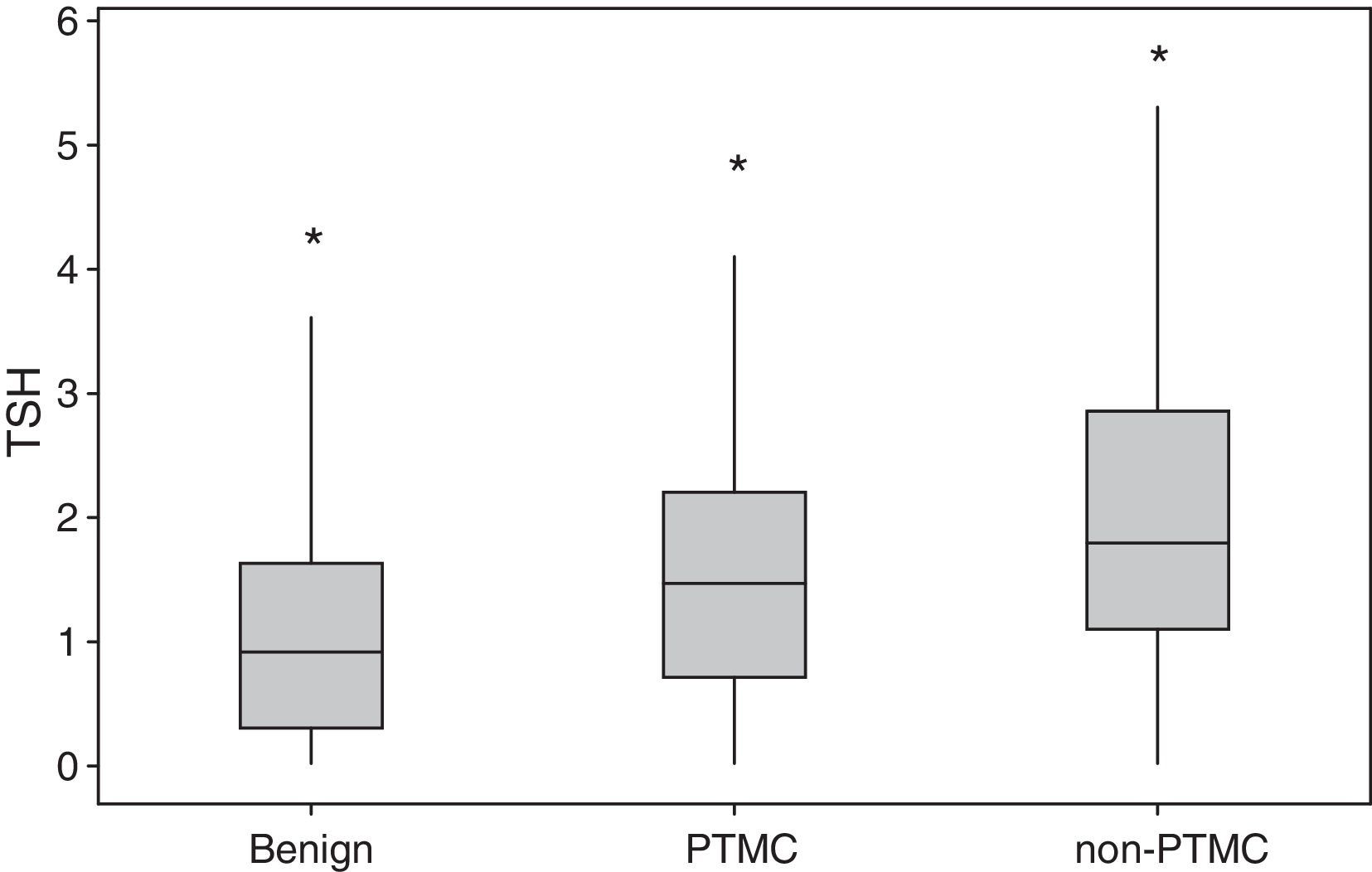
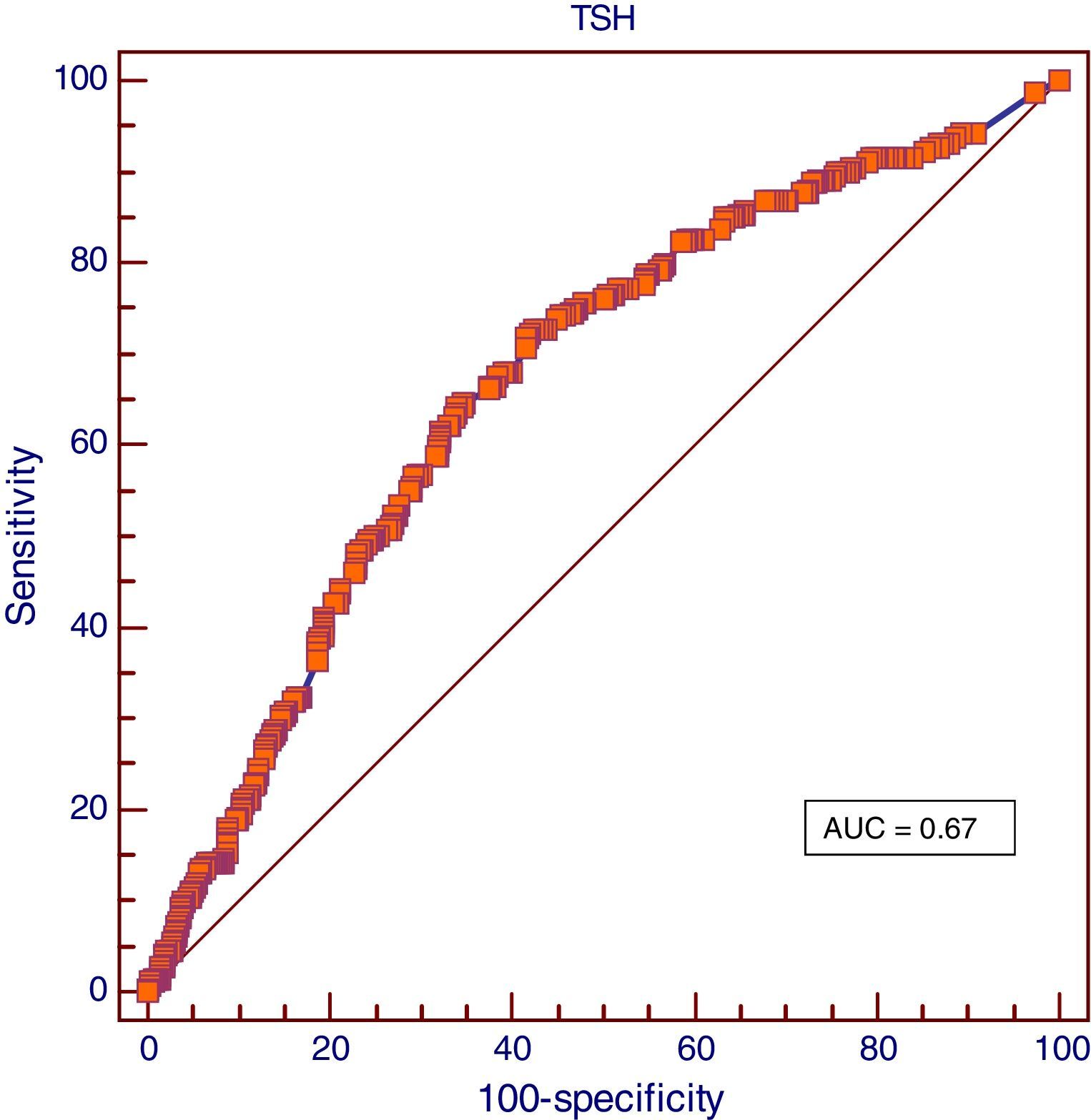
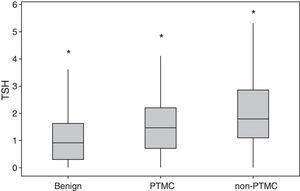
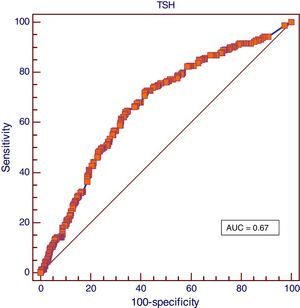
Overall, patients with malignancy had higher median values of TSH than did patients with benignancy (1.61mU/L (0.9–2.5) versus 0.9mU/L (0.3–1.6), respectively; p-value<0.001). The difference remained significant after adjusting for age. Among the set of patients with malignant nodules, the median TSH level was 1.47mU/L (0.7–2.2) in subjects with PTMC and 1.80mU/L (1.1–2.8) in patients with non-PTMC (p-value=0.017). The median TSH levels for the benign, PTMC, and non-PTCM groups were significantly different (p-value<0.001) (Fig. 1), and pairwise comparisons between the three groups also revealed significant differences. The ROC analysis showed a TSH cut off point of 1.08mU/L to differentiate benign from malignant NTD with a sensitivity of 72% and a specificity of 58% and with an area under the curve (AUC) of 0.67 (Fig. 2).
