Rhinomucormycosis, an opportunistic infection caused by fungi of the Phycomycetes class, usually occurs in diabetic patients with poor metabolic control and in those with organ transplant, cancer, neutropenia, or immunodeficiency.1–3 The main pathogens belong to the species Rhizomucor, Rhizopus, Absidia, and Mucor. The most common presentation is rhino-orbital-cerebral mucormycosis. We report the case of a patient with oral mucormycosis and type 1 diabetes mellitus (DM).
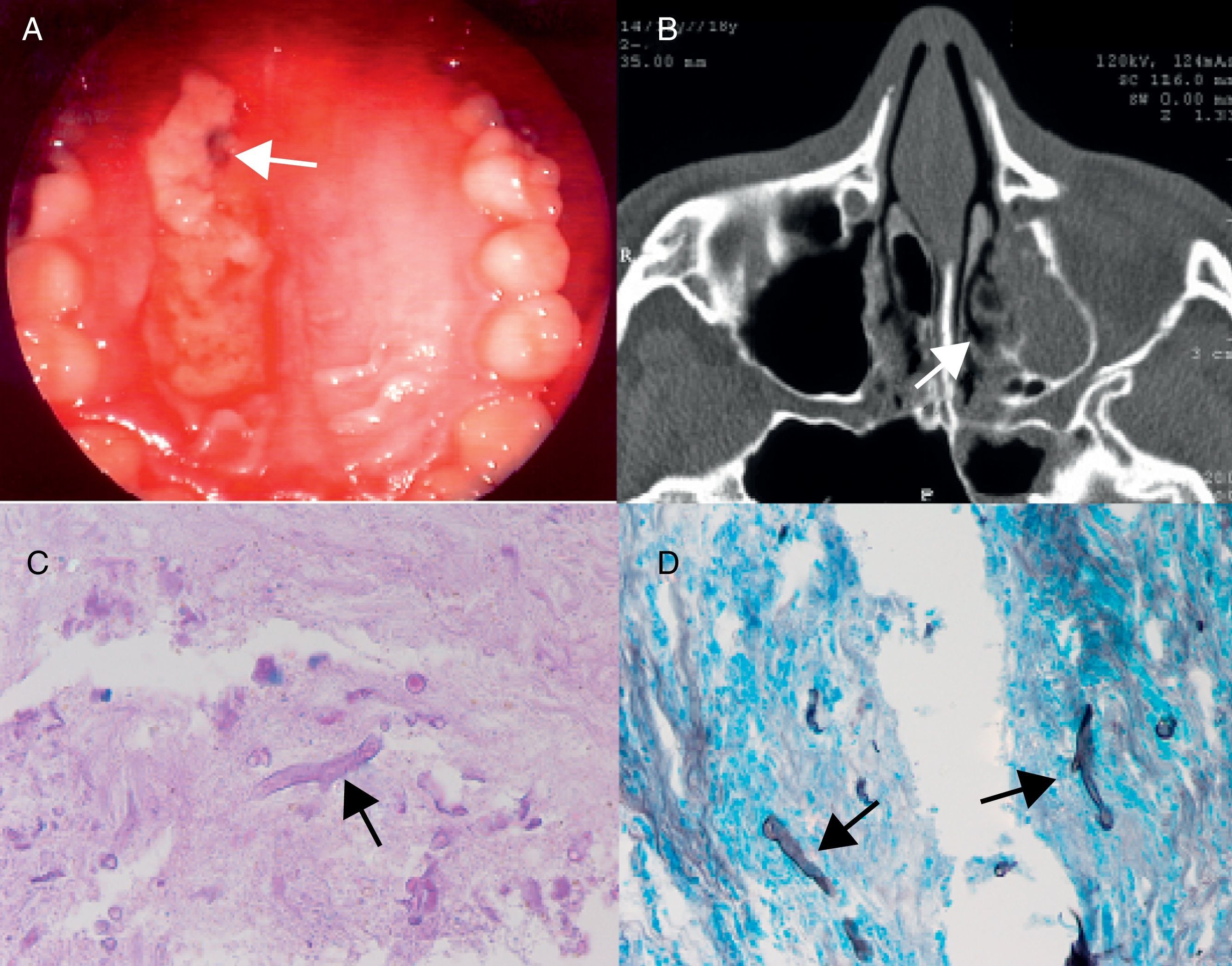
The patient was a 22-year-old female diagnosed with primary hypothyroidism and type DM since six years of age. She had been admitted to hospital several times for diabetic ketoacidosis (DKA), and her most recent glycosylated hemoglobin value was 14%. Her treatment included insulin glargine 29IU/day, insulin aspart 6IU with each meal, and levothyroxine 50mcg/day. During the previous week she had experienced malaise, headache, and decreased sensitivity in the left side of the face (territory of the maxillary branch of the 7th cranial nerve). Physical examination revealed hypesthesia in the above region and lysis with sphacelation at palate level (Fig. 1).
Photograph A: the soft palate with lysis and sphacelation in the palatal region (white arrow). Photograph B: computed tomography showing partial occupation of the basal and lateral region of left maxillary sinus with no air-fluid levels. Photographs C and D: the arrow shows the image of the thick fungus consistent with Mucor in PAS staining (C) and with the Grocott–Gomori technique (D).
No changes were found in the complete blood count, kidney function, thyroid function, venous blood gases, and microalbuminuria. Blood glucose and glycosylated hemoglobin levels were 107mg/dL and 10.7% respectively. Computed tomography (CT) of the paranasal sinuses revealed partial occupation of the basal and lateral region of the left maxillary sinus without air-fluid levels, with thinning and dehiscence of the alveolar recess and soft tissue occupation (Fig. 1).
