Obesity is one of the main problems for our Public Health System today. The prevalence of obesity and overweight in adults in Spain is 22.9% and 39.4% respectively.1 Obesity causes 1 of every 13 deaths in Europe and it is the second cause of evitable mortality behind smoking.2 The treatment of obesity always includes hypocaloric diets, exercise, changes in one's way of life and regular medical visits.3 If the results after the previous treatments are not good, the pharmacological treatments are limited in Europe,4 so that, patients with body mass index (BMI)≥35kg/m2 may be referred to a Hospital Clinic. In these patients, we can consider a very-low calorie diet and bariatric surgery.5
It is known that referrals to a Hospital Clinic from Primary Care are not homogeneous and, one important factor of this is the need to travel to another city to be attended.6 The aim of our study was to know if the need to travel to another city to be attended in a Hospital Clinic for obesity may affect to the adequacy of referrals from Primary Care.
52213 inhabitants located in the southeast of Castilla-La Mancha are attended in our hospital. 25024 inhabitants live in the same city where the hospital in located, but 27389 live in other cities and these people need to travel between 50 and 60km to be attended in our Hospital. The study was based on a retrospective design and the following variables were collected: age (years), BMI (kg/m2), type of obesity, adequacy of referrals (BMI≥35kg/m2), and need to travel to be attended (a patient who lives in the same city where the Hospital is located or in a different city) for each of the patients referred because of their obesity or overweight from Primary Care to our Hospital Clinic in first visit in 2014.
Qualitative variables were expressed as absolute and relative frequency. Quantitative variables were expressed as mean, standard deviation, and range. The T-Student test was used to compare quantitative variables and the Chi-square test to compare proportions between two groups (same city versus different cities). A p value<0.05 was considered statistically significant.
The study included 131 patients who were referred from Primary Care for not-complicated obesity, who were attended in less than 30 days in our Hospital in their first visit in 2014. Patients who were referred from Hospital Care and patients with complications related to obesity are not included in this study.
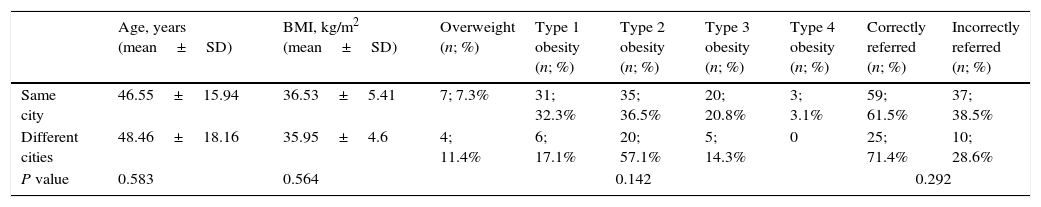
The clinical characteristics of all subjects are shown in Table 1. The age mean value was 47±16 years [14–80] and their BMI was 36.4±5.2kg/m2 [25.3–51.5]. 11 patients (8.4%) suffered from overweight; 37 patients (28.2%) suffered from type 1 obesity; 55 patients (41.9%) suffered from type 2 obesity; 25 patients suffered from type 3 obesity; and 3 patients (2.3%) suffered from type 4 obesity. 96 patients (73.3%) live in the same city where the Hospital is located (1 patient of every 260 inhabitants) and 35 patients (26.7%) live in different cities (1 patient of every 782 inhabitants). 83 patients (64.1%) had been referred correctly (BMI≥35kg/m2). The study failed to show statistically differences between groups (same city vs different cities) regarding age, BMI, type of obesity or adequacy of referrals (61.5% in the same city vs 71.4% in different cities). The fact of not finding any statistically significant difference despite of the big difference in the number of referrals (1 patient of every 782 inhabitants versus 1 patient of every 260 inhabitants) leads us to two important conclusions.
Comparison of clinical features between patients who live in the same city where the Hospital is located and patients who live in different cities.
| Age, years (mean±SD) | BMI, kg/m2 (mean±SD) | Overweight (n; %) | Type 1 obesity (n; %) | Type 2 obesity (n; %) | Type 3 obesity (n; %) | Type 4 obesity (n; %) | Correctly referred (n; %) | Incorrectly referred (n; %) | |
|---|---|---|---|---|---|---|---|---|---|
| Same city | 46.55±15.94 | 36.53±5.41 | 7; 7.3% | 31; 32.3% | 35; 36.5% | 20; 20.8% | 3; 3.1% | 59; 61.5% | 37; 38.5% |
| Different cities | 48.46±18.16 | 35.95±4.6 | 4; 11.4% | 6; 17.1% | 20; 57.1% | 5; 14.3% | 0 | 25; 71.4% | 10; 28.6% |
| P value | 0.583 | 0.564 | 0.142 | 0.292 | |||||
The first conclusion is that we have to find out a clinical pathway to reduce the number of patients incorrectly referred (35.9% in our study) and we have to look for new ways (tele-assistance, for example) to assist patients who cannot be attended in our hospital. With the use of this clinical pathway and new ways to assist, we have to improve the quality and accessibility of our attention to these patients.
Conflict of interestAll authors of this manuscript state that there is no conflict of interest in relation to the same.