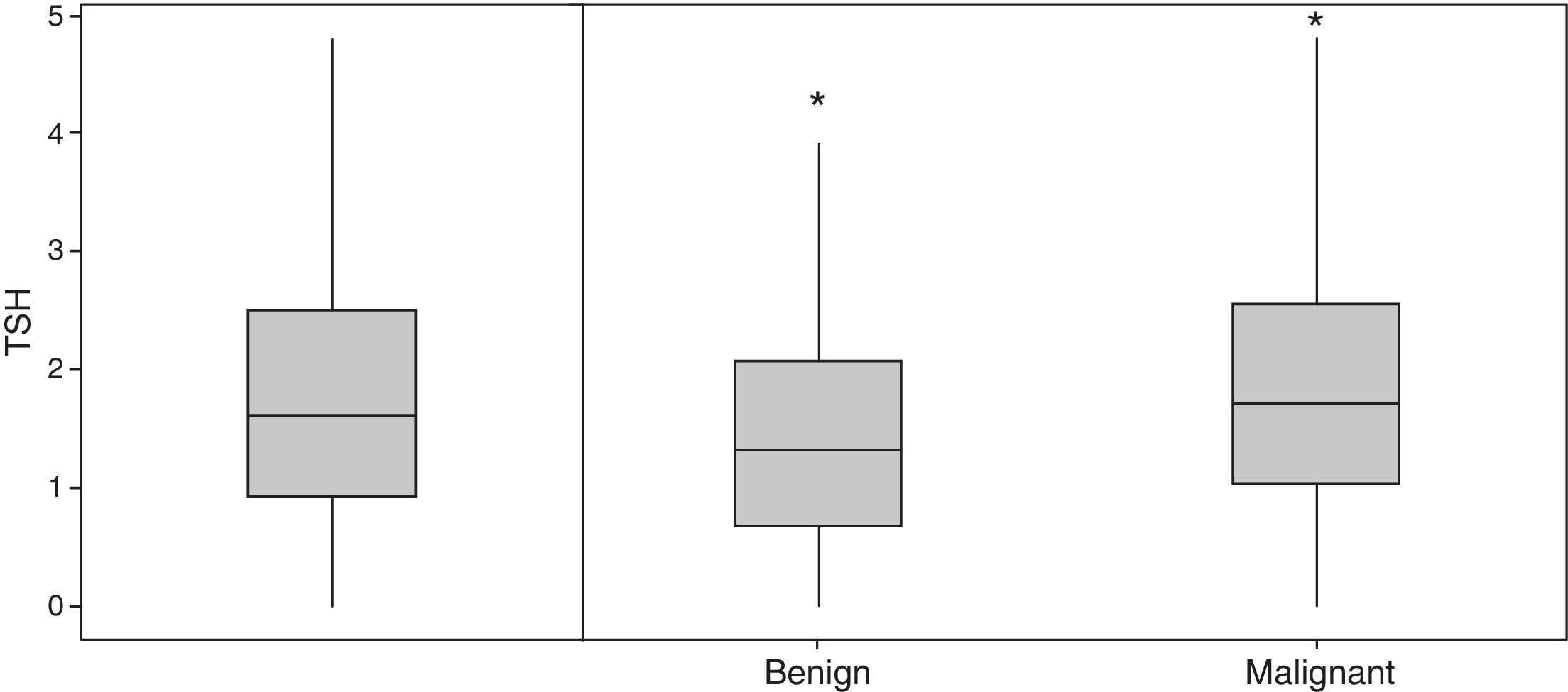
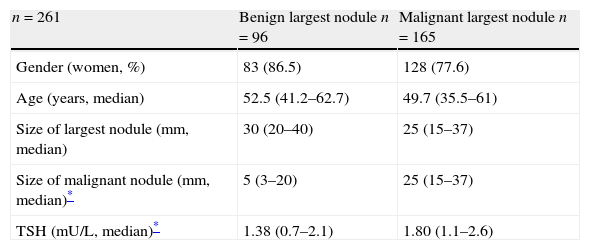
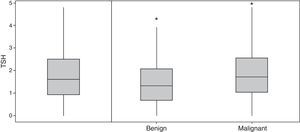
Characteristics of patients with DTC according to whether the largest nodule was benign or malignant are summarized in Table 1. In 165 patients (63.2%) with DTC, the largest nodule was malignant. The median TSH was higher in this group of subjects than in patients for whom the largest nodule was benign (1.80mU/L (1.1–2.6) versus 1.38mU/L (0.7–2.1), respectively; p-value=0.025) (Fig. 3). Spearman's correlation showed a moderate but significant correlation between the size of the malignant nodule and the level of TSH (Rho=0.15; p-value=0.012). However, there was no significant association between TSH and the size of largest nodule (either benign or malignant) (Rho=−0.03; p-value=0.59) or the size of largest nodule when the largest nodule was benign (Rho=0.10; p-value=0.26).
Characteristics of patients with differentiated thyroid carcinoma according to whether largest nodule was benign or malignant.
| n=261 | Benign largest nodule n=96 | Malignant largest nodule n=165 |
| Gender (women, %) | 83 (86.5) | 128 (77.6) |
| Age (years, median) | 52.5 (41.2–62.7) | 49.7 (35.5–61) |
| Size of largest nodule (mm, median) | 30 (20–40) | 25 (15–37) |
| Size of malignant nodule (mm, median)* | 5 (3–20) | 25 (15–37) |
| TSH (mU/L, median)* | 1.38 (0.7–2.1) | 1.80 (1.1–2.6) |
In the present study we have confirmed the relationship between preoperative TSH levels and the likelihood of malignancy in patients with NTD. It is not currently clear whether TSH is involved in the development or progression of DTC, or both. Experimental data suggest that the TSH signaling pathway may predispose thyroid cells to BRAF-induced transformation.8 Alternatively, some authors have suggested that TSH is only involved in the progression and growth of pre-existing tumors.2,9 It has been hypothesized that patients with tiny tumors, such as papillary thyroid microcarcinoma, should have higher TSH values than subjects without DTC if TSH exerts any influence on the origin of PTC. In this regard, PTMC is thought to be an early stage in the development of PTC. To date, six studies have analyzed the association of TSH concentration with PTMC. In a series of reports by Haymart et al.6, the authors found that an escalating risk of malignancy persisted with higher TSH levels until the hormone reached ≥5mU/L in the subset of tumors that were <1cm. Moon et al.11 also showed that TSH concentration was an independent risk factor for PTMC in euthyroid patients. Alternatively, Gerspacher et al.10 compared a cohort of patients with PTMC and a control group of patients whose thyroid glands had been removed as a treatment for medullary thyroid carcinoma and found no significant differences in TSH levels. Also, Shi et al.12 and Negro et al.9 found no preoperative TSH differences between patients with PTMC and patients with NTD without malignancies. Finally, in a previous study, we observed an incremental increase in tumor sizes as a function of an increase in TSH levels.13 Thus, the TSH level gradually increases, starting with benign cases, progressing to PTMCs, and then to PTCs of larger size. Though an incremental increase in TSH levels across the three conditions was evident, differences were only significant between benign cases and PTC>1cm. The present study evaluated a larger number of cases, and we found that TSH differences were significant not only between benign and malignant cases, but also between benign cases and PTMCs and PTMCs and non-PTMCs.
Many patients with DTC also have other benign nodules in their thyroid. In some cases, the cancerous nodule was not the largest. It has been suggested that additional nodules could modify the level of TSH. Fiore et al.5 have postulated that benign nodules become progressively more autonomous with age. Such nodules may reduce TSH levels and thus reduce the influence of TSH on the development and/or growth of thyroid cancer. In our study, DTC was not the largest nodule in 97 (37%) cases. Interestingly, we found that TSH levels were significantly associated with the size of the malignant nodule, but not with either the predominant nodule or the dominant benign nodule. Moreover, TSH levels were higher in those patients for whom the predominant nodule was DTC than in patients for whom the predominant nodule was benign. All of these findings suggest that TSH levels are mainly related with the size of the malignant nodule, even though additional concomitant benign nodules could modulate that association.
Notably, it has recently been reported in a genome-wide association study that TSH levels are associated with the presence of 22 gene variants.14 Some of these variants also conferred risk for thyroid cancer. Intriguingly, the at-risk allele was associated with lower serum levels of TSH for all the variants that confer risk for cancer. The authors hypothesized that a low level of TSH may suppress differentiation of the thyroid epithelium, causing a predisposition to malignant transformation. In this regard, several authors have reported an association between hyperfunctioning thyroid nodules and thyroid cancer risk.15,16 In a recent meta-analysis, Negro et al.17 did not find any significant difference in the risk of incidental thyroid cancer in patients with toxic versus non-toxic multinodular goiter.
Finally, there are some limitations in the study. TSH determination was performed only once and within one year before thyroidectomy. It is not known whether fluctuating TSH values along time could influence the cancer evolution. Moreover, the clinical impact of the relation between TSH levels and cancer risk seems very limited. Although most studies confirm the relationship, the application in an individual patient with the aim of deciding the type of surgical intervention is of little use. However, the TSH value, together with those factors that have classically been accepted as cancer risk markers, can improve the correct assessment of the patient.
In summary, we have confirmed the association between preoperative TSH levels and the risk of DTC in patients with NTD, and we have found a direct relationship between the size of the malignant nodule and TSH. Furthermore, the presence of benign nodules was not related with TSH levels, but could modify the intensity of the relationship between malignant nodule size and TSH levels. The controversial data published so far demonstrates that the relation between TSH levels and the risk of thyroid cancer remains poorly understood. Further basic and clinical studies will be required to determine the role of TSH in thyroid cancer origin and development.
Conflict of interestThe authors declare that they have no conflict of interest.