The patient underwent nasosinusal endoscopic surgery consisting of uncinectomy, anterior ethmoidectomy, and maxillary antrostomy. Because of the presence of infected tissue and necrosis at the middle septal region, debridement was performed up to the healthy bone area.
A pathological study found fragments of nasosinusal mucosa with mixed inflammatory infiltrate (lymphoplasmacytic proliferation and polymorphonuclear white blood cells) and fibrosis with granulomatous reaction with multinucleated giant cells. PAS and Grocott stains revealed the presence of mitotic figures consistent with Mucor (Fig. 1). Based on these results, antibiotic treatment was started with intravenous amphotericin B 50mg/12h for two weeks and insulin treatment was intensified, which improved blood glucose control. Three months later, a CT scan of the paranasal sinuses showed lesion improvement and a virtually complete filling of the left maxillary sinus with mild sclerosis of its bone walls.
Infection by fungi belonging to the order of Mucorales, first described by Paltauf,5 is uncommon in the general population, but exposure to these fungi is common. In humans, infection is acquired by spore inhalation,5 and once colonization has occurred, the fungi grow along the arterial internal elastic lamina, enter the endothelium, and cause thrombosis, infarction, and tissue necrosis.6 High glucose levels alter phagocytosis and decrease neutrophil chemotaxis, promoting fungal growth. Poorly controlled DM is therefore considered a risk factor. Acidosis impairs iron binding to transferrin, increases free iron, and promotes fungal growth. DKA therefore triggers this infection.6 Type 1 DM has been estimated to increase 4-fold the risk for zygomycosis, while type 2 DM increases the risk 6-fold.3 In a review of 929 cases of zygomycosis,3 36% of patients had diabetes. Sinus involvement consisting of paranasal sinus, rhino-cerebral, or sino-orbital infection accounted for the majority of infections in patients with DM (66%).3 In another reported series of 34 patients with rhino-orbital-cerebral mucormycosis, 88.2% had poorly controlled diabetes, and 53.3% of these had DKA.7
Dissemination occurs due to the invasive nature of Mucorales. There are different clinical forms of the infection, which may affect the nasal region, lung, gastrointestinal tract, and central nervous system (CNS). Rhinocerebral mucormycosis, starting with the involvement of the paranasal sinuses, oral mucosa, and palate is the most common. Clinically, palatal hypesthesia, nasal obstruction, rhinorrhea, or epistaxis occur. When the infection extends to the orbital and periorbital regions, ophthalmoplegia, ptosis, mydriasis, hypesthesia, or hyperesthesia may occur in the different distributions of branches of the 5th cranial nerve. Mucormycosis may affect other cranial nerves, and when it reaches the cavernous sinus, it causes thrombosis and compromises the 3rd, 4th, and 6th cranial nerves. If the patient has changes in the higher mental functions, cerebral extension, which may cause coma and death, is assumed.4 The reported patient had the paranasal sinuses affected with involvement of the 5th cranial nerve, but without orbital or CNS damage. This type of localization with involvement of the paranasal sinuses alone is uncommon, probably because diagnosis is made at more advanced stages of infection.
The clinical course and progression of the disease are fulminant due to rapid fungal growth and bone destruction. Early treatment therefore improves prognosis. Infection should be suspected in any patient with risk factors and signs and symptoms in the nostrils, paranasal sinuses, orbital region, and CNS.3,4 Diagnosis is confirmed by histological and microbiological studies. The Grocott–Gomori stain is the most effective for identifying fungi, but the hematoxylin–eosin or periodic acid-Schiff stains are also helpful.1,4 Blood vessel invasion and the presence of a neutrophilic infiltrate in necrotic tissue are characteristic of mucormycosis.4 Tissue and blood cultures fail to show the presence of Mucorales, and are therefore not used as single diagnostic tests.4 In addition, identification of the saprophyte fungus does not prove that infection has occurred. CT and MRI are useful for the extension study because they reveal the involvement of the paranasal sinuses, orbits, and CSN. Bone lesions occur in late infection stages.
Successful treatment is based on control of the underlying disease, extensive surgical resection of the infection site and/or debridement of necrotic tissue, and medical treatment with antifungals. The overall mortality rate is 43% when the rhinocerebral region is involved, but only 13% if only sinusitis exists. Disseminated disease, infection by Cunninghamella bertholletiae and renal failure worsen prognosis.
In DM, blood glucose and acidosis correction are the basis of treatment. Surgical procedure depends on the extent of the disease, but drainage of the paranasal sinuses and the removal of infected tissue should be ensured. Amphotericin B, at doses ranging from 1.0 to 1.5mg/kg/day, is the drug of choice because of its superior efficacy compared to other treatments. Treatment duration is 3–6 weeks. The reported adverse effects include hypokalemia, fever, dyspnea, tachycardia, and abdominal pain. Posaconazole, a new drug, is an alternative option that may be used alone or combined with amphotericin B.6,7 The use of hematopoietic stimulating factors and hyperbaric oxygen to improve angiogenesis may be beneficial, but no adequate data are available to recommend their use.4,8 The mortality rate of this infection decreased after the advent of amphotericin, from 84% in 1950s to 37% in 1990s. The combination of surgery and antifungal therapy achieves 79% survival.3,9 The most significant prognostic factor is delayed diagnosis.
The high mortality rate in patients with mucormycosis requires a high degree of suspicion for early diagnosis and treatment in early disease stages.
Please cite this article as: Manrique K, et al. Rinomucormicosis y diabetes mellitus tipo 1. Endocrinol Nutr. 2013;60:149–